A plausible mechanism apparently exists for the tendency of COVID-19 to be more severe in patients with type-A/AB blood, compared to B or especially O:
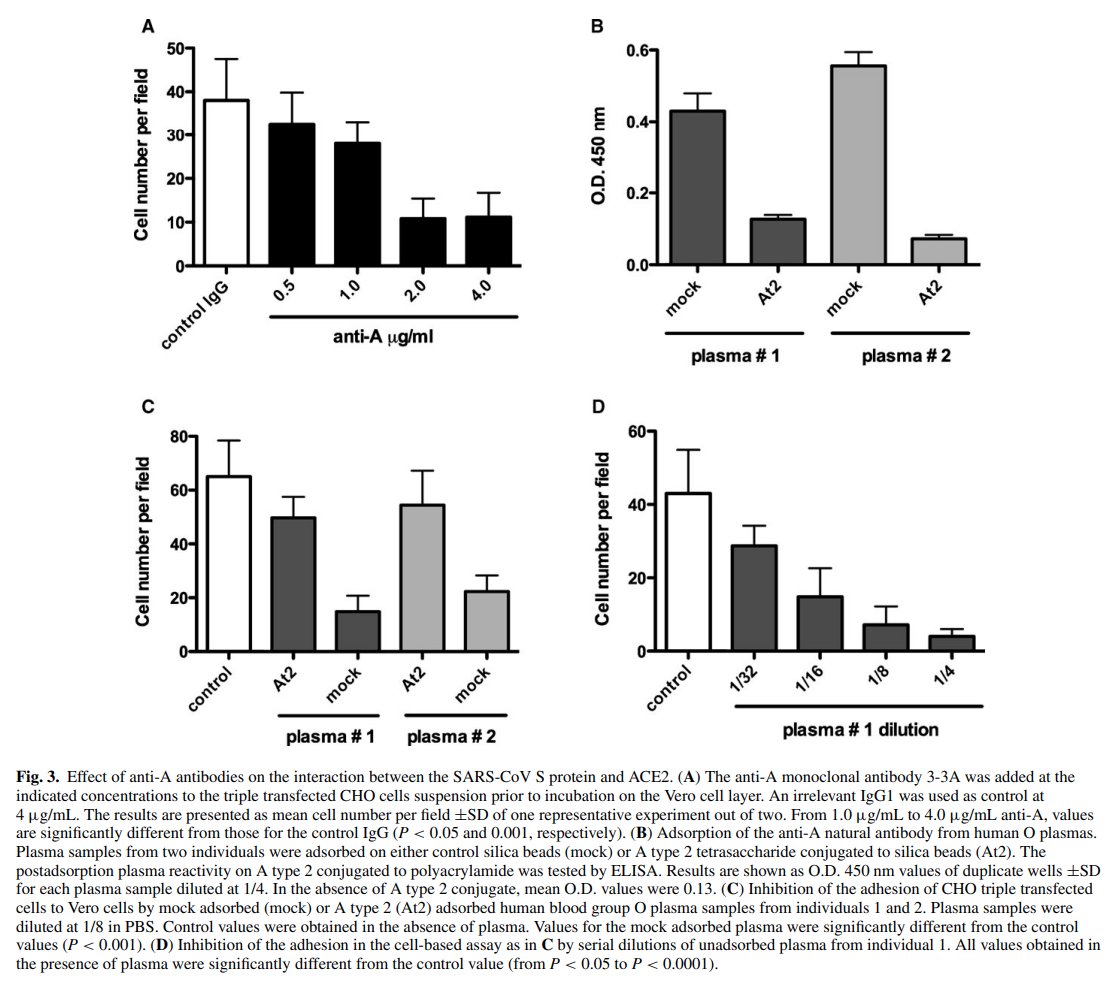
Anti-A antibodies (present in types B/O) apparently disrupt the binding of SARS-CoV to ACE-2. SARS-CoV-2 is likely similar. https://twitter.com/psykiln/status/1245858763526901760">https://twitter.com/psykiln/s...
Anti-A antibodies (present in types B/O) apparently disrupt the binding of SARS-CoV to ACE-2. SARS-CoV-2 is likely similar. https://twitter.com/psykiln/status/1245858763526901760">https://twitter.com/psykiln/s...
Although not studied here, it is possible that anti-B antibodies might also confer a (smaller) degree of protective interference.
Both are hypothesized to facilitate anti-viral immunity, and patients with type O blood have both.
Unclear, new tighter-binding Spike protein.
Both are hypothesized to facilitate anti-viral immunity, and patients with type O blood have both.
Unclear, new tighter-binding Spike protein.
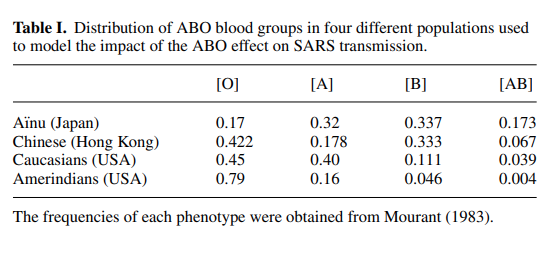
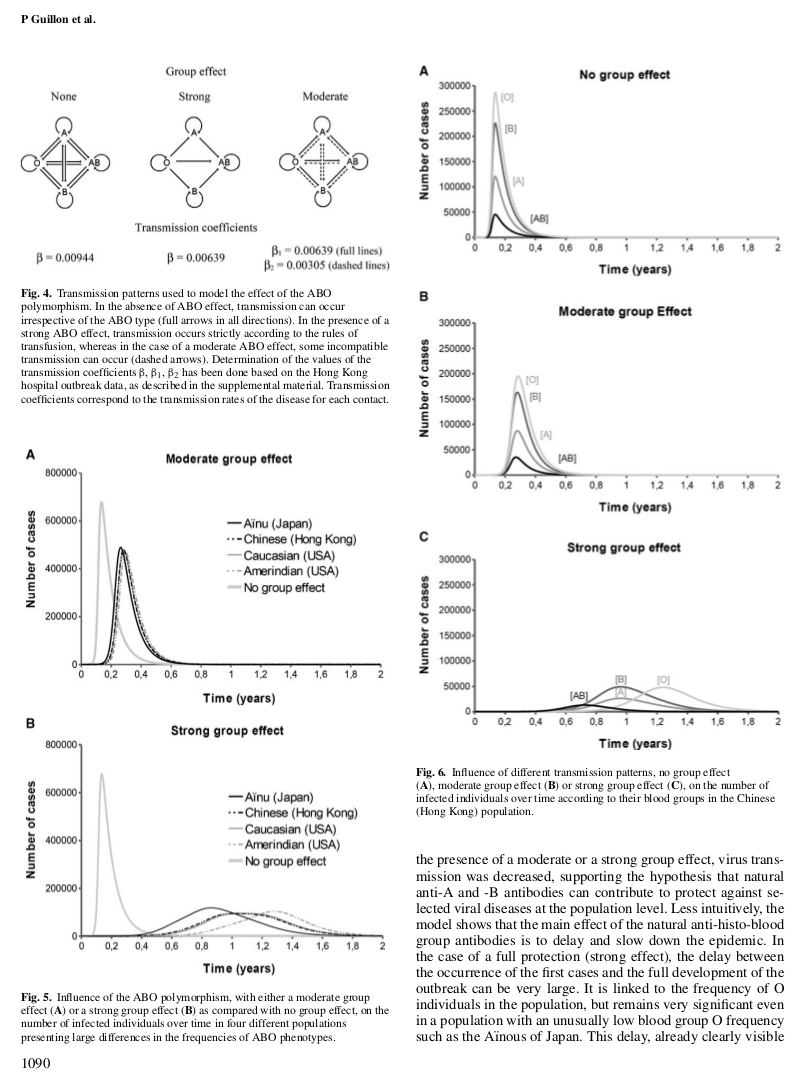
The authors observe that variation in blood type distributions by regional ancestry could have demographic implications for disease severity.
A simple model of the effect suggests SARS outbreaks in European-origin populations and developed countries might occur more rapidly.
A simple model of the effect suggests SARS outbreaks in European-origin populations and developed countries might occur more rapidly.
Empirically, though, it appears likely that public health measures, sanitation practices, social norms, and population age distributions explain much more of the observed international variation in differenced log case counts and the severity of such cases.
The authors also suggest that deliberate attempts to somehow increase the titer of anti-A or anti-B antibodies in patients with compatible blood types might provide another mechanism for slowing viral replication.
In summary: the blood type effect is likely real.
It has a plausible mechanism in SARS-CoV. Statistics for SARS-CoV-2 remain consistent.
This could have therapeutic implications-- but may require new methods, as raising ABO antibody levels is not usually considered desirable.
It has a plausible mechanism in SARS-CoV. Statistics for SARS-CoV-2 remain consistent.
This could have therapeutic implications-- but may require new methods, as raising ABO antibody levels is not usually considered desirable.

 Read on Twitter
Read on Twitter