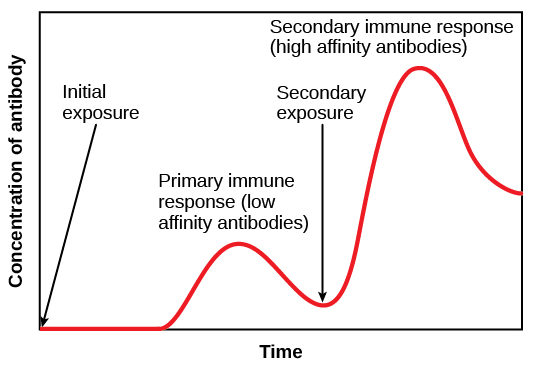
1. Type III hypersensitivity reactions typically develop ~6 h after exposure to antigen.
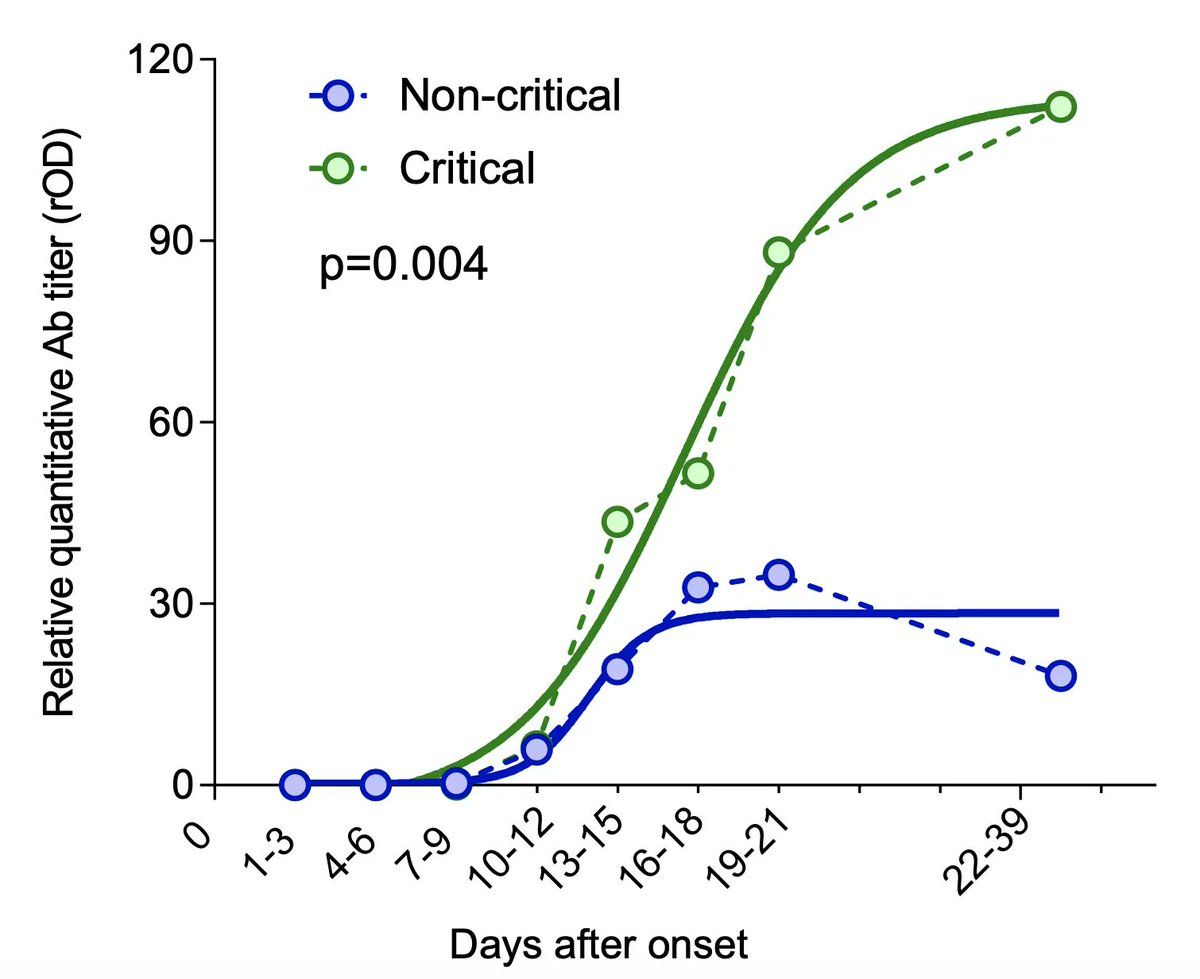
This is the timeframe we are often seeing patients rapidly decompensate in (2L -> 15L -> intubation), usually around day 7 to 14, when an antibody response would be reaching a peak (below)
This is the timeframe we are often seeing patients rapidly decompensate in (2L -> 15L -> intubation), usually around day 7 to 14, when an antibody response would be reaching a peak (below)
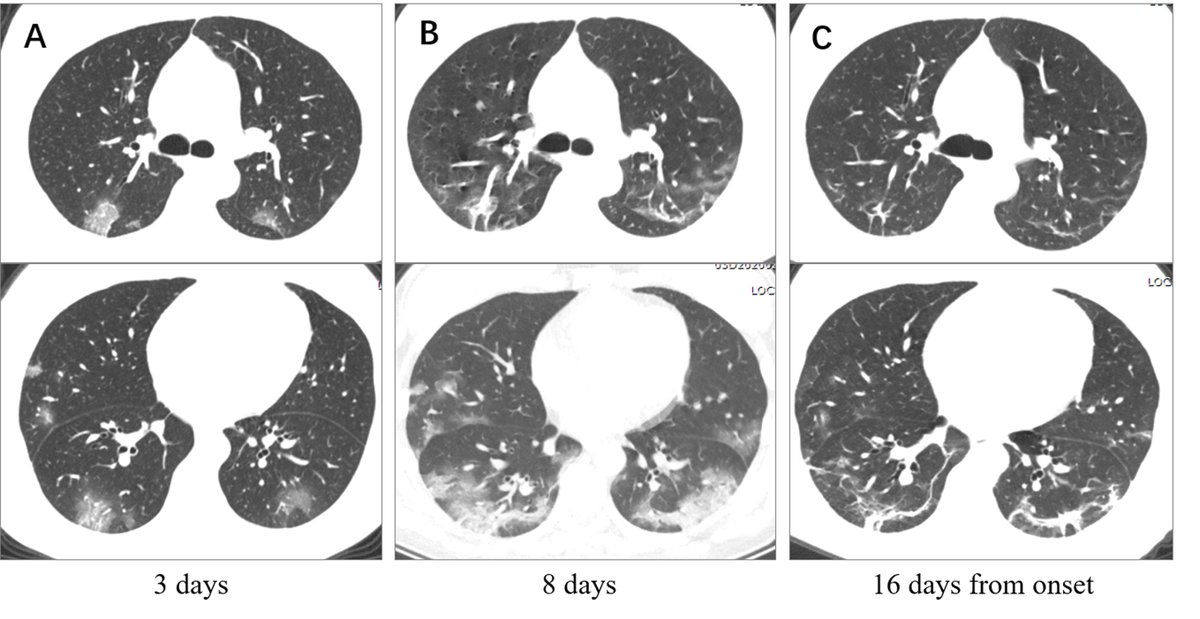
2. Basal lung = where perfusion is greatest
Peripheral lung = where capillary networks are richest.
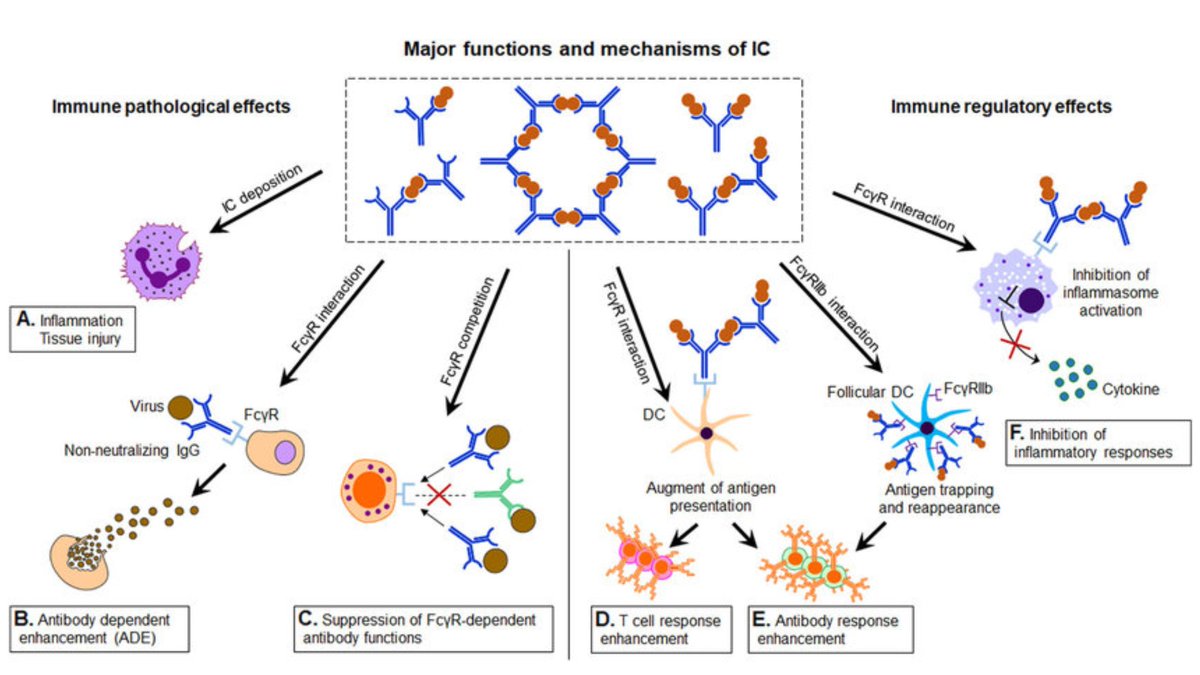
Immune complexes most readily deposit within the interstitium of capillaries --> lymphohistiocytic response.
...this potentially explains the predominant CT findings in COVID-19.
Peripheral lung = where capillary networks are richest.
Immune complexes most readily deposit within the interstitium of capillaries --> lymphohistiocytic response.
...this potentially explains the predominant CT findings in COVID-19.
3. Lung injury in COVID-19 does not behave like classical ARDS.
Patients are poor to oxygenate but have adequate lung compliance, especially early on.
This fits with interstitial edema > intra-alveolar edema and also explains why high PEEP is often needed in these patients.
Patients are poor to oxygenate but have adequate lung compliance, especially early on.
This fits with interstitial edema > intra-alveolar edema and also explains why high PEEP is often needed in these patients.
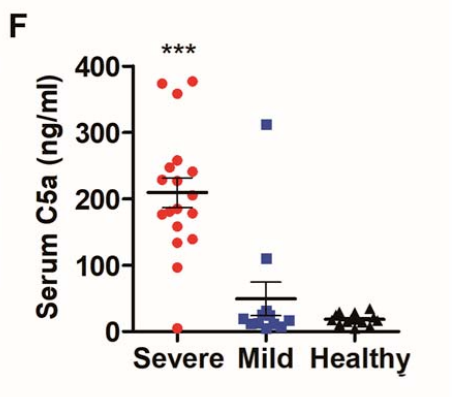
4. Immune complex deposition leads to complement activation.
Complement over-activation, particularly within the lung tissue, is seen in the severe phase of COVID19.
Notably, it is not seen much in the early phase.
Complement over-activation, particularly within the lung tissue, is seen in the severe phase of COVID19.
Notably, it is not seen much in the early phase.
5. Memory B cells have been shown to persist in the lung following pulmonary infection with various respiratory viruses.
An antibody response occurring within the lungs would lead to the greatest degree of intrapulmonary immune complex deposition and damage.
An antibody response occurring within the lungs would lead to the greatest degree of intrapulmonary immune complex deposition and damage.
6. Distant immune complex spread would be variable may partly explain the heterogeneity of other organ damage:
Renal deposition --> AKI / ARF
Muscle capillary bed --> rhabdomyolysis
GI tract --> colitis
Cardiac --> coronary arteritis
CNS --> hemorrhagic necrotizing encephalitis
Renal deposition --> AKI / ARF
Muscle capillary bed --> rhabdomyolysis
GI tract --> colitis
Cardiac --> coronary arteritis
CNS --> hemorrhagic necrotizing encephalitis
TL;DR:
1. Non-SARS coronaviruses are ubiquitous
2. Antibody levels parallel age
3. Sub-neutralizing antibodies are key, as they enhance viremia and disease severity
4. Ab/ag complex deposition may drive severe disease phenotype via type III / IV hypersensitivity rxns
Part 2:
1. Non-SARS coronaviruses are ubiquitous
2. Antibody levels parallel age
3. Sub-neutralizing antibodies are key, as they enhance viremia and disease severity
4. Ab/ag complex deposition may drive severe disease phenotype via type III / IV hypersensitivity rxns
Part 2:

 Read on Twitter
Read on Twitter