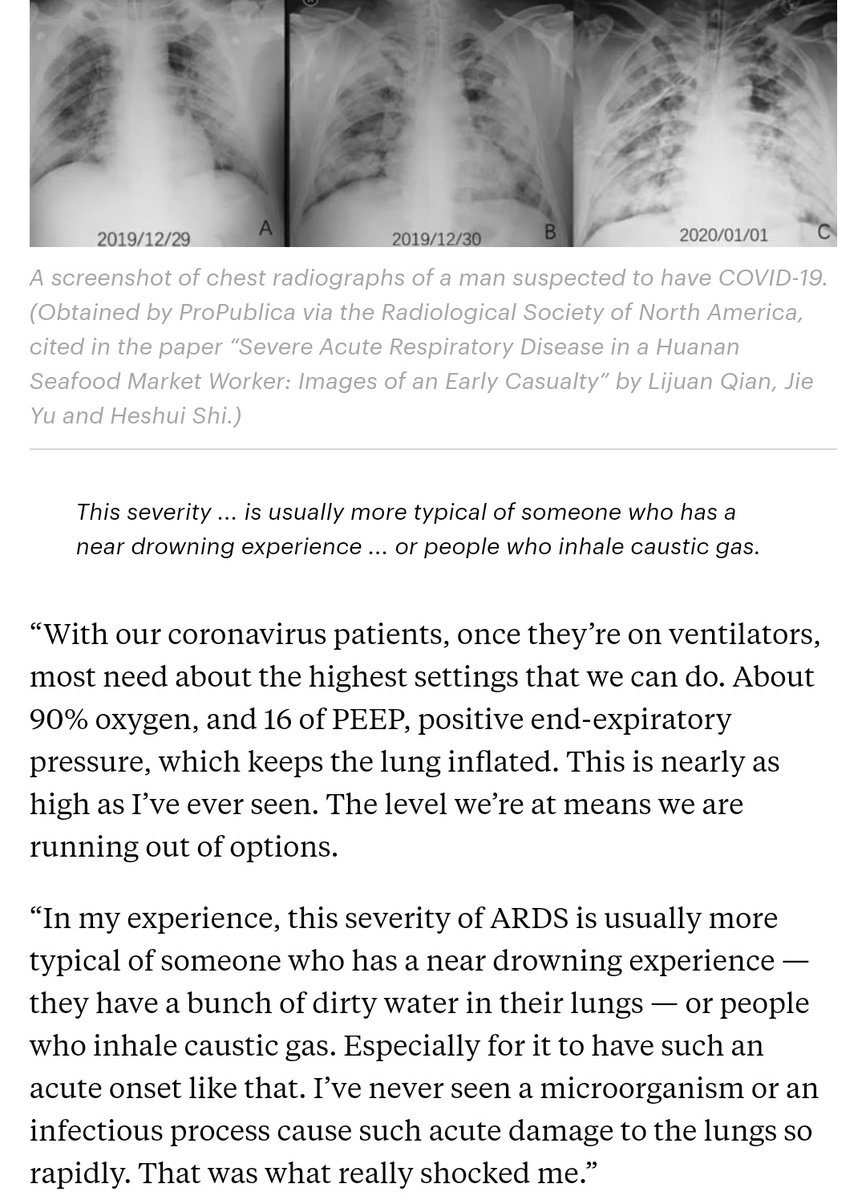
Another reminder that outcomes for intubated patients with this disease are... not great.
The sorts of vent settings required to keep them from dying of hypoxia tend to further intensify the damage to the lungs. https://twitter.com/thisisnotharsh/status/1246193930103918592">https://twitter.com/thisisnot...
The sorts of vent settings required to keep them from dying of hypoxia tend to further intensify the damage to the lungs. https://twitter.com/thisisnotharsh/status/1246193930103918592">https://twitter.com/thisisnot...
https://www.npr.org/sections/health-shots/2020/04/02/826105278/ventilators-are-no-panacea-for-critically-ill-covid-19-patients">https://www.npr.org/sections/...
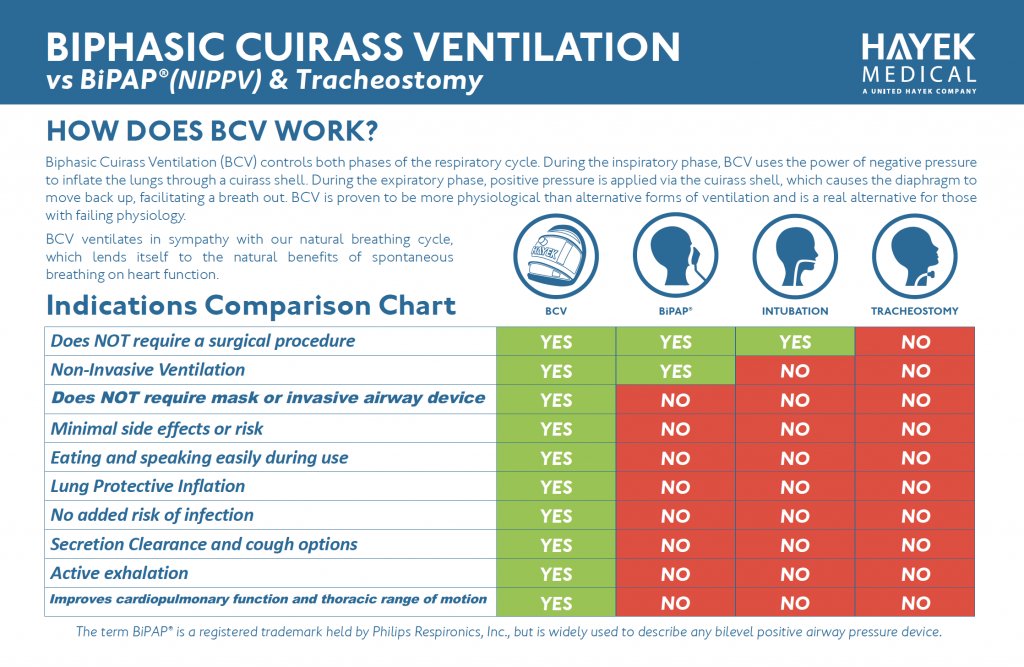
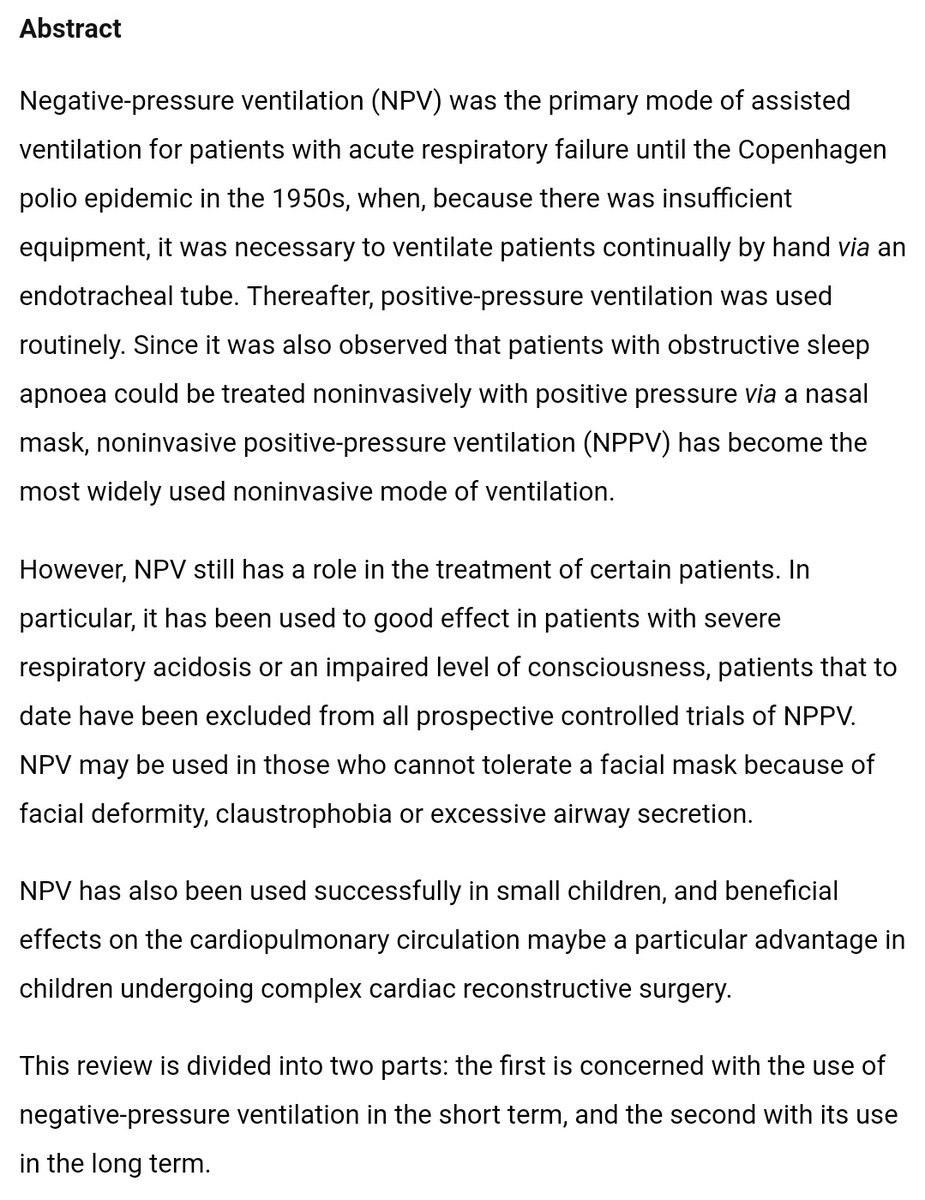
One subject on which I have seen little discussion to date: negative-pressure ventilation.
Negative-pressure ventilation generally results in less ventilator-associated lung damage than the current standard of positive-pressure ventilation: https://pubmed.ncbi.nlm.nih.gov/18079496/ ">https://pubmed.ncbi.nlm.nih.gov/18079496/...
Negative-pressure ventilation generally results in less ventilator-associated lung damage than the current standard of positive-pressure ventilation: https://pubmed.ncbi.nlm.nih.gov/18079496/ ">https://pubmed.ncbi.nlm.nih.gov/18079496/...
Completely counterintuitive:
Negative-pressure ventilators (the & #39;iron lung& #39;) may actually provide *better* oxygenation for patients experiencing ARDS: https://pubmed.ncbi.nlm.nih.gov/22386062/ ">https://pubmed.ncbi.nlm.nih.gov/22386062/...
Negative-pressure ventilators (the & #39;iron lung& #39;) may actually provide *better* oxygenation for patients experiencing ARDS: https://pubmed.ncbi.nlm.nih.gov/22386062/ ">https://pubmed.ncbi.nlm.nih.gov/22386062/...
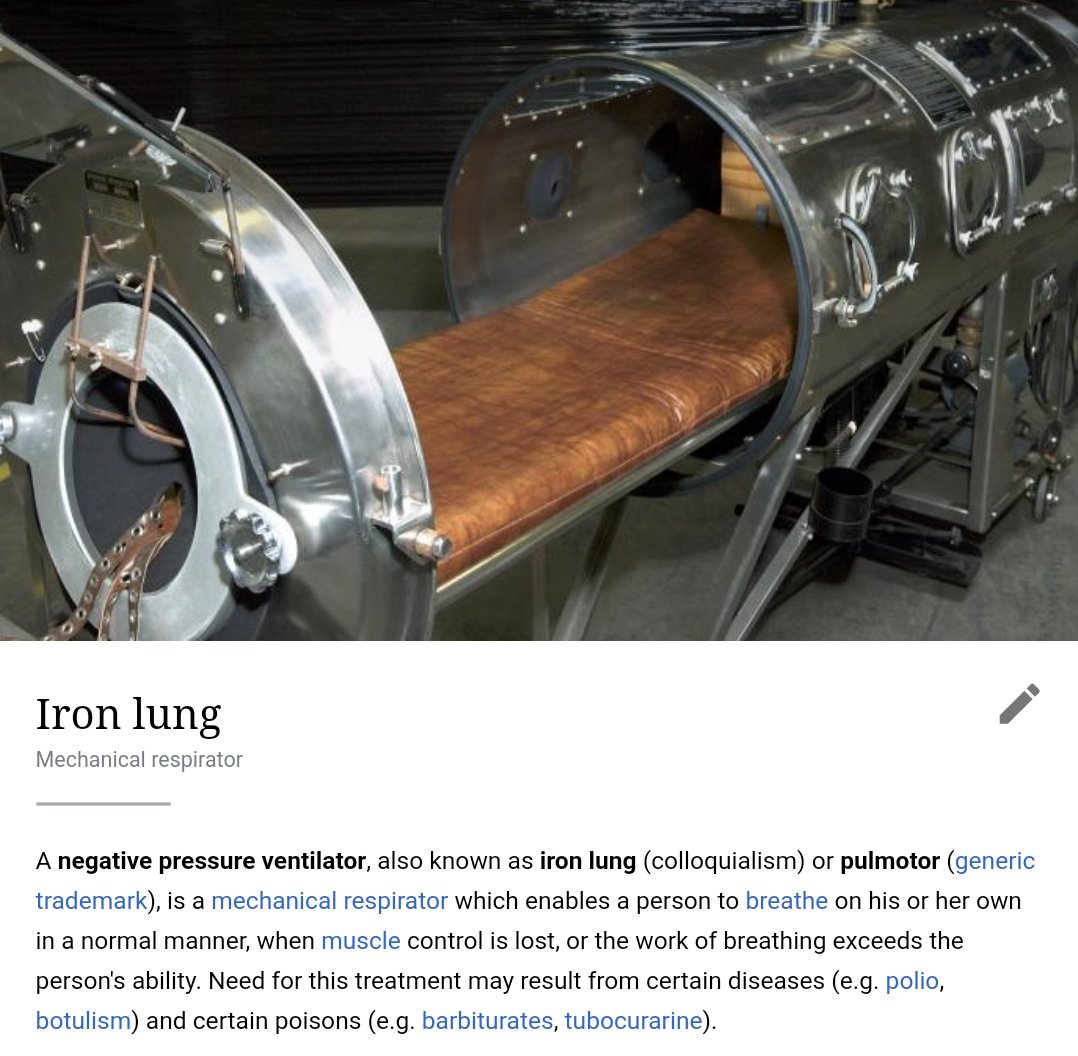
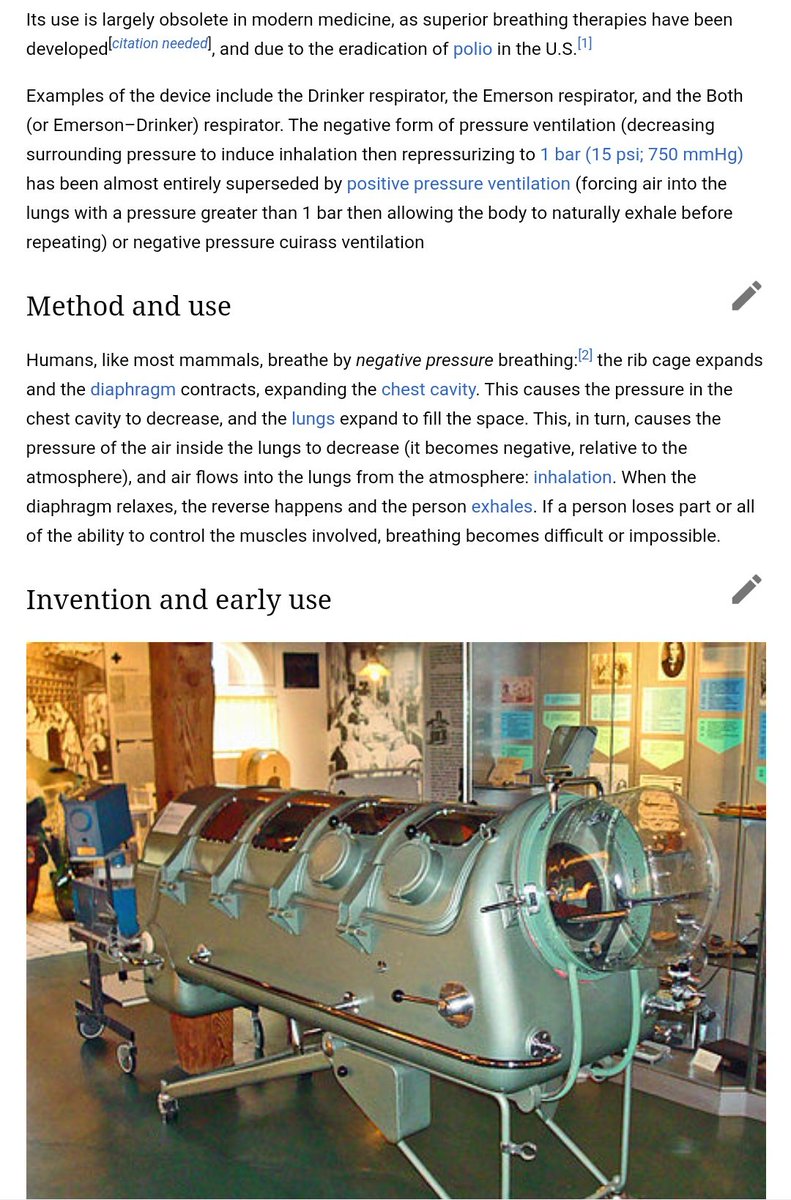
Historically, negative-pressure ventilation required the use of a large and bulky machine.
They were particularly popular in treating acute polio.
Over time, use of this approach declined, mainly due to space requirements and obstruction of access to the patient.
They were particularly popular in treating acute polio.
Over time, use of this approach declined, mainly due to space requirements and obstruction of access to the patient.
But note: & #39;space requirements& #39; and & #39;obstruction of access& #39; are *not* directly medical considerations.
They are predominantly logistical and financial ones.
Pro: money, access
Con: barotrauma
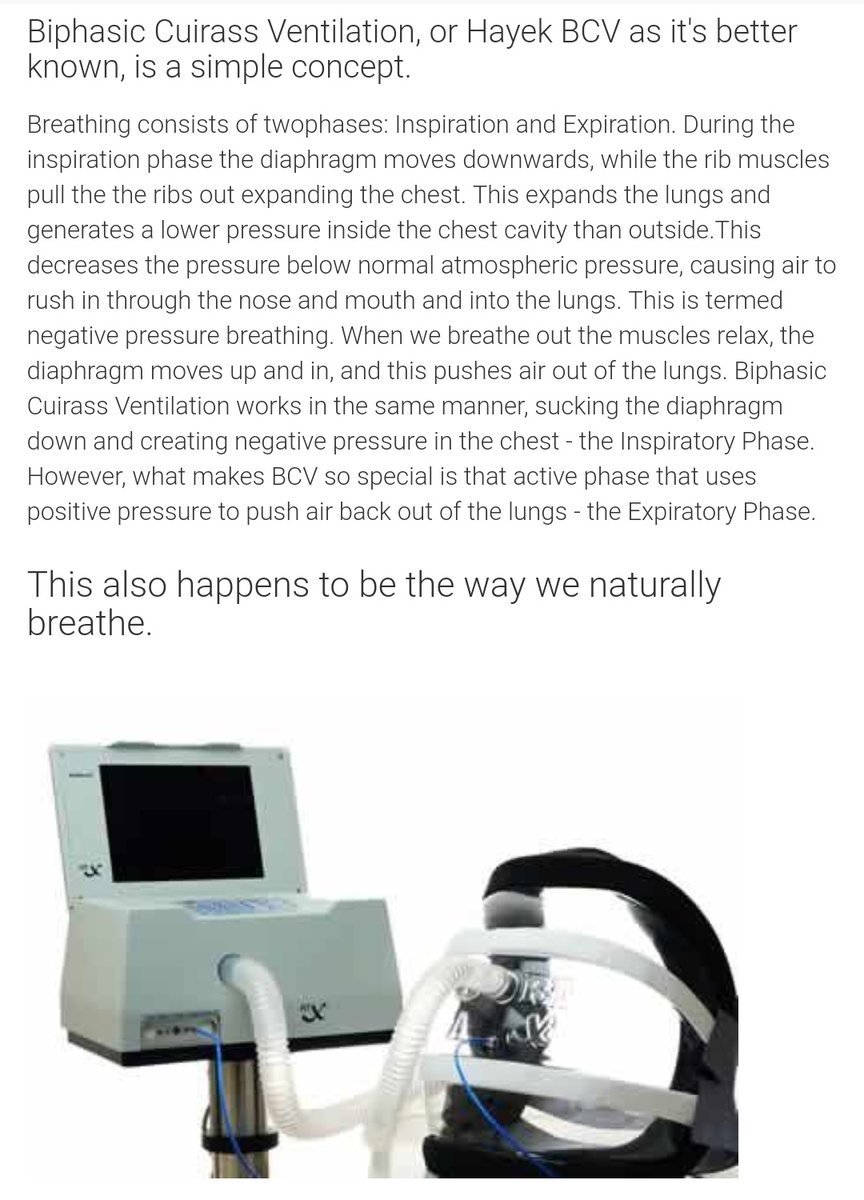
Moreover, newer and more compact designs for negative-pressure ventilation now exist--
They are predominantly logistical and financial ones.
Pro: money, access
Con: barotrauma
Moreover, newer and more compact designs for negative-pressure ventilation now exist--
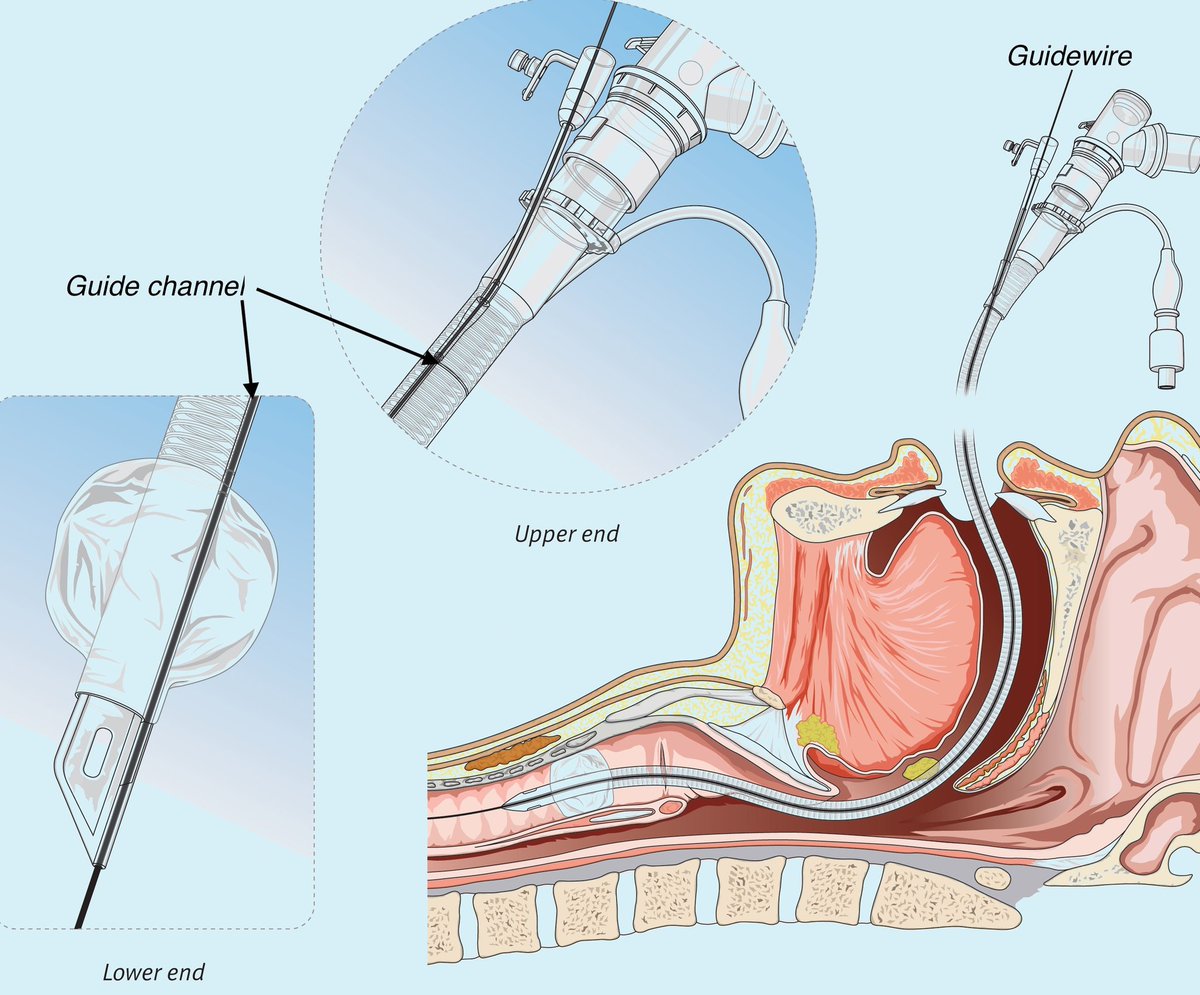
Moreover, access to the lungs themselves is actually *blocked* by the tracheal balloon used in endotracheal intubation.
This requires frequent suctioning of secretions to prevent suffocation, and still mechanically obstructs their removal.
It also blocks tracheal endoscopy.
This requires frequent suctioning of secretions to prevent suffocation, and still mechanically obstructs their removal.
It also blocks tracheal endoscopy.
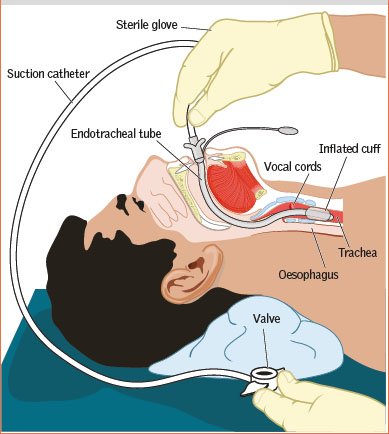
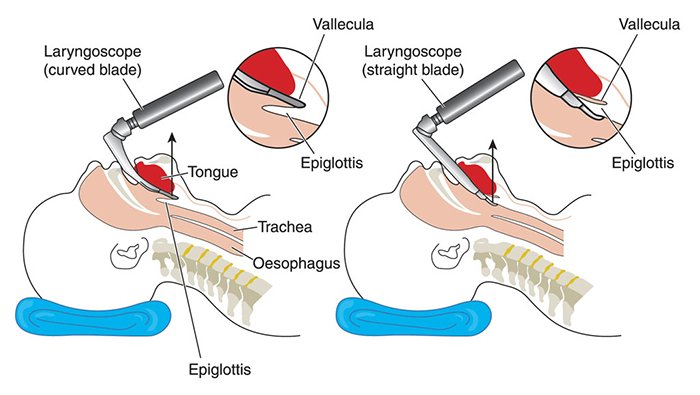
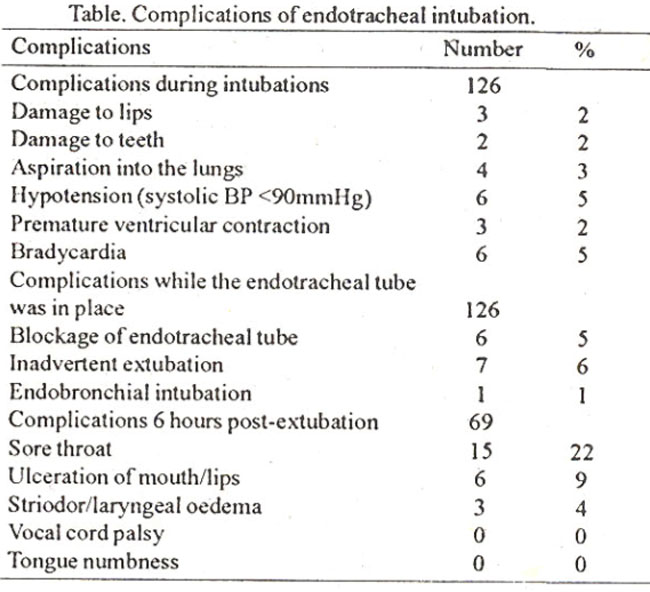
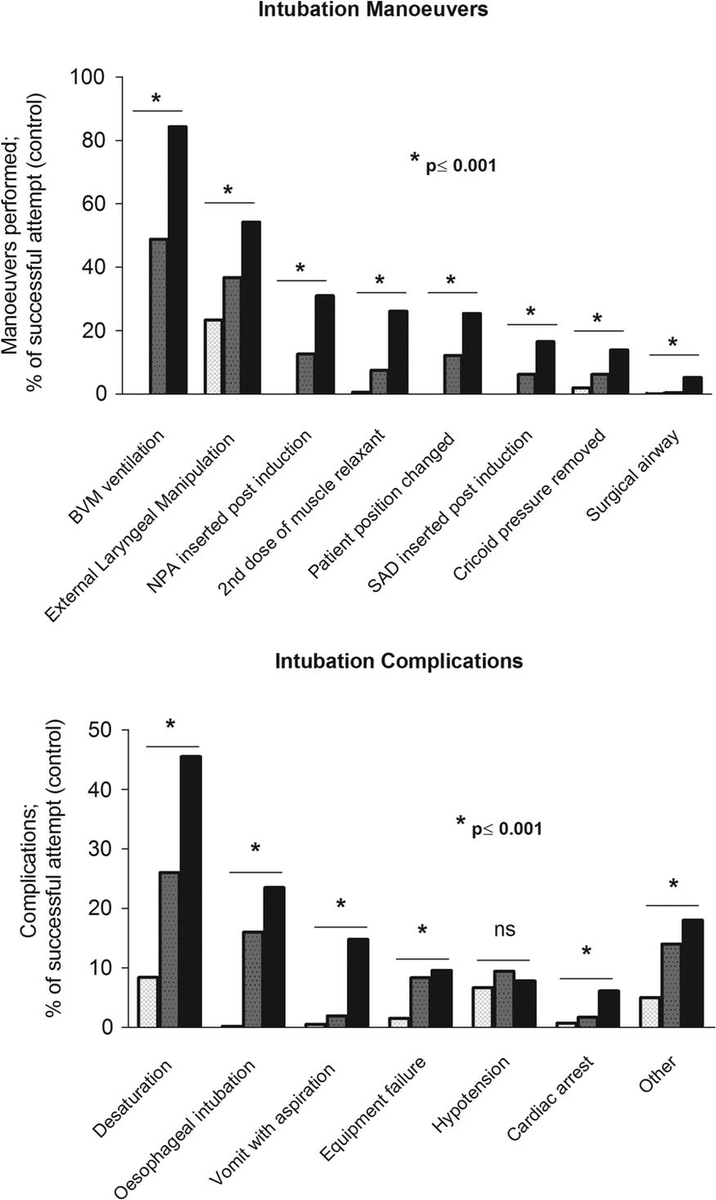
The intubation process is also associated with many potential complications absent in negative-pressure ventilation.
Minor example: oral damage
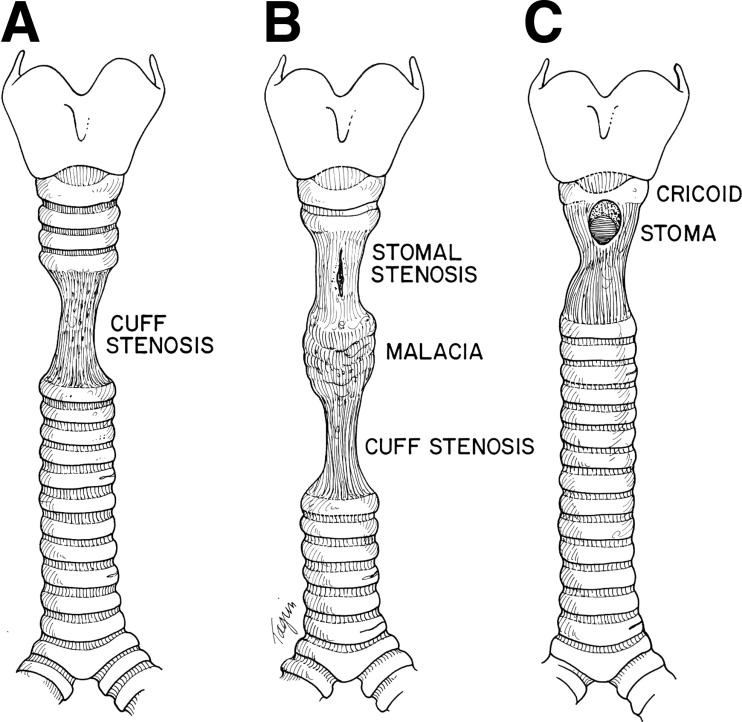
Major example: tracheal stenosis
There is also a risk of blockage by secretions.
Statistics vary by facility.
https://www.intechopen.com/books/tracheal-intubation/long-term-complications-of-tracheal-intubation">https://www.intechopen.com/books/tra...
Minor example: oral damage
Major example: tracheal stenosis
There is also a risk of blockage by secretions.
Statistics vary by facility.
https://www.intechopen.com/books/tracheal-intubation/long-term-complications-of-tracheal-intubation">https://www.intechopen.com/books/tra...
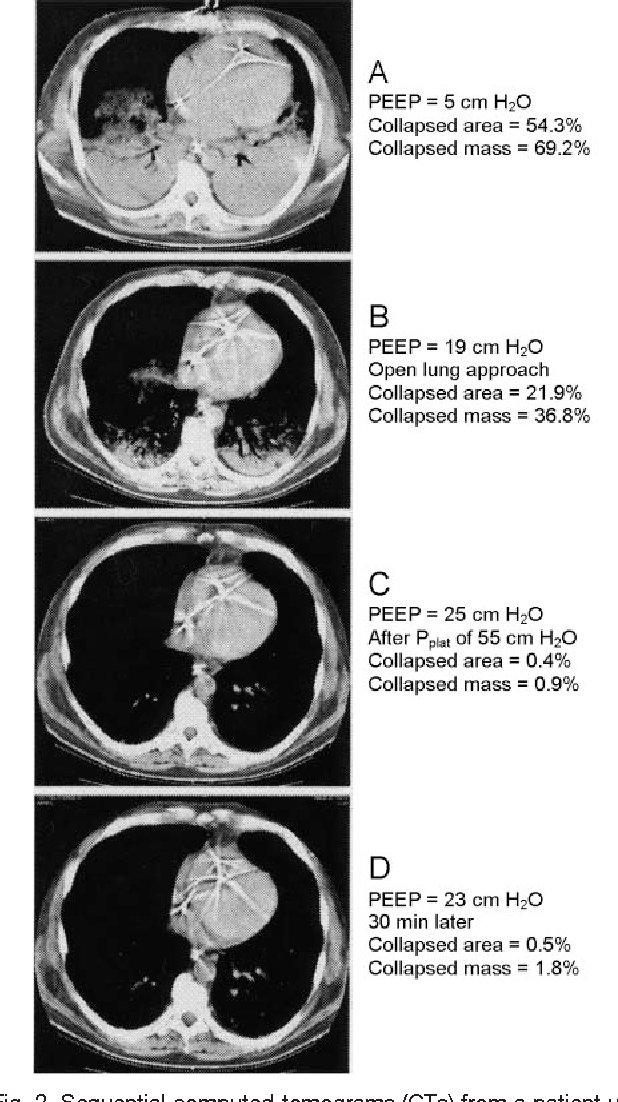
Detailed animal studies with CT scanning showed that negative-pressure ventilation for ARDS results in a greater volume of ventilated lung tissue, and a smaller volume of atelectatic (collapsed) lung tissue, as compared with positive-pressure-- https://pubmed.ncbi.nlm.nih.gov/18651149/ ">https://pubmed.ncbi.nlm.nih.gov/18651149/...
In some regions, negative-pressure ventilation was the standard of care until polio overwhelmed available equipment. Positive-pressure methods prevailed thereafter.
https://erj.ersjournals.com/content/20/1/187
Note">https://erj.ersjournals.com/content/2... again that financial and logistical, not medical, considerations drove the change.
https://erj.ersjournals.com/content/20/1/187
Note">https://erj.ersjournals.com/content/2... again that financial and logistical, not medical, considerations drove the change.
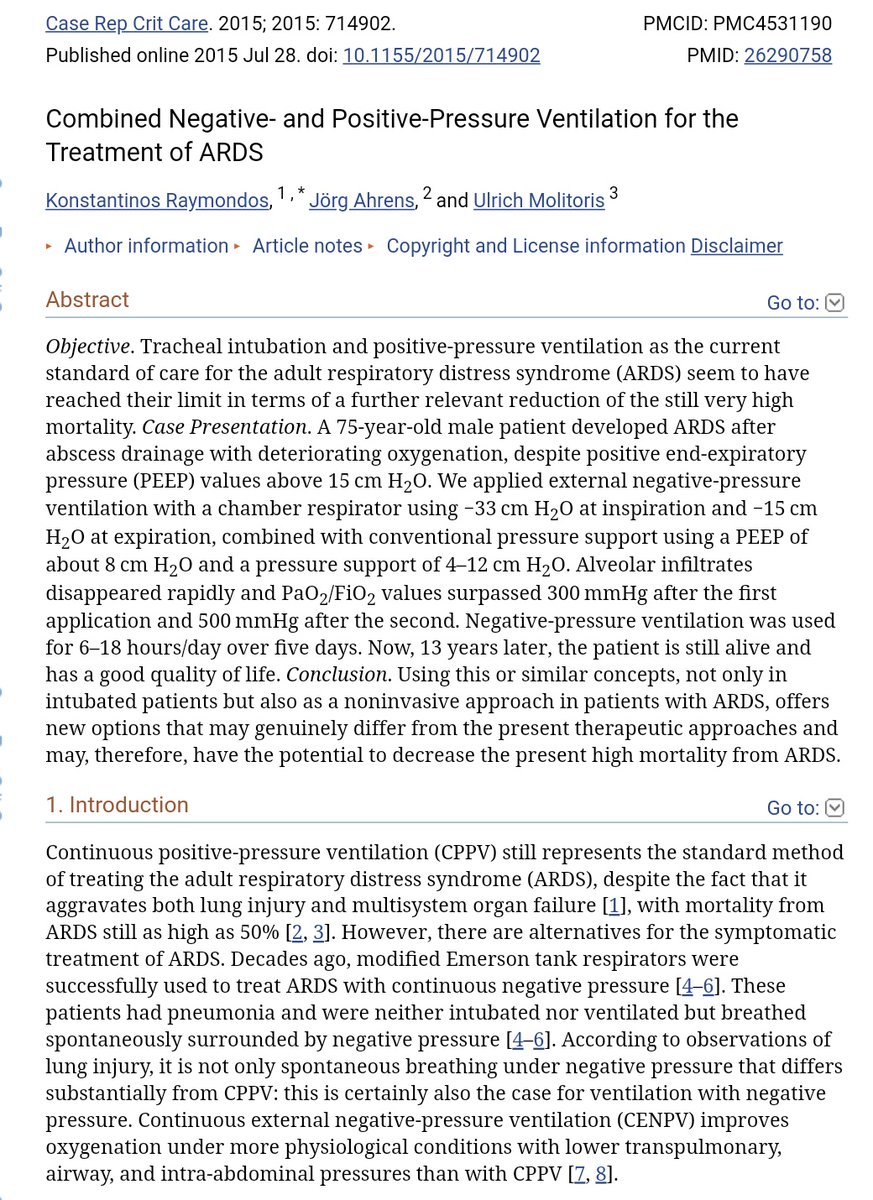
Negative-pressure and positive-pressure ventilation can also be used *simultaneously*, given device synchronization.
In one ARDS case study, this apparently prompted rapid clinical recovery and enhanced oxygenation, even at gentler PEEP settings--
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4531190/">https://www.ncbi.nlm.nih.gov/pmc/artic...
In one ARDS case study, this apparently prompted rapid clinical recovery and enhanced oxygenation, even at gentler PEEP settings--
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4531190/">https://www.ncbi.nlm.nih.gov/pmc/artic...
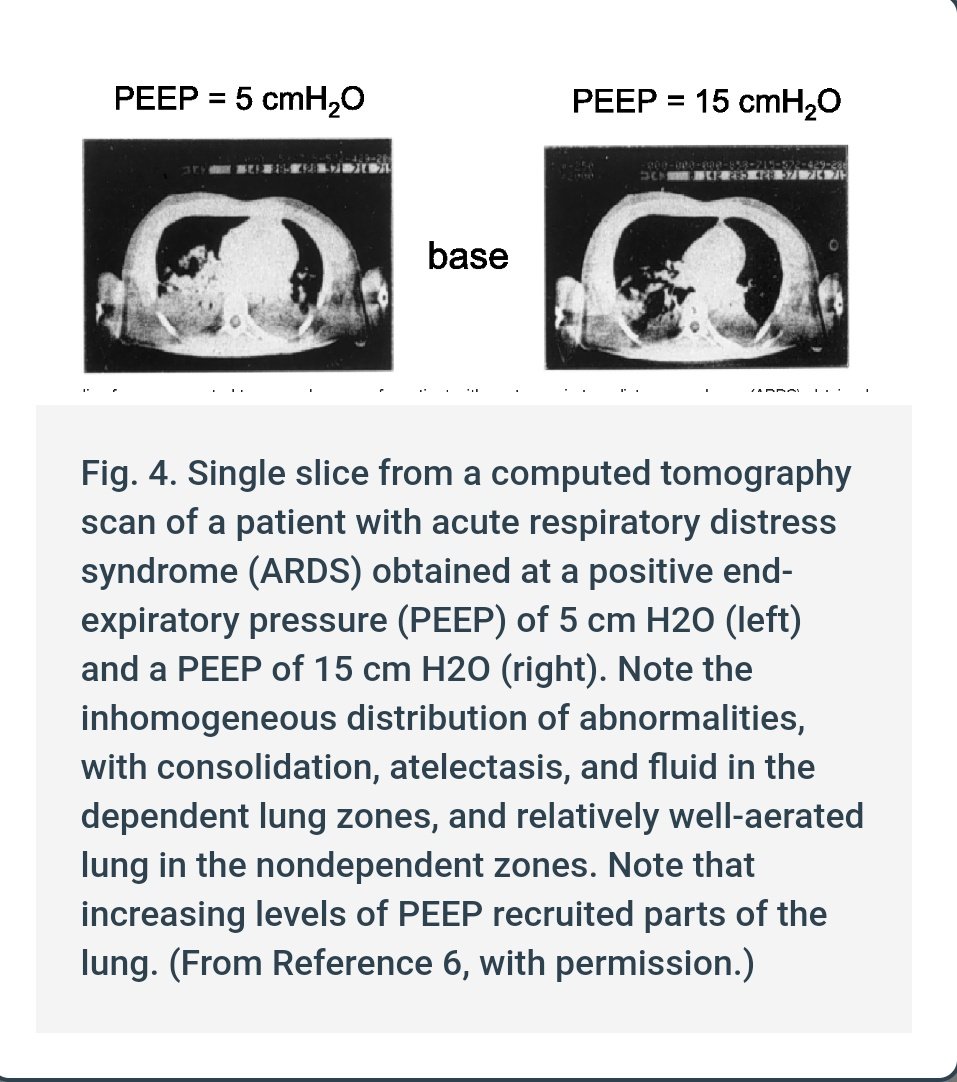
ARDS often requires rather extreme PEEP settings to recruit damaged regions of the lungs-- in other words, to un-collapse the swollen and fluid-soaked areas.
Meanwhile, negative-pressure ventilation is free of barotrauma at all and still achieves greater oxygenation in ARDS.
Meanwhile, negative-pressure ventilation is free of barotrauma at all and still achieves greater oxygenation in ARDS.
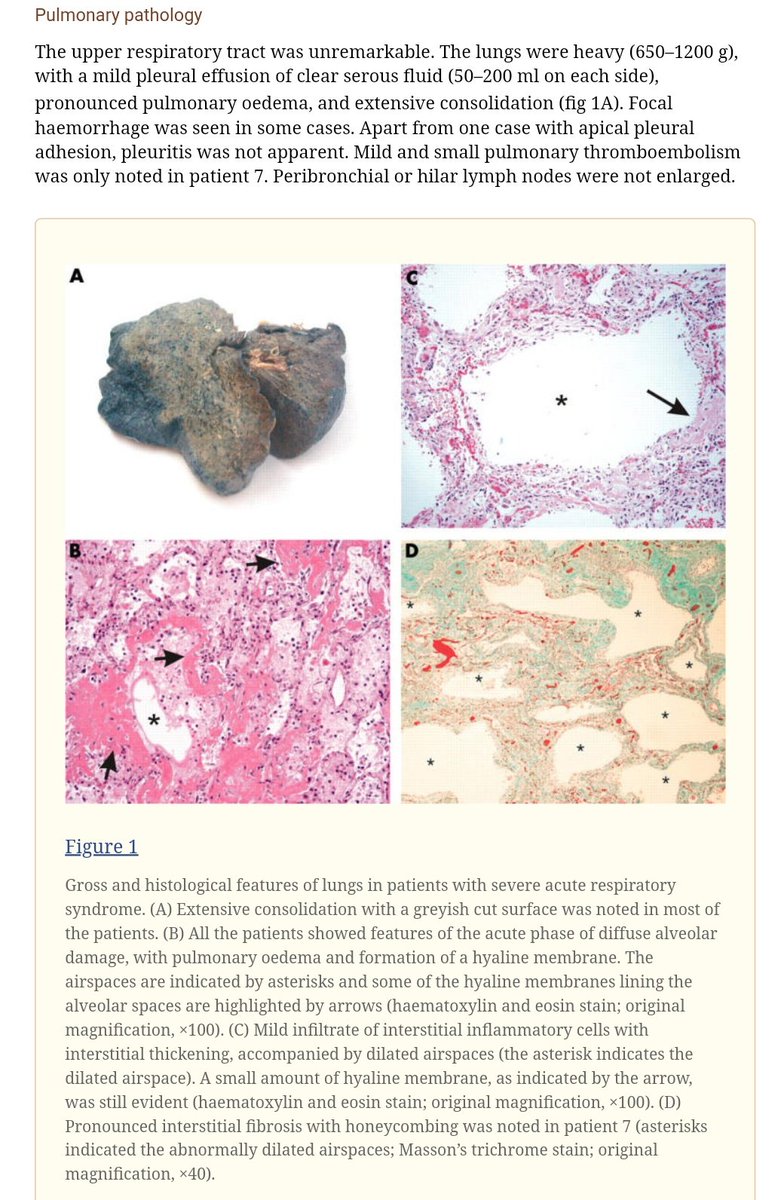
Lung samples from fatal SARS cases were collapsed, edematous, fibrotic, and greyish, with heavily disrupted microstructure. COVID-19 is presumably similar.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4531190/
Inflating">https://www.ncbi.nlm.nih.gov/pmc/artic... such lungs with positive pressure requires high levels thereof.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4531190/
Inflating">https://www.ncbi.nlm.nih.gov/pmc/artic... such lungs with positive pressure requires high levels thereof.
In a time of serious equipment shortages and supplier constraints, iron lungs also involve much simpler feedback control mechanisms and are arguably easier to build with non-specialist manufacturing. https://twitter.com/halvorz/status/1246482610433527808?s=19">https://twitter.com/halvorz/s...
Another few overview papers on negative-pressure ventilation:
https://jamanetwork.com/journals/jama/article-abstract/196033
https://jamanetwork.com/journals/... href=" #57066340">https://accessmedicine.mhmedical.com/content.aspx?bookid=520§ionid=41692256 #57066340
The">https://accessmedicine.mhmedical.com/content.a... incessant focus on non-medical reasons to use a device that by all evidence appears to produce a higher risk of death in ARDS seems absurd.
https://jamanetwork.com/journals/jama/article-abstract/196033
The">https://accessmedicine.mhmedical.com/content.a... incessant focus on non-medical reasons to use a device that by all evidence appears to produce a higher risk of death in ARDS seems absurd.
Ultimately, it is best if ventilation can be avoided.
Although negative-pressure methods pose less risk of lung damage, they are not perfect-- e.g. they likely have equal risk of diaphragm problems:
https://pubmed.ncbi.nlm.nih.gov/23838714/
Prone">https://pubmed.ncbi.nlm.nih.gov/23838714/... positioning can help: https://twitter.com/BBroderickMD/status/1244489353071661057?s=19">https://twitter.com/BBroderic...
Although negative-pressure methods pose less risk of lung damage, they are not perfect-- e.g. they likely have equal risk of diaphragm problems:
https://pubmed.ncbi.nlm.nih.gov/23838714/
Prone">https://pubmed.ncbi.nlm.nih.gov/23838714/... positioning can help: https://twitter.com/BBroderickMD/status/1244489353071661057?s=19">https://twitter.com/BBroderic...
And above all: treat early! https://twitter.com/__ice9/status/1246125893623390209?s=19">https://twitter.com/__ice9/st...

 Read on Twitter
Read on Twitter