Petra Klinge’s talk on tethered cord syndrome blew my mind. It‘s given me a deeper understanding of how tethered cord syndrome might play a fundamental role in the patholophysiology and symptoms of a subset of #MECFS and #EDS patients. THREAD [1] https://youtu.be/zpSXSMPiMI8 ">https://youtu.be/zpSXSMPiM...
Tethered cord syndrome is a cluster of symptoms that develop when the filum terminale, a string of connective tissue that links the end of your spinal cord to your sacrum, is either inappropriately attached to your spinal canal or is too tight. [2] https://me-pedia.org/wiki/Tethered_cord_syndrome">https://me-pedia.org/wiki/Teth...
This tethering exerts a downward force on your spinal cord. It’s why some neurosurgeons think tethered cord might predispose people to developing craniocervical instability/atlantoaxial instability (CCI/AAI) or symptomatic Chiari later in life. [3]
My neurosurgeon looked at 250 patients (primarily patients with #EDS) who had craniocervical fusions for CCI between 2012 and 2018. He found that 30% required a tethered cord release surgery either before or after their craniocervical fusions. (Unpublished data.) [4]
According to @jeff_says_that, 85% of the 15 #MECFS patients who have so far had craniocervical fusions in our Facebook group were subsequently diagnosed with tethered cord syndrome. This includes me, @julierehmeyer and @jeff_says_that. [5]
. @jeff_says_that suspects that when compared to other patient populations, a higher percentage of #MECFS patients will turn out to have concurrent CCI and tethered cord syndrome. I agree. (It goes without saying that n=15 is still to small to know.) [6]
What does this have to do with #MECFS? I think tethered cord syndrome explains a lot of the symptoms that began one year after my viral onset, including migrating leg pain, asymmetric leg weakness, and severe crashing after physical exertion. [7] https://link.medium.com/vY5tDGymA7 ">https://link.medium.com/vY5tDGymA...
I think I have had a tethered cord my whole life, and that it was the *most important risk factor* for my developing #MECFS after a viral infection. [8]
My whole life, the soles of my feet have been less sensitive than they should be, but also incredibly ticklish. As a kid, I was a late bed wetter. I hated running. [9]
I peed more often and with greater urgency than I should––a problem that could be particularly bad on long hikes. And as I grew, I developed a head forward posture with hunched shoulders and kyphosis in my thoracic spine. [10]
As a teenager, my mom constantly told me to stand up straight. I had no idea anything was wrong. At the time, these symptoms were not life-limiting. And how could I know there was something “wrong” with my body if it was the only body I had ever lived in? [11]
In her talk, Dr. Klinge presents the symptoms and outcomes of 113 patients with occult tethered cord (OTC). OTC is tethered cord that *does not appear on a lumbar MRI.* [12]
Tethered cord is generally considered to be a genetic or developmental condition. (I suspect there may also be important environmental factors that contribute to it becoming symptomatic or not.) Key is that it presents very differently in infants, children, and adults. [13]
It also tends to worsen over time, as you grow. This may be why many of us with TC don& #39;t develop life-limiting symptoms until our 20s or 30s, even if looking back, there were signs our whole life. Some don& #39;t develop overt symptoms until their 50s or 60s. [14]
Here are some of the common symptoms of tethered cord syndrome, pre/post tethered cord release surgery. I marked the ones I use to have in red. (More on symptoms here: https://www.me-pedia.org/wiki/Tethered_cord_syndrome)">https://www.me-pedia.org/wiki/Teth... [15]
In addition to CCI and Chiari, it is often comorbid with #EDS, dysautonomia, #POTS, and #MCAS. However, many, many cases are being missed. Klinge& #39;s talk helps explain why.
In fact, if we are relying primarily on MRIs, we are probably diagnosing tethered cord ALL WRONG. [16]
In fact, if we are relying primarily on MRIs, we are probably diagnosing tethered cord ALL WRONG. [16]
First, there is a major imaging problem. Typically, a tethered cord is diagnosed if the conus, the terminal end of the spinal cord, lies below L2, the second vertebra of the lumbar spine. If the conus is at or above L2, a radiologist will consider your lumbar MRI normal. [17]
Klinge found *no statistically significant differences* in the level of the conus between her surgical patients and healthy controls. This is mindblowing. [18]
While only ppl with major symptoms are ever referred for surgery, this means:
– many ppl w/ low conuses are “healthy”
– only symptomatic ppl w/ low conuses get diagnosed
– symptomatic ppl w/o low conuses are generally left to get worse until they are bedridden, like I was. [19]
– many ppl w/ low conuses are “healthy”
– only symptomatic ppl w/ low conuses get diagnosed
– symptomatic ppl w/o low conuses are generally left to get worse until they are bedridden, like I was. [19]
Fat is another problem. A fatty filum is a major radiological sign of tethered cord that does not appear with OTC. Some of Klinge’s OTC patients actually DID have fat. It might have appeared on one MRI, but not another, perhaps due to CSF pulsation...[20]
...a signifcant proportion of Klinge’s “occult” tethered cord syndrome patients did not have fatty filums on MRI. However, when Klinge examined the filum tissue itself, she did find fat in a large % of patients’ filums. [21]
The results of Klinge’s histology studies of her 113 occult tethered cord syndrome patients are rich. She found venous abnormalities, collagen abnormalities, and *inflammatory changes* in her patient’s filums. [22]
Klinge found venous filum congestion (i.e., problems of venous outflow), large veins, especially in those with #EDS, and even found a venous angioma in a few patients. [23]
She found major collagen abnormalities in the filums of her occult tethered cord syndrome patients. [24]
Klinge also found—and if you have #MECFS, this may be a bit more your love language—major inflammatory changes: microglia in the filum, activated mast cells, CD45 lymphocytes. She wonders if this might be mirroring some kind of neuroinflammation happening in the spinal cord. [25]
In other words, Klinge found in her patients’ filums all the
same “themes” we keep seeing at the craniocervical junction: abnormal venous outflow, collagen abnormalities, neuroinflammation. This fits into the connective tissue hypothesis of #MECFS [26] https://medium.com/@jenbrea/onset-part-iii-connections-65269f41b861">https://medium.com/@jenbrea/...
same “themes” we keep seeing at the craniocervical junction: abnormal venous outflow, collagen abnormalities, neuroinflammation. This fits into the connective tissue hypothesis of #MECFS [26] https://medium.com/@jenbrea/onset-part-iii-connections-65269f41b861">https://medium.com/@jenbrea/...
Here is where things get EVEN more interesting. While abnormal collagen was common in her OTC patients, there were no significant differences in the rate of collagen abnormalities between her EDS patients and patients without EDS. [27]
While 60% of her OTC patients had #EDS, Klinge says she found nothing indicative of a problem of collagen in the filum “tied to the connective tissue disorder.” The key, Klinge thinks, may NOT be EDS. They key, Klinge says, might be mast cells.
That’s a bombshell. [28]
That’s a bombshell. [28]
Recall that last year, I wondered if we might be conceiving of #EDS & #MECFS the wrong way. At the time, my surgeon thought I had EDS. I disagreed. The more patients he sees w/o EDS, the more he thinks the common connection is #MCAS. @DrEReinhold [29] https://link.medium.com/3QwByEPyA7 ">https://link.medium.com/3QwByEPyA...
This raises SO MANY QUESTIONS. Is the collagen abnormality actually genetic? If it is, why does it present in some patients as an #EDS phenotype while others may only have noticeable damage in a few, discrete places? (In my case, my filum and CCJ.) [30]
If the problem isn’t genetic, what’s preventing normal collagen weaving and—crucially—*why is it ongoing*? Could it be that an autoimmune process disrupts mast cells function? Or might an ongoing infection being keeping mast cells “hot,” as @microbeminded2 has wondered? [31]
What I can’t help but wonder is if my tethered cord had been diagnosed when I was much younger, or when I first started developing #MECFS symptoms, and I had had surgery, might I have avoided full-blown #MECFS and #POTS? Might I have ever needed a fusion? [32]
If for many years, neurosurgeons have thought tethered cord syndrome only happens in kids, is diagnosed by a low-lying conus, and is something to look out for in #EDS but not, say, people with #MECFS, then perhaps we’ve been missing a lot of cases! [33]
I don’t think me, @jeff_says_that, @julierehmeyer, and the growing number of patients with both craniocervical instability and tethered cord syndrome were misdiagnosed with #MECFS. [34]
There is a paradigm problem. Either PEM is not unique to #MECFS or we were missing (and perhaps this is one of them?) the link between infectious onset, inflammation, and #MECFS symptoms. And that the link, the “it” that keeps people from recovering, is tissue damage. [35]
. @ASAPorg’s talks are wonderful. I encourage everyone in #MECFS to watch and perhaps attend future conferences. @microbeminded2 @MBVanElzakker @sjmnotes @keithgeraghty @LBatemanMD @JanetDafoe @DrMaureenHanson @ruhoyMD @DrEReinhold @Dr_M_Guthridge @mhornig https://www.youtube.com/channel/UCJHul2aTWLIjLBUuIsJSWvg/playlists">https://www.youtube.com/channel/U...
Also just wanted to copy @BhupeshPrusty @Derya_ @BendyBrain @davidtuller1 @keithgeraghty @julierehmeyer @jeff_says_that on this thread.
I know not every researcher or clinician has had time to dig into my writings on Medium, and so the above thread is really beginning the conversation in mid-sentence: https://link.medium.com/ypbBQV0GA7 ">https://link.medium.com/ypbBQV0GA...
However, Klinge’s talk really clicked *a lot* of things into place for me around the possible infection—>inflammation––>connective tissue damage causal chain. In particular, her immunological findings. So, I felt compelled to share! https://twitter.com/jenbrea/status/1275902798475882496?s=21">https://twitter.com/jenbrea/s...
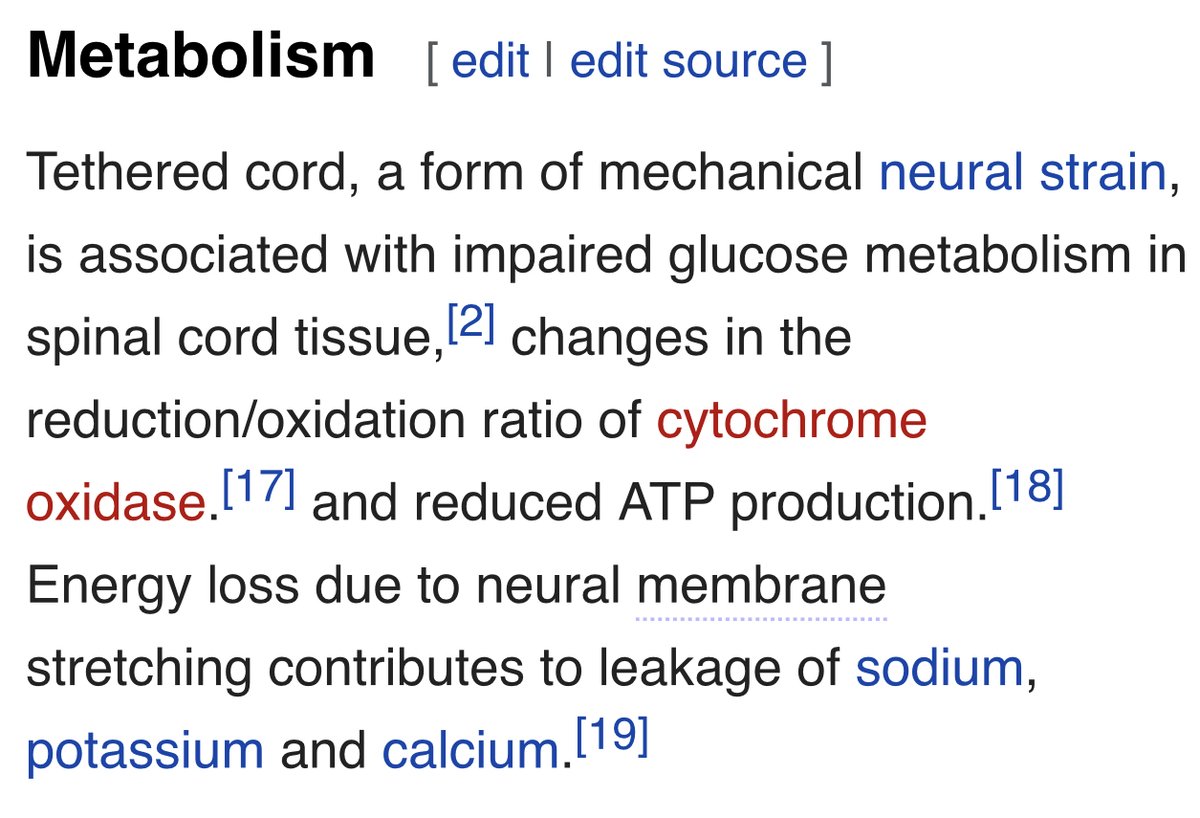
The one thing Klinge does not discuss in this talk, but that I think is potentially quite relevant for #MECFS, are the metabolic impacts of tethered cord syndrome. Again, we see some familiar findings such as a switch to anaerobic metabolism, reduced ATP production.
Tethered cord also causes spinal cord hypoperfusion (analogous to the hypoperfusion we see in #MECFS brains?). In animal models, they find reduced NK cell function. (Some of that literature summarized here: https://www.me-pedia.org/wiki/Neural_strain)">https://www.me-pedia.org/wiki/Neur...
I’d love to hear what you think. I’m also tagging Julie & Jeff since like me, they both had #MECFS, #MCAS and CCI + tethered cord.
There are of course 100+ patients who have been diagnosed with CCI, and a growing number with tethered cord syndrome, but we are the ones who are most public and on Twitter.
@fereshtehjahan1 another interesting thought: Is #MCAS a connective tissue disorder? (MCAS is a common comorbidity of #MECFS that might explain the epidemiological overlap of EDS & ME) https://twitter.com/joshuadmiller/status/1276033247772848128?s=21">https://twitter.com/joshuadmi...
How might mast cell/collagen research help us develop better diagnostic techniques for #hEDS (currently a clinical diagnosis), #MECFS, and #MCAS? https://twitter.com/joshuadmiller/status/1276037951416344577?s=21">https://twitter.com/joshuadmi...
At a Q&A yesterday, Dr. Klinge said (according to a patient’s notes): “There are some MRI studies where ppl have looked at the motion of upper spinal cord in Cine MRI before and after TCR.”
Findings: TCR changes the motion of spinal cord (up and down, front to back) and there is an indication that TCR has remote effect on spinal cord motion *and* suspension of the skull base (!!)
In a different cadaver study, they looked at the conus and end of filum. They found there are cells that are pressure sensors of CSF flow (could the filum be a sensor of CSF pressure?) and the filum might actually be a CSF pressure and flow sensor.
She said: “Still, we don& #39;t have clinical studies. Very valuable old studies and it’s unfortunate that they sit in the sand.” WE NEED MORE RESEARCH.

 Read on Twitter
Read on Twitter![This tethering exerts a downward force on your spinal cord. It’s why some neurosurgeons think tethered cord might predispose people to developing craniocervical instability/atlantoaxial instability (CCI/AAI) or symptomatic Chiari later in life. [3] This tethering exerts a downward force on your spinal cord. It’s why some neurosurgeons think tethered cord might predispose people to developing craniocervical instability/atlantoaxial instability (CCI/AAI) or symptomatic Chiari later in life. [3]](https://pbs.twimg.com/media/EbTbh-kU8AAadxe.jpg)
![In her talk, Dr. Klinge presents the symptoms and outcomes of 113 patients with occult tethered cord (OTC). OTC is tethered cord that *does not appear on a lumbar MRI.* [12] In her talk, Dr. Klinge presents the symptoms and outcomes of 113 patients with occult tethered cord (OTC). OTC is tethered cord that *does not appear on a lumbar MRI.* [12]](https://pbs.twimg.com/media/EbThTPRUMAAxxld.jpg)
![Tethered cord is generally considered to be a genetic or developmental condition. (I suspect there may also be important environmental factors that contribute to it becoming symptomatic or not.) Key is that it presents very differently in infants, children, and adults. [13] Tethered cord is generally considered to be a genetic or developmental condition. (I suspect there may also be important environmental factors that contribute to it becoming symptomatic or not.) Key is that it presents very differently in infants, children, and adults. [13]](https://pbs.twimg.com/media/EbTi5-IUMAAYp-P.jpg)
![Here are some of the common symptoms of tethered cord syndrome, pre/post tethered cord release surgery. I marked the ones I use to have in red. (More on symptoms here: https://www.me-pedia.org/wiki/Teth... [15] Here are some of the common symptoms of tethered cord syndrome, pre/post tethered cord release surgery. I marked the ones I use to have in red. (More on symptoms here: https://www.me-pedia.org/wiki/Teth... [15]](https://pbs.twimg.com/media/EbTjNqAUYAAuDJK.jpg)
![Here are some of the common symptoms of tethered cord syndrome, pre/post tethered cord release surgery. I marked the ones I use to have in red. (More on symptoms here: https://www.me-pedia.org/wiki/Teth... [15] Here are some of the common symptoms of tethered cord syndrome, pre/post tethered cord release surgery. I marked the ones I use to have in red. (More on symptoms here: https://www.me-pedia.org/wiki/Teth... [15]](https://pbs.twimg.com/media/EbTjNqAUcAEvIGx.jpg)
![In addition to CCI and Chiari, it is often comorbid with #EDS, dysautonomia, #POTS, and #MCAS. However, many, many cases are being missed. Klinge& #39;s talk helps explain why. In fact, if we are relying primarily on MRIs, we are probably diagnosing tethered cord ALL WRONG. [16] In addition to CCI and Chiari, it is often comorbid with #EDS, dysautonomia, #POTS, and #MCAS. However, many, many cases are being missed. Klinge& #39;s talk helps explain why. In fact, if we are relying primarily on MRIs, we are probably diagnosing tethered cord ALL WRONG. [16]](https://pbs.twimg.com/media/EbTkRQJUwAAZJL1.jpg)
![Klinge found *no statistically significant differences* in the level of the conus between her surgical patients and healthy controls. This is mindblowing. [18] Klinge found *no statistically significant differences* in the level of the conus between her surgical patients and healthy controls. This is mindblowing. [18]](https://pbs.twimg.com/media/EbTl4k5U4AAdiP1.jpg)
![Fat is another problem. A fatty filum is a major radiological sign of tethered cord that does not appear with OTC. Some of Klinge’s OTC patients actually DID have fat. It might have appeared on one MRI, but not another, perhaps due to CSF pulsation...[20] Fat is another problem. A fatty filum is a major radiological sign of tethered cord that does not appear with OTC. Some of Klinge’s OTC patients actually DID have fat. It might have appeared on one MRI, but not another, perhaps due to CSF pulsation...[20]](https://pbs.twimg.com/media/EbTn-iRVcAEpmzq.jpg)
![The results of Klinge’s histology studies of her 113 occult tethered cord syndrome patients are rich. She found venous abnormalities, collagen abnormalities, and *inflammatory changes* in her patient’s filums. [22] The results of Klinge’s histology studies of her 113 occult tethered cord syndrome patients are rich. She found venous abnormalities, collagen abnormalities, and *inflammatory changes* in her patient’s filums. [22]](https://pbs.twimg.com/media/EbTpFzFU8AA0eEi.jpg)
![She found major collagen abnormalities in the filums of her occult tethered cord syndrome patients. [24] She found major collagen abnormalities in the filums of her occult tethered cord syndrome patients. [24]](https://pbs.twimg.com/media/EbTqGJJVcAAoa0W.jpg)
![Klinge also found—and if you have #MECFS, this may be a bit more your love language—major inflammatory changes: microglia in the filum, activated mast cells, CD45 lymphocytes. She wonders if this might be mirroring some kind of neuroinflammation happening in the spinal cord. [25] Klinge also found—and if you have #MECFS, this may be a bit more your love language—major inflammatory changes: microglia in the filum, activated mast cells, CD45 lymphocytes. She wonders if this might be mirroring some kind of neuroinflammation happening in the spinal cord. [25]](https://pbs.twimg.com/media/EbTq050UEAEsAPk.jpg)
![Here is where things get EVEN more interesting. While abnormal collagen was common in her OTC patients, there were no significant differences in the rate of collagen abnormalities between her EDS patients and patients without EDS. [27] Here is where things get EVEN more interesting. While abnormal collagen was common in her OTC patients, there were no significant differences in the rate of collagen abnormalities between her EDS patients and patients without EDS. [27]](https://pbs.twimg.com/media/EbTsBnVUYAALxt3.jpg)
![If the problem isn’t genetic, what’s preventing normal collagen weaving and—crucially—*why is it ongoing*? Could it be that an autoimmune process disrupts mast cells function? Or might an ongoing infection being keeping mast cells “hot,” as @microbeminded2 has wondered? [31] If the problem isn’t genetic, what’s preventing normal collagen weaving and—crucially—*why is it ongoing*? Could it be that an autoimmune process disrupts mast cells function? Or might an ongoing infection being keeping mast cells “hot,” as @microbeminded2 has wondered? [31]](https://pbs.twimg.com/media/EbTwgHsUEAAIHfH.jpg)
![If for many years, neurosurgeons have thought tethered cord syndrome only happens in kids, is diagnosed by a low-lying conus, and is something to look out for in #EDS but not, say, people with #MECFS, then perhaps we’ve been missing a lot of cases! [33] If for many years, neurosurgeons have thought tethered cord syndrome only happens in kids, is diagnosed by a low-lying conus, and is something to look out for in #EDS but not, say, people with #MECFS, then perhaps we’ve been missing a lot of cases! [33]](https://pbs.twimg.com/media/EbTx9ymVAAASup6.jpg)