Can the the absence of evidence of in-school transmission be taken as evidence of absence?
This is the question that @KaitEJohnson9, @mikha_ehl, M. Stoddard, R. Pasco, Spencer Fox, L. Meyers ( @meyerslab) and A. Chakravarty address in this preprint. https://www.medrxiv.org/content/10.1101/2021.04.26.21256136v1">https://www.medrxiv.org/content/1...
This is the question that @KaitEJohnson9, @mikha_ehl, M. Stoddard, R. Pasco, Spencer Fox, L. Meyers ( @meyerslab) and A. Chakravarty address in this preprint. https://www.medrxiv.org/content/10.1101/2021.04.26.21256136v1">https://www.medrxiv.org/content/1...
They aim straight at the core of the claims that in-person schooling have not amplified SARS-CoV-2 transmission based on the observation of similar infection rates in schools and communities and limited numbers of documented in-school transmission events.
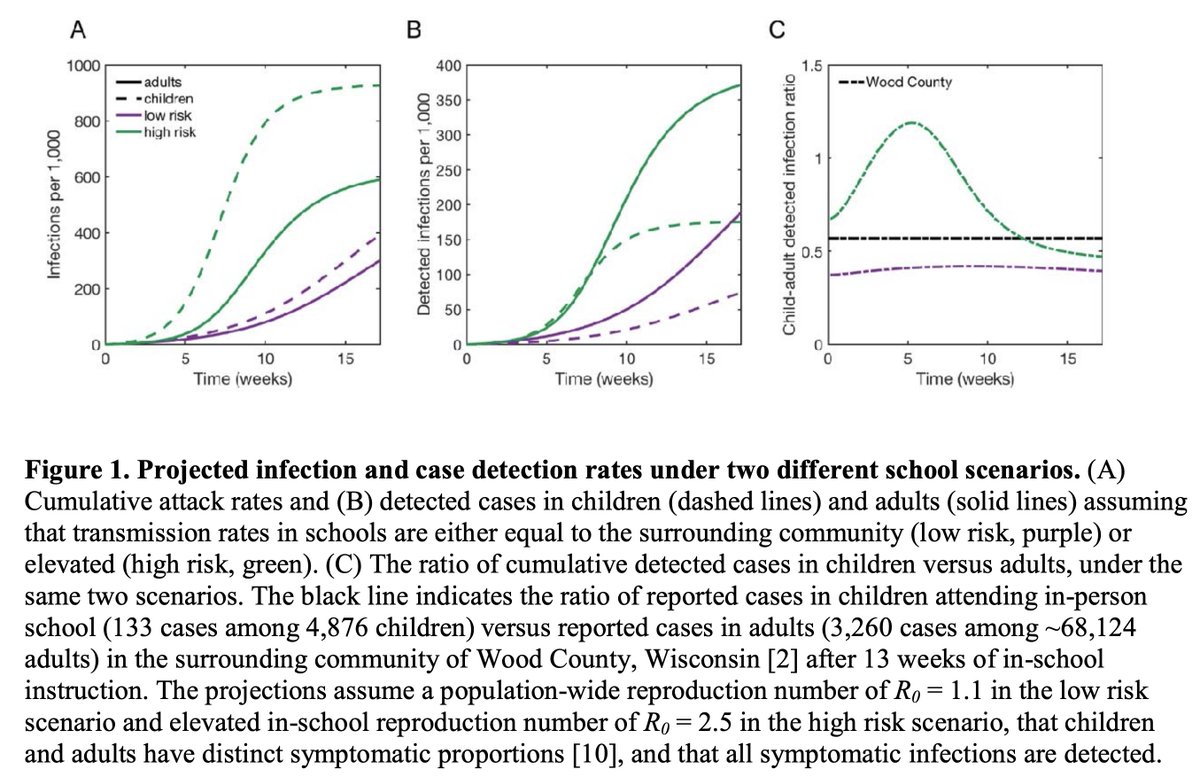
This very interesting simulation study models age-specific transmission scenarios of both high [R2.5] and low [R1.1] in-school transmission, but accounts for the known low case detection rates in children based on lower probability of symptoms, and the SARS-CoV-2 over dispersion.
The simulations suggest that even with high infection rates among children (green lines below), the ratio of child to adult cases tends to drop to well below 1 over time, suggesting that even when schools amplify transmission, a low ration of child to adult cases may be observed.
Why does this happen?
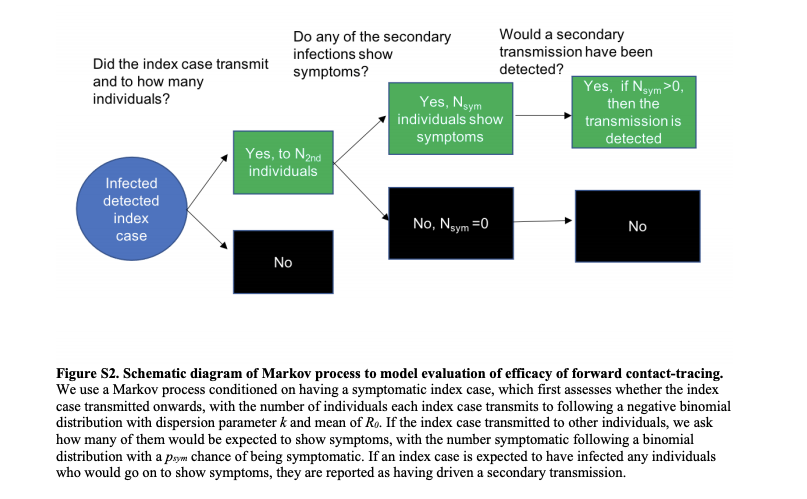
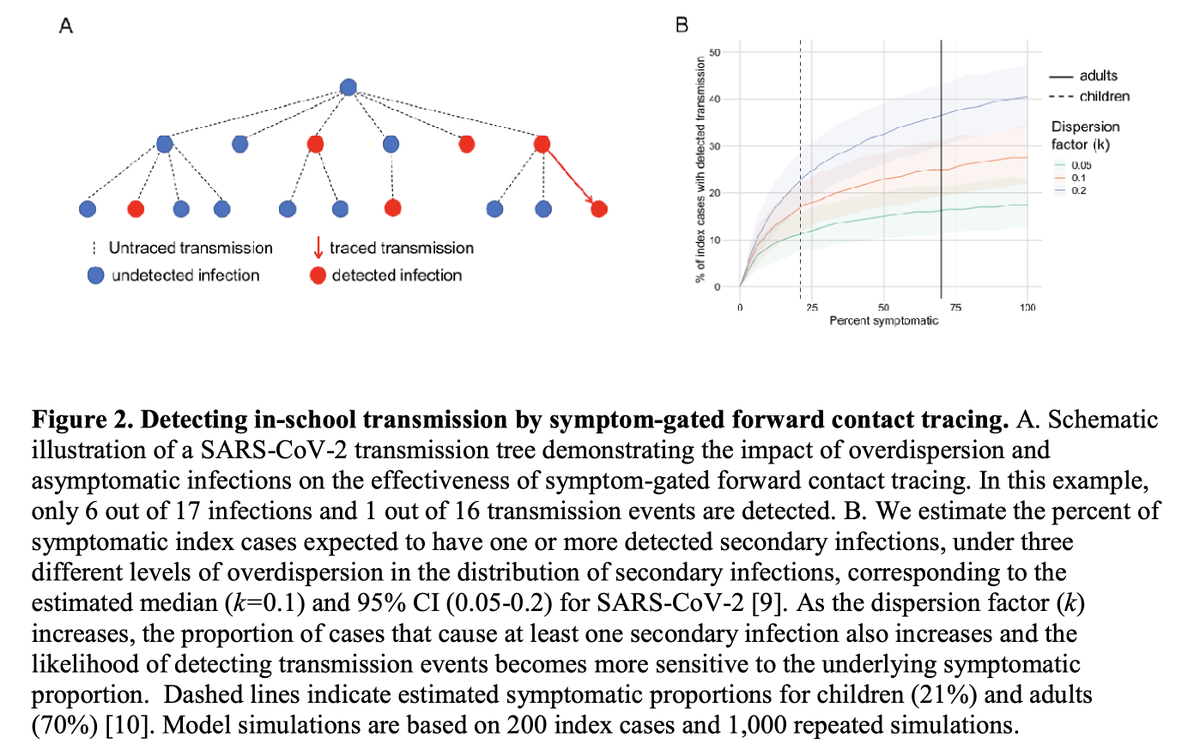
In a second analysis, the authors estimate the probability of detecting school outbreaks via symptom-gated forward contact tracing. This child-to-child transmission detection criteria requires 2 or more symptomatic consecutive cases, epidemiologically linked (transmission event).
As we know, symptom detection in children is less likely than adults (authors assumed 21% symptomatic), therefore the probability of detection of transmission events (i.e. 2 consecutive cases in school is only 4.4% (0.21*0.21)).
I would add that the probability of detecting a school outbreak is much lower when transmission events are ruled out due to distance, time, environment and PPE/masks use criteria for epidemiological linkage. It may reduce the proportion of events detected to less than 1%.
When accounting for the known overdispersion (most cases do not infect others), the probability of detecting a symptomatic kid infecting another kid that also becomes symptomatic is only 16.5%. The low number of school outbreaks detected are a & #39;feature& #39; of the contact tracing.
That is why neither the ratio of cases in and out of schools nor low numbers of documented in-school transmission events (outbreaks) are sufficient to distinguish scenarios of high or low in-school transmission. This is what we have been saying all along, not nearly as elegantly.
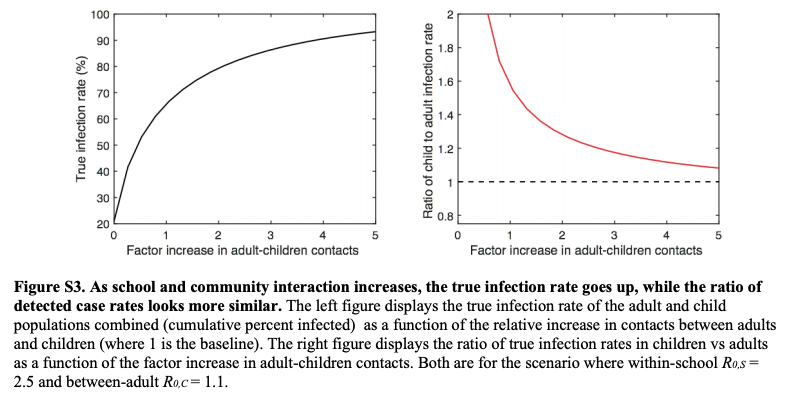
In a sensitivity analysis, increasing child-adult contacts increases the number of infections but that the symptom-gated testing makes it appear that school infection rates are lower than in the community, even when schools are driving transmission in the population.
The authors conclude that these metrics (low ratio of infection rates in children compared to adults, and the lack of detected in-school outbreaks) cannot exclude the possibility that transmission in schools exacerbated overall pandemic risks.
"While there are compelling arguments for returning to in-person learning, particularly as SARS-CoV-2 vaccine coverage increases, a robust understanding of the limitations of the metrics being used to assess SARSCoV-2 transmission is critical for risk management."
Could not find the handles for M. Stoddard, R. Pasco, Spencer Fox, L. Meyers and A. Chakravarty (will tag them if anyone points to it).

 Read on Twitter
Read on Twitter