Interesting preprint of the #LIVEAIR study of #lenzilumab in #COVID19:
-double blind RCT n=502 hospitalized pts on suppl O2
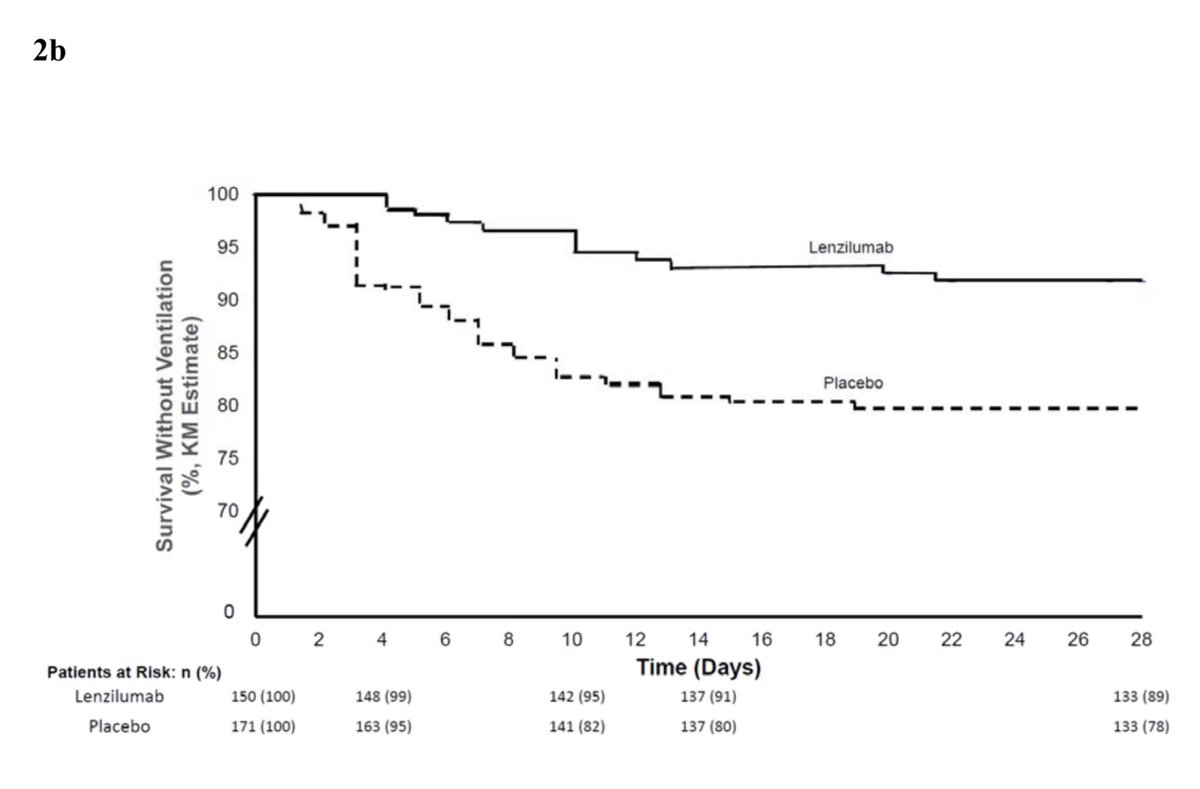
-lenzilumab associated with improved survival w/o ventilation: 84% vs 77.9%
-larger benefit when combined w/ steroids (NNT 10)
https://www.medrxiv.org/content/10.1101/2021.05.01.21256470v1.full.pdf
1/">https://www.medrxiv.org/content/1...
-double blind RCT n=502 hospitalized pts on suppl O2
-lenzilumab associated with improved survival w/o ventilation: 84% vs 77.9%
-larger benefit when combined w/ steroids (NNT 10)
https://www.medrxiv.org/content/10.1101/2021.05.01.21256470v1.full.pdf
1/">https://www.medrxiv.org/content/1...
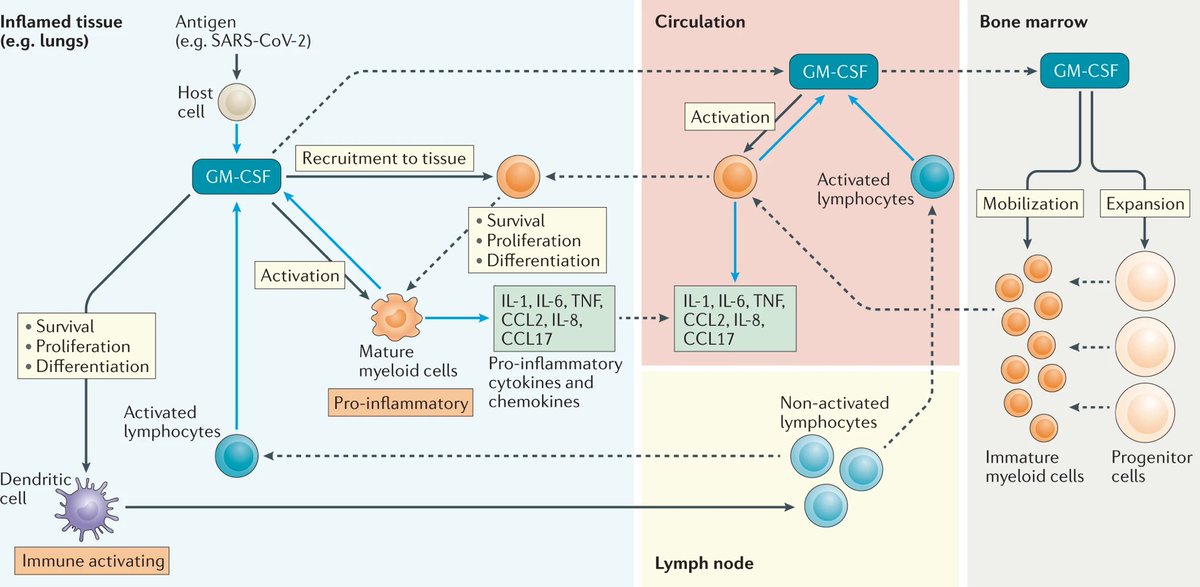
Context: GM-CSF is among the (many) cytokines upregulated in COVID & higher levels assoc w/ worse outcomes
https://pubmed.ncbi.nlm.nih.gov/33622974/
GM-CSF">https://pubmed.ncbi.nlm.nih.gov/33622974/... expressing Th17 cells are in BAL suggesting a role as mediators of lung injury
https://pubmed.ncbi.nlm.nih.gov/33622974/
So">https://pubmed.ncbi.nlm.nih.gov/33622974/... blocking GM-CSF makes sense https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤷" title="Mit Schultern zuckende Person" aria-label="Emoji: Mit Schultern zuckende Person">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤷" title="Mit Schultern zuckende Person" aria-label="Emoji: Mit Schultern zuckende Person">
2/
https://pubmed.ncbi.nlm.nih.gov/33622974/
GM-CSF">https://pubmed.ncbi.nlm.nih.gov/33622974/... expressing Th17 cells are in BAL suggesting a role as mediators of lung injury
https://pubmed.ncbi.nlm.nih.gov/33622974/
So">https://pubmed.ncbi.nlm.nih.gov/33622974/... blocking GM-CSF makes sense
2/
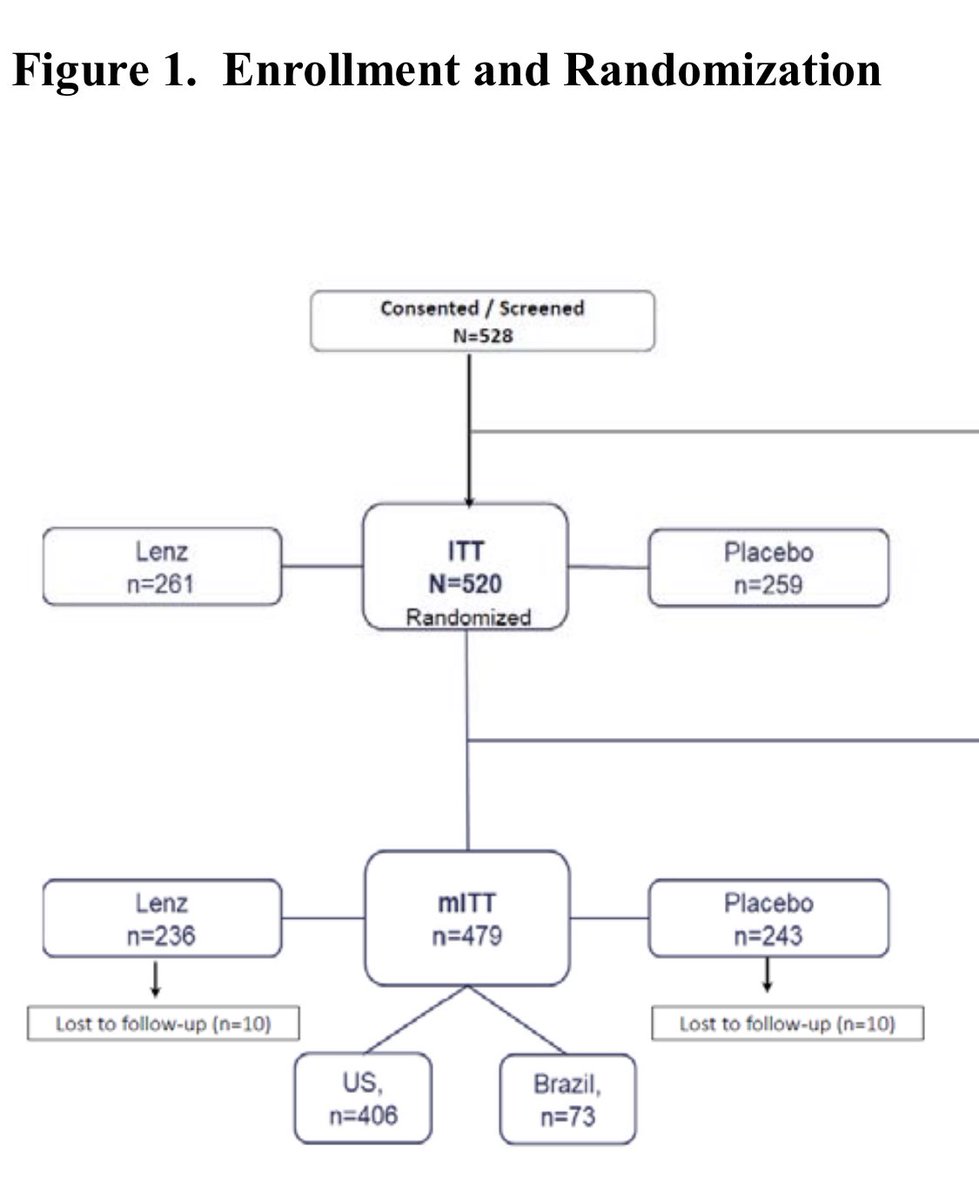
LIVE-AIR was a phase 3 placebo controlled RCT of lenzilumab (a humanized moAb against GM-CSF) at 29 sites in  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🇺🇸" title="Flagge der Vereinigten Staaten" aria-label="Emoji: Flagge der Vereinigten Staaten"> &
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🇺🇸" title="Flagge der Vereinigten Staaten" aria-label="Emoji: Flagge der Vereinigten Staaten"> &  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🇧🇷" title="Flagge von Brasilien" aria-label="Emoji: Flagge von Brasilien">.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🇧🇷" title="Flagge von Brasilien" aria-label="Emoji: Flagge von Brasilien">.
It enrolled Adults w/ COVID pneumonia who were hypoxemic: SpO2 < 94% on air and/or on NC, HFNC, or NIPPV. People w/ bacterial or fungal infxns were excluded.
3/
It enrolled Adults w/ COVID pneumonia who were hypoxemic: SpO2 < 94% on air and/or on NC, HFNC, or NIPPV. People w/ bacterial or fungal infxns were excluded.
3/
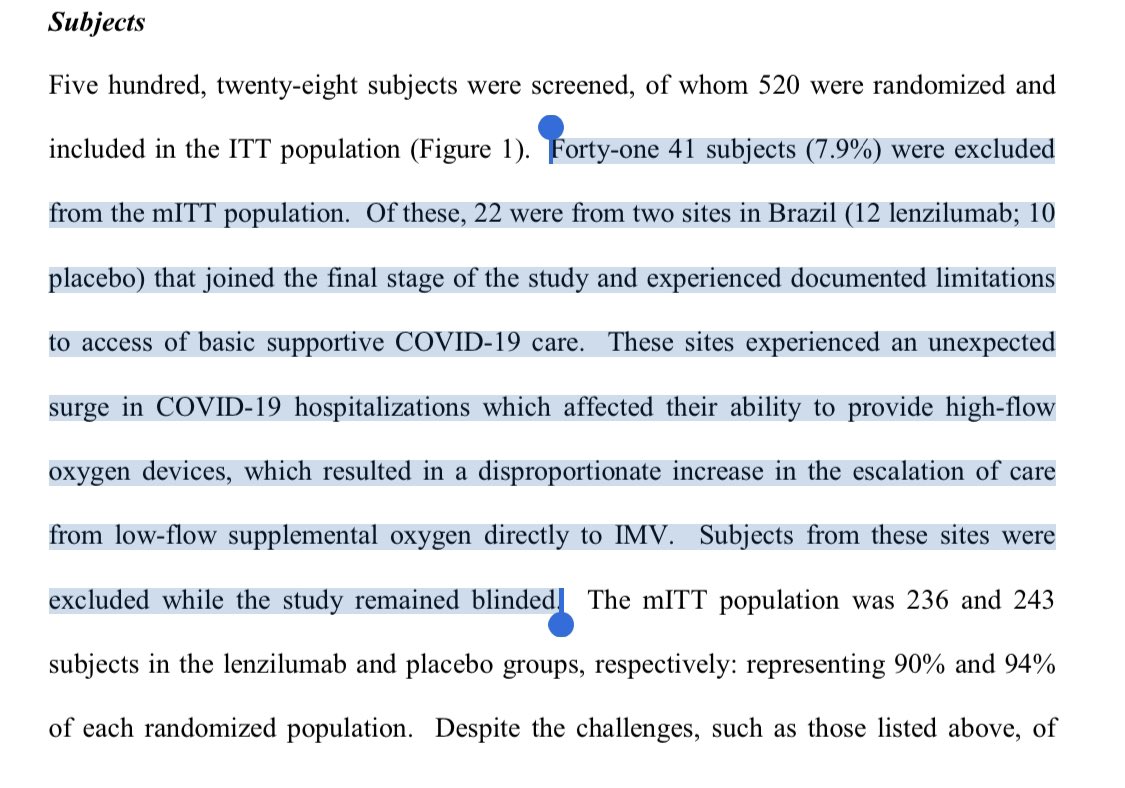
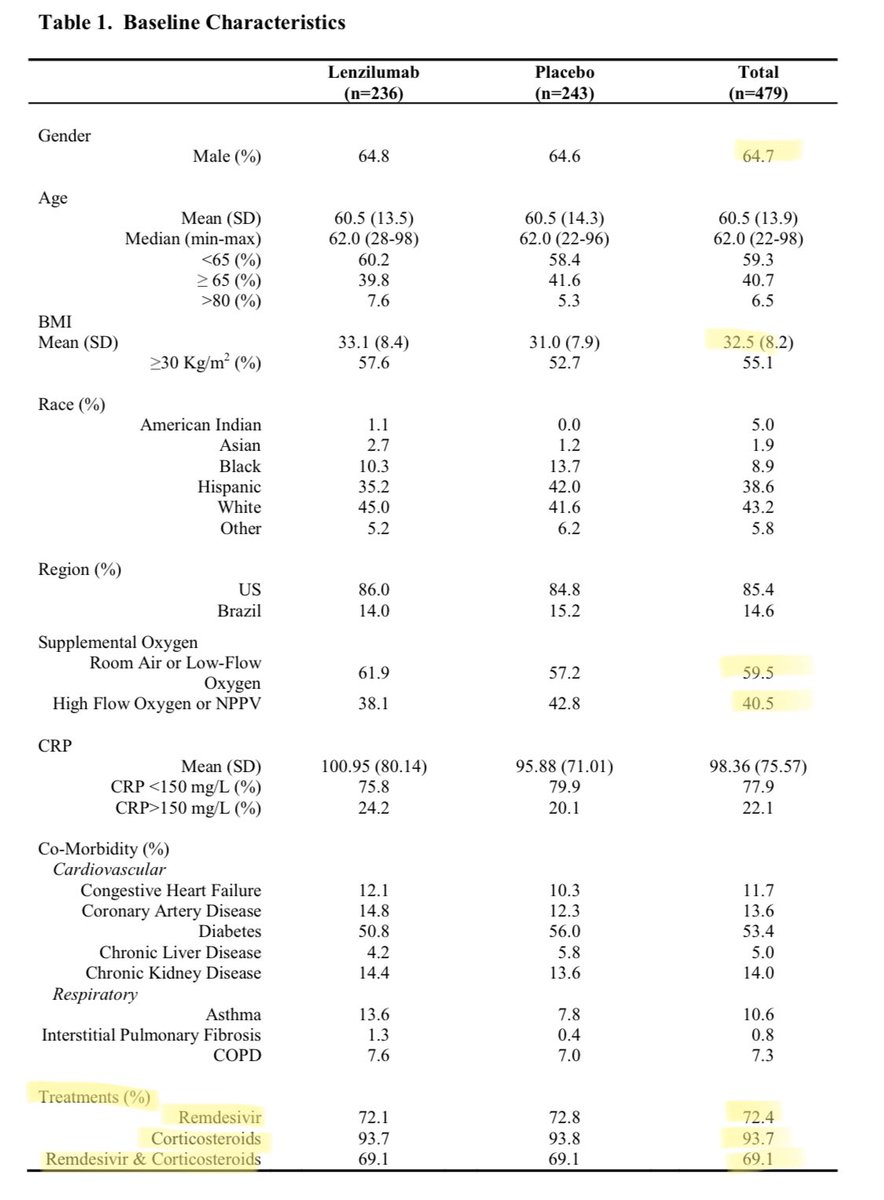
They enrolled 520 pts. Baseline characteristics were comparable. Most received steroids.
Big protocol deviations occurred at 1 site forcing them to drop 42 pts before unblinding, hence a modified ITT analysis. This happens (esp in a pandemic) & IMO doesn’t alter the results.
4/
Big protocol deviations occurred at 1 site forcing them to drop 42 pts before unblinding, hence a modified ITT analysis. This happens (esp in a pandemic) & IMO doesn’t alter the results.
4/
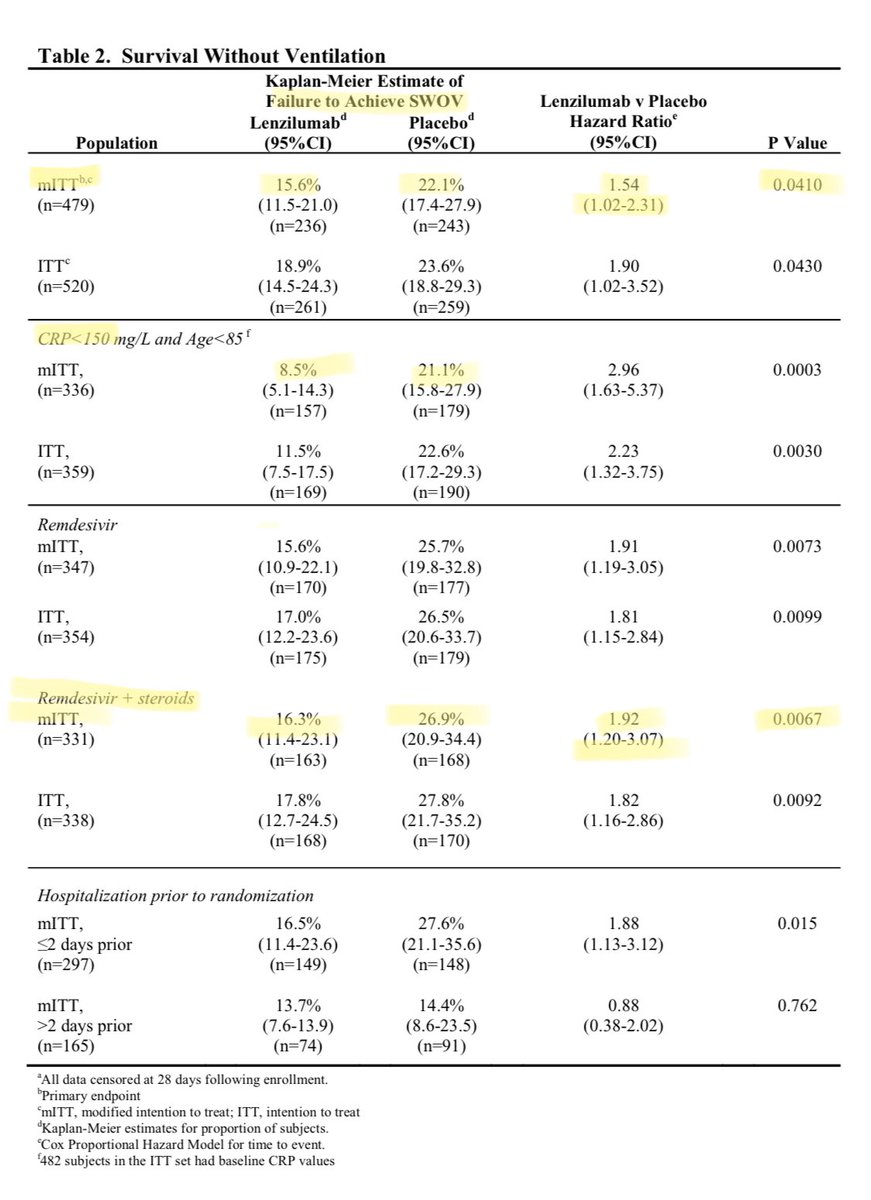
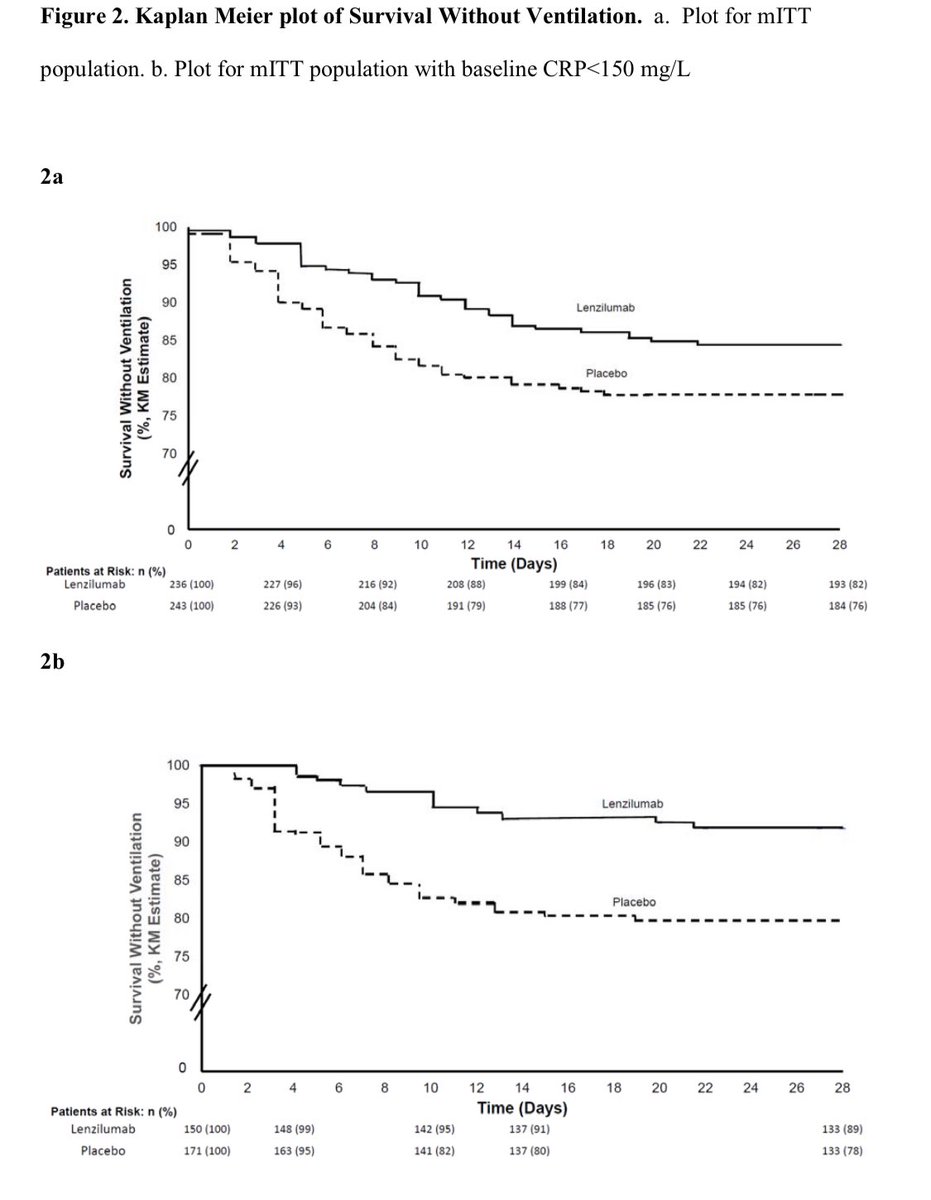
The 1° endpoint was Survival w/o ventilation (SWOV)
Lenzilumab improved SWOV a lot: a 6.5% reduction in the mITT analysis (NNT 15 to prevent death or intubation)
A larger effect was seen in pts with low CRP or on “standard of care” tx (remdesivir + steroids): 10.6% (NNT=9.4)
5/
Lenzilumab improved SWOV a lot: a 6.5% reduction in the mITT analysis (NNT 15 to prevent death or intubation)
A larger effect was seen in pts with low CRP or on “standard of care” tx (remdesivir + steroids): 10.6% (NNT=9.4)
5/
I’ll pause to share 2 pet peeves:
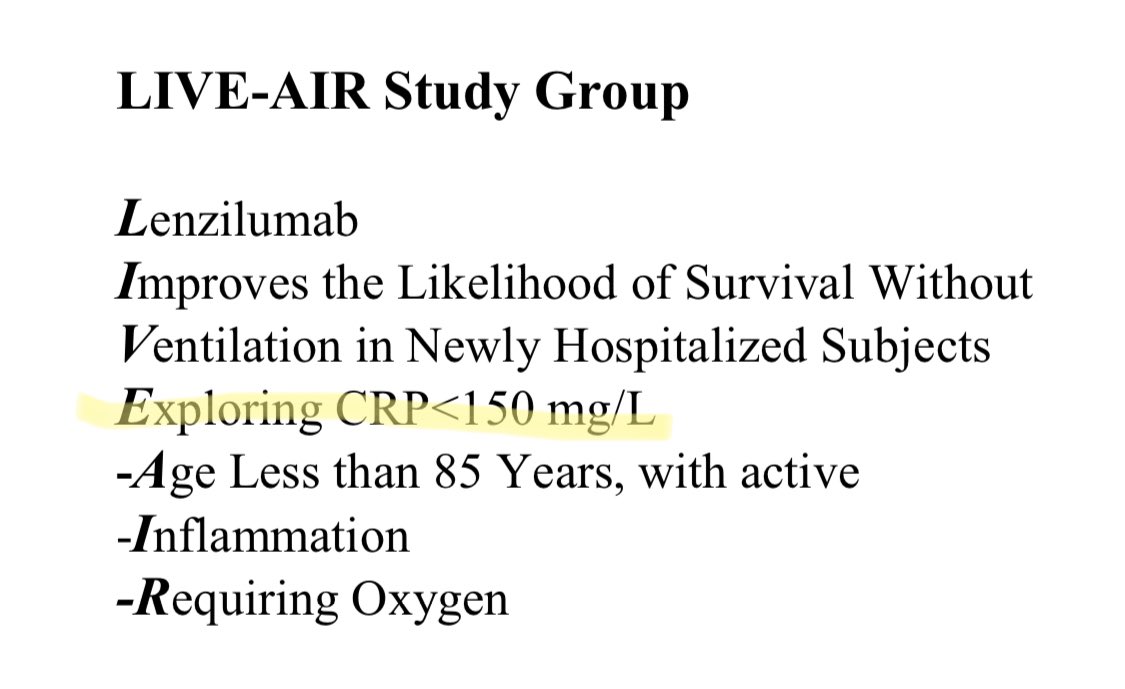
1. They were clearly focused on the low CRP subgroup a priori (it’s the “E” in the not so great backronym study name); Why didn’t they just make this an inclusion?
2. I HATE when authors interrupt the y axis on KM curves! This is deceptive!
6/
1. They were clearly focused on the low CRP subgroup a priori (it’s the “E” in the not so great backronym study name); Why didn’t they just make this an inclusion?
2. I HATE when authors interrupt the y axis on KM curves! This is deceptive!
6/
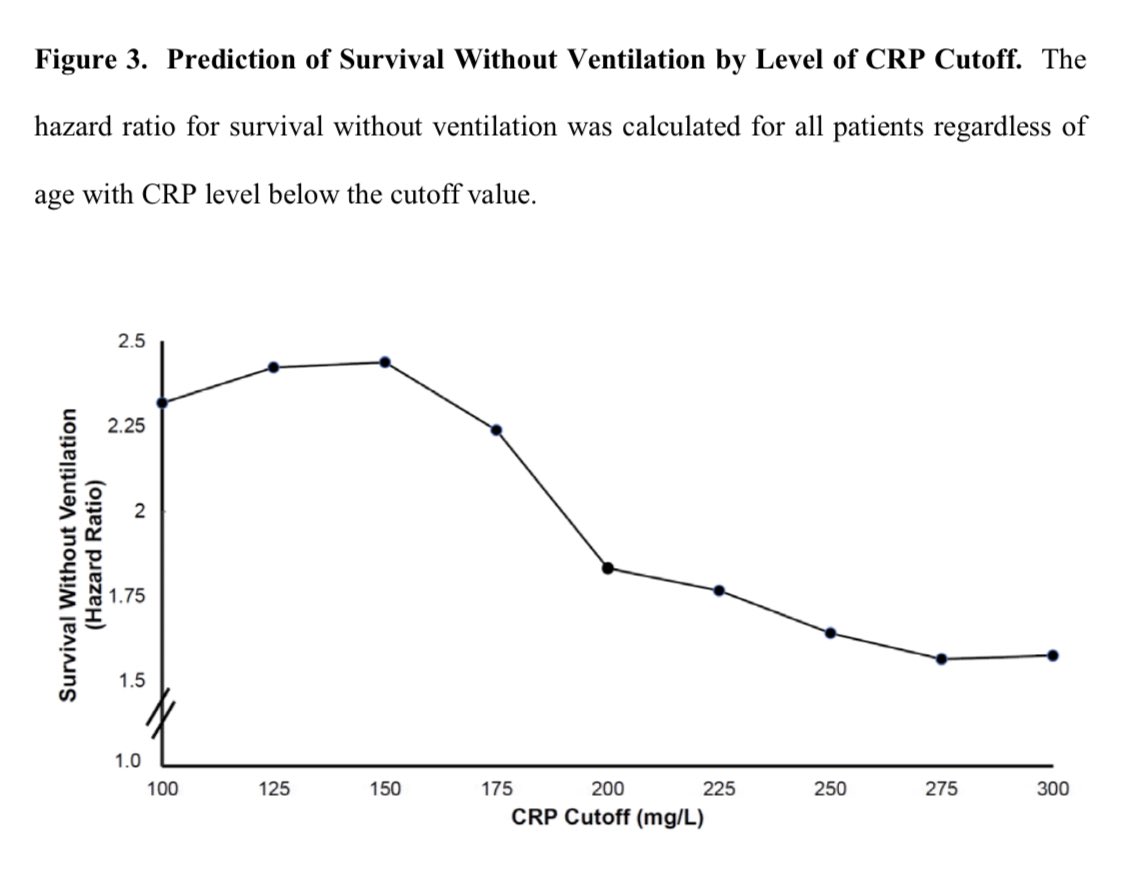
What to make of the greater benefit in pts CRP <150 mg/L?
It’s biologically plausible
If GM-CSF helps *initiate* inflammation, it makes sense that blocking GM-CSF might be more beneficial early. Low CRP *may* indicate earlier disease, though its also assoc w/ better survival
7/
It’s biologically plausible
If GM-CSF helps *initiate* inflammation, it makes sense that blocking GM-CSF might be more beneficial early. Low CRP *may* indicate earlier disease, though its also assoc w/ better survival
7/
Mortality was apparently 7.2% lower in patients with CRP <150 mg/dL who were treated with lenzilumab:
6.6% vs 13.8% (NNT 14 to save a life)
I’m reflexively highly skeptical about secondary endpoints in subgroups, but this is exciting. If replicated this is a big deal!
8/
6.6% vs 13.8% (NNT 14 to save a life)
I’m reflexively highly skeptical about secondary endpoints in subgroups, but this is exciting. If replicated this is a big deal!
8/
Recall that Tocilizumab (associated w mortality reduction in #RECOVERY) was most effective in HIGH CRP (>150).
Ironically after a year of asking “why do we keep checking all these CRPs” the distinction between low (<150) & high (>150) CRP may actually turn out to be useful.
9/ https://twitter.com/nickmmark/status/1359964191306567680">https://twitter.com/nickmmark...
Ironically after a year of asking “why do we keep checking all these CRPs” the distinction between low (<150) & high (>150) CRP may actually turn out to be useful.
9/ https://twitter.com/nickmmark/status/1359964191306567680">https://twitter.com/nickmmark...
It’s becoming clear that immunomodulatory therapies are beneficial in severe COVID
Increasingly it seems that combining steroids w/ other approaches like blocking cytokines (IL-6, GM-CSF) & downstream signaling (JAK) may further improve outcomes.
Still a lot we don’t know
10/
Increasingly it seems that combining steroids w/ other approaches like blocking cytokines (IL-6, GM-CSF) & downstream signaling (JAK) may further improve outcomes.
Still a lot we don’t know
10/
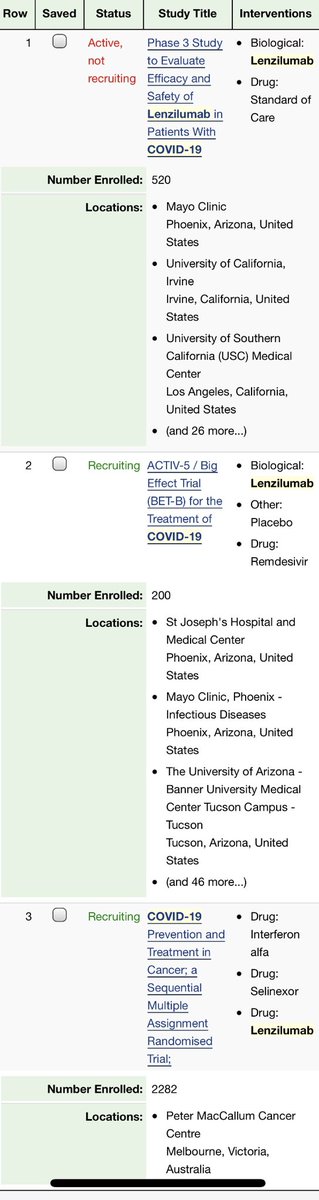
Importantly these impressive results should be replicated (or not) by 2 high quality RCTs relatively soon:
#ACTIV5 in the https://abs.twimg.com/emoji/v2/... draggable="false" alt="🇺🇸" title="Flagge der Vereinigten Staaten" aria-label="Emoji: Flagge der Vereinigten Staaten"> & arm 4 of #CSMART in
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🇺🇸" title="Flagge der Vereinigten Staaten" aria-label="Emoji: Flagge der Vereinigten Staaten"> & arm 4 of #CSMART in  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🇦🇺" title="Flagge von Australien" aria-label="Emoji: Flagge von Australien"> are both trialing lenzilumab
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🇦🇺" title="Flagge von Australien" aria-label="Emoji: Flagge von Australien"> are both trialing lenzilumab
https://www.clinicaltrials.gov/ct2/show/NCT04534725
https://www.clinicaltrials.gov/ct2/show/... href=" https://www.clinicaltrials.gov/ct2/show/NCT04583969
11/">https://www.clinicaltrials.gov/ct2/show/...
#ACTIV5 in the
https://www.clinicaltrials.gov/ct2/show/NCT04534725
11/">https://www.clinicaltrials.gov/ct2/show/...
-GM-CSF blockade w/ lenzilumab prevents intubations & mortality in hospitalized people with COVID who require O2
-it appears to have greater benefit in patients w/ low CRP (<150 mg/dL)
-this should change our practice, either now or when other studies conclude
12/12

 Read on Twitter
Read on Twitter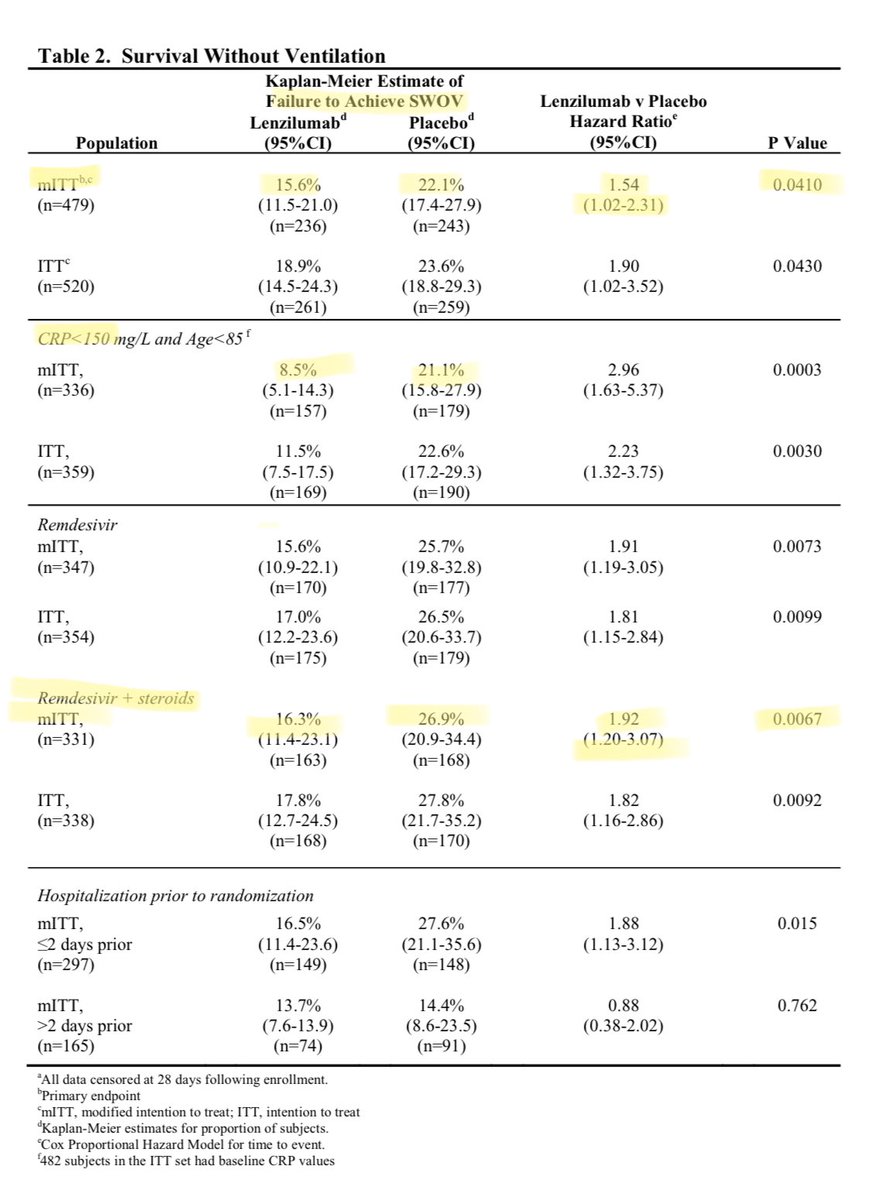

 2/" title="Context: GM-CSF is among the (many) cytokines upregulated in COVID & higher levels assoc w/ worse outcomes https://pubmed.ncbi.nlm.nih.gov/33622974/... expressing Th17 cells are in BAL suggesting a role as mediators of lung injury https://pubmed.ncbi.nlm.nih.gov/33622974/... blocking GM-CSF makes sensehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="🤷" title="Mit Schultern zuckende Person" aria-label="Emoji: Mit Schultern zuckende Person">2/" class="img-responsive" style="max-width:100%;"/>
2/" title="Context: GM-CSF is among the (many) cytokines upregulated in COVID & higher levels assoc w/ worse outcomes https://pubmed.ncbi.nlm.nih.gov/33622974/... expressing Th17 cells are in BAL suggesting a role as mediators of lung injury https://pubmed.ncbi.nlm.nih.gov/33622974/... blocking GM-CSF makes sensehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="🤷" title="Mit Schultern zuckende Person" aria-label="Emoji: Mit Schultern zuckende Person">2/" class="img-responsive" style="max-width:100%;"/>




 & arm 4 of #CSMART in https://abs.twimg.com/emoji/v2/... draggable="false" alt="🇦🇺" title="Flagge von Australien" aria-label="Emoji: Flagge von Australien"> are both trialing lenzilumab https://www.clinicaltrials.gov/ct2/show/... href=" https://www.clinicaltrials.gov/ct2/show/NCT0458396911/">https://www.clinicaltrials.gov/ct2/show/..." title="Importantly these impressive results should be replicated (or not) by 2 high quality RCTs relatively soon: #ACTIV5 in the https://abs.twimg.com/emoji/v2/... draggable="false" alt="🇺🇸" title="Flagge der Vereinigten Staaten" aria-label="Emoji: Flagge der Vereinigten Staaten"> & arm 4 of #CSMART in https://abs.twimg.com/emoji/v2/... draggable="false" alt="🇦🇺" title="Flagge von Australien" aria-label="Emoji: Flagge von Australien"> are both trialing lenzilumab https://www.clinicaltrials.gov/ct2/show/... href=" https://www.clinicaltrials.gov/ct2/show/NCT0458396911/">https://www.clinicaltrials.gov/ct2/show/..." class="img-responsive" style="max-width:100%;"/>
& arm 4 of #CSMART in https://abs.twimg.com/emoji/v2/... draggable="false" alt="🇦🇺" title="Flagge von Australien" aria-label="Emoji: Flagge von Australien"> are both trialing lenzilumab https://www.clinicaltrials.gov/ct2/show/... href=" https://www.clinicaltrials.gov/ct2/show/NCT0458396911/">https://www.clinicaltrials.gov/ct2/show/..." title="Importantly these impressive results should be replicated (or not) by 2 high quality RCTs relatively soon: #ACTIV5 in the https://abs.twimg.com/emoji/v2/... draggable="false" alt="🇺🇸" title="Flagge der Vereinigten Staaten" aria-label="Emoji: Flagge der Vereinigten Staaten"> & arm 4 of #CSMART in https://abs.twimg.com/emoji/v2/... draggable="false" alt="🇦🇺" title="Flagge von Australien" aria-label="Emoji: Flagge von Australien"> are both trialing lenzilumab https://www.clinicaltrials.gov/ct2/show/... href=" https://www.clinicaltrials.gov/ct2/show/NCT0458396911/">https://www.clinicaltrials.gov/ct2/show/..." class="img-responsive" style="max-width:100%;"/>


