Seeing papers make the rounds that the herd immunity threshold may be much lower than the rough approximation 1-1/R0. Maybe, but let& #39;s slow down a minute.
#1. There is still way too much uncertainty.
#2. This does not qualitatively change our strategy.
My comments. 1/
#1. There is still way too much uncertainty.
#2. This does not qualitatively change our strategy.
My comments. 1/
Two papers are listed in this thread by @mlipsitch, and a third here. https://arxiv.org/abs/2002.04004 ">https://arxiv.org/abs/2002.... 2/ https://twitter.com/mlipsitch/status/1258827506930667523">https://twitter.com/mlipsitch...
The basic premise is that when contact networks are highly heterogeneous, people with the most contacts are at greatest risk of infection. Once they are infected/immune, the network is more "robust" to future outbreaks since they break chains of transmission. 3/
The implication is that the herd immunity threshold (percent that must be infected to drop the effective reproduction number below 1) is lower than the mass action value 1-1/R0. Some interpret this as meaning we are closer to herd immunity. 4/ https://www.washingtonpost.com/outlook/2020/04/29/antibody-test-coronavirus-fatality-immunity/">https://www.washingtonpost.com/outlook/2...
Point #1. There is still way too much uncertainty.
What even is R0? Remember that R0 is context-specific. Britton et al use 2.5 as an example, which could be appropriate for certain populations, but I& #39;ve seen credible estimates of 3.0 or higher. 5/ https://twitter.com/mlipsitch/status/1259068917999382529">https://twitter.com/mlipsitch...
What even is R0? Remember that R0 is context-specific. Britton et al use 2.5 as an example, which could be appropriate for certain populations, but I& #39;ve seen credible estimates of 3.0 or higher. 5/ https://twitter.com/mlipsitch/status/1259068917999382529">https://twitter.com/mlipsitch...
The models assume that incoming risk is equivalent to outgoing risk. In other words, are people who are the most likely to be infected also the most likely to infect others? But do we know this? This is a question I have seen raised by several network epidemiologists. 6/
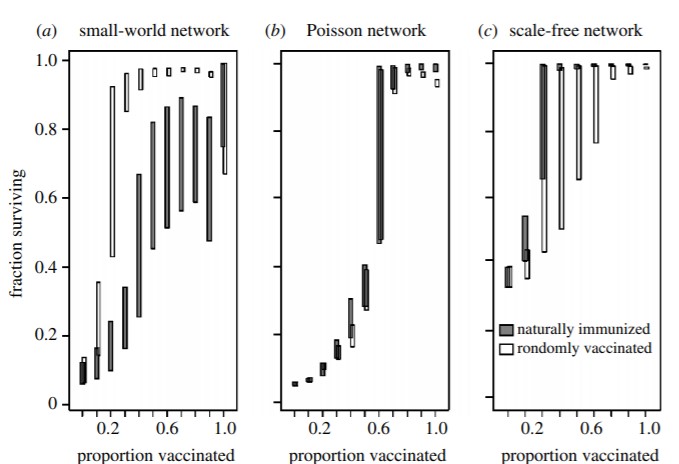
How is the network structured? This paper shows that, while the threshold is lower for scale-free (highly heterogeneous) networks, the opposite is true for small-world (highly structured) networks. 7/
https://twitter.com/bansallab/status/1258872610210877442">https://twitter.com/bansallab...
https://twitter.com/bansallab/status/1258872610210877442">https://twitter.com/bansallab...
Why do we think the network here is scale-free? Some sexual networks have been shown to be scale-free (think commercial sex workers), but why is that true for a respiratory pathogen like SARS-CoV-2? To see dramatic drops in the threshold, the tails must be very heavy. 8/
Maybe our network is heterogeneous right now because essential workers are at work but the rest of us are home. But what happens as things open back up? Wouldn& #39;t our network structure tend to become more homogeneous? 9/ https://twitter.com/mlipsitch/status/1259067061822783489">https://twitter.com/mlipsitch...
Notably, one of the above papers assumes social distancing is ongoing, as pointed out by co-author @caesoma, and so should be interpreted with that in mind. 10/ https://twitter.com/caesoma/status/1257762721317224448">https://twitter.com/caesoma/s...
In fact, the effect of this heterogeneity can actually strengthen the argument for the effectiveness of shutdowns. 11/ https://twitter.com/joel_c_miller/status/1257561071893704706">https://twitter.com/joel_c_mi...
There is also a lot we are still learning about this virus. Who is most susceptible? In what settings is it transmitted? Are fomites a key factor? What is the role of children? Does variation in individual-level viral load drive super-spreading events? 12/
Basically, there is still way too much uncertainty to assume a particular model, and to use that model to establish a potential threshold. 13/ https://twitter.com/caesoma/status/1257762727864434690">https://twitter.com/caesoma/s...
Point #2. This does not qualitatively change our strategy.
Some interpret these papers as strengthening the case for "managed" infection, allowing low risk groups to be infected as a way to protect the vulnerable. I have thoughts... 14/ https://twitter.com/nataliexdean/status/1256351498340044800">https://twitter.com/nataliexd...
Some interpret these papers as strengthening the case for "managed" infection, allowing low risk groups to be infected as a way to protect the vulnerable. I have thoughts... 14/ https://twitter.com/nataliexdean/status/1256351498340044800">https://twitter.com/nataliexd...
A friendly reminder that just because something works in a model doesn& #39;t mean it translates into actionable policy. We are already struggling to protect the vulnerable already, and this will only get harder as transmission increases. 15/ https://twitter.com/joel_c_miller/status/1258933191768825857">https://twitter.com/joel_c_mi...
Highly structured communities of high risk individuals (retirement communities) will remain at risk. 16/ https://twitter.com/joel_c_miller/status/1257561054780915712">https://twitter.com/joel_c_mi...
Furthermore, our groups most likely to be infected are essential workers, including people who are older. They didn& #39;t sign up for this. Is there a credible plan to replace them with low risk individuals? 17/ https://twitter.com/jessikator/status/1257691531340734464?s=20">https://twitter.com/jessikato...
In Sweden, the modeling suggests that they will reach a lower immunity threshold in June. I think they are over-estimating the current seroprevalence in Stockholm and under-estimating severity. Meaning, I think this will keep going longer. 18/ https://twitter.com/nataliexdean/status/1254251246904631302">https://twitter.com/nataliexd...

 Read on Twitter
Read on Twitter