Good evening everyone and welcome to tonight& #39;s case based discussion!  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧠" title="Gehirn" aria-label="Emoji: Gehirn"> tonight we have @AFAlalade from @PrestonNeuro as our moderator. Follow this thread and join in the discussion! Look out for the code word required for certificates/feedback form at the end..lets get started!
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧠" title="Gehirn" aria-label="Emoji: Gehirn"> tonight we have @AFAlalade from @PrestonNeuro as our moderator. Follow this thread and join in the discussion! Look out for the code word required for certificates/feedback form at the end..lets get started!
1. A 53-year-old female presents to the neurosurgery outpatient clinic with an 8 month history of right-sided progressive hearing loss and nonpulsatile tinnitus. She has a PMH of T1DM but is otherwise well.
Based on the history, what are your thoughts on a differential diagnosis?
3. Good stuff guys! Infectious: e.g. otitis externa resulting in conductive hearing loss, viral labyrinthitis Traumatic: perforation of tympanic membrane, cholesteatoma Neoplastic: vestibular schwannoma, CPA meningioma, CPA neuroma
4. Idiopathic: Presbycusis, Meniere’s disease, otosclerosis Autoimmune: MS. Drug induced: e.g. aminoglycosides, diuretics.
5. You go on to take a more comprehensive history. The patient reports no nausea or vomiting, no LOC or seizures, and no weakness of UL/LL or facial weakness. She does report to feeling dizzy at times and some loss of balance...
6. The patient has no visual disturbances and only has occasional headaches. She reports her hearing in her left ear has been fine but the right ear has been worsening. As such she has been using a hearing aid for the past couple of months.
7. Are there any examinations you’d like to perform?
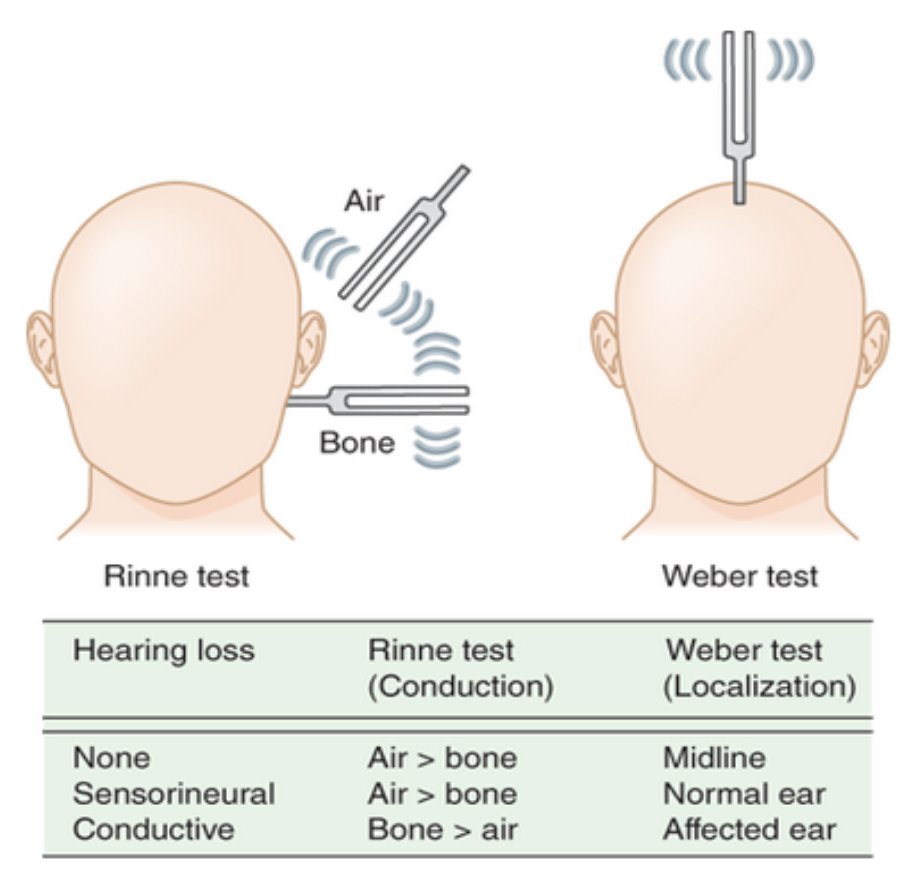
8. Comprehensive UL/LL neurological examination and cranial nerve examination. Ear examination and hearing test including Rhine’s and Weber’s. Audiometric (pure tone audiogram and speech discrimination) is a useful test to determine the type and also the degree of hearing loss
9. Great to see some new faces! So... O/E CN’s I-VII and IX-XII are grossly intact. There is no focal neurology on UL/LL examination. Pupils are equal and reactive to light, corneal reflex is intact and there is no facial asymmetry.
10. The external acoustic meatus is unremarkable and the tympanic membrane is intact with the handle of the malleus clear and no sign of effusion or retraction. You go on to perform Rinne and Weber’s test...
11. Rinne’s test shows air conduction > bone conduction in both the right and left ear. Weber’s test lateralized to the left. What is the significance of this result?
12. This implies right sensorineural deafness. In Weber’s test if there is a sensorineural deafness then the sound localises to the unaffected side. Here is a useful schematic demonstrating this well..
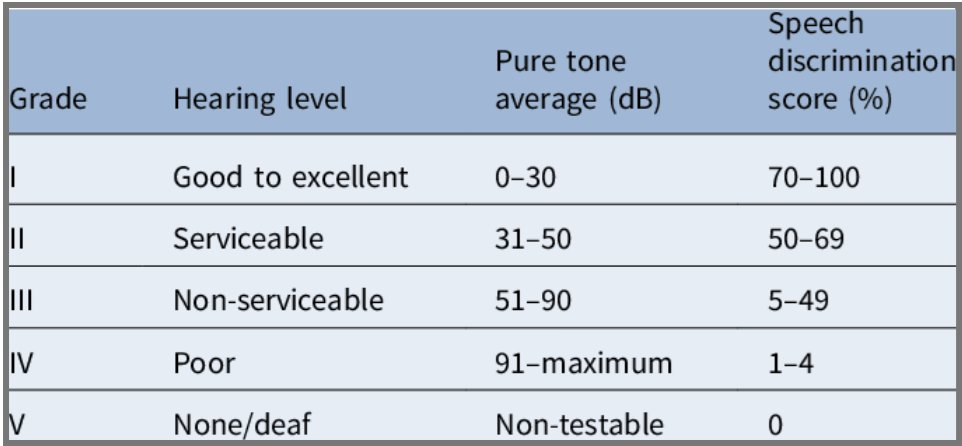
13. An audiogram is performed which demonstrates a high-frequency hearing loss on the right ear. The left ear is otherwise normal. Do you know any grading systems we can use for hearing?
14. Gardner and Robertson! Here’s the modified grading system below. To differentiate between Class I and Class II, class I can hear with a mobile phone on that side; whilst class II can localise the sound.
15. Based on the above findings, what are your thoughts now about the diagnosis?
16. The symptoms the patient is experiencing alone with the examination findings point towards sensorineural deafness. What will you do now to investigate this?
17. An MRI head with and without contrast is performed. MRI scans have become the gold standard imaging test and are especially useful for detecting soft tissue masses. Below is the result of the MRI head, what do you see?
18. This is an MRI head with contrast. The axial T2 image shows a mass in the right cerebellopontine angle. Can anyone describe what the cerebella-pontine angle is?
19. The cerebellopontine angle is a triangular space located posterior to the pyramid, inferior to the tentorium, lateral to the pons, and ventral to the cerebellum. It is formed by the superior and inferior limbs of the cerebellopontine fissure.
20. The CPA is occupied by the CPA cistern. This is essentially a triangular CSF filled subarachnoid cistern which lies between anterior surface of cerebellum and lateral surface of pons.
21. This comprises CN VII, CN VIII, flocculus of the cerebellum, and the choroid plexus, protruding through foramen of Luschka and AICA (anterior inferior cerebellar artery). CN V lies superior and CN IX, X and XI lie inferior to the CPA cistern.
22. Here is the image again. You’ll notice there are areas of hyperintense signal and hypointense signal. We call this heterogeneous in signal.
23. If you look closely you’ll see the tissue extends into the internal acoustic meatus. Who can tell us what nerves run through the internal acoustic meatus?
24. There are actually 5 nerves which run through the IAM! These are (1) nervus intermedius (sensory component of VII). (2) facial motor root VII, (3)cochlear nerve VIII (4) inferior vestibular nerve (VIII) (5) superior vestibular nerve (VIII).
25. Let’s explore some anatomy shall we? Within the IAM, these nerves mainly run in the lateral portion. The lateral portion is split into the superior and inferior portions by the falciform crescent.
26. In the superior portion we have the facial nerve and superior vestibular nerve (SVN); the facial nerve is anterior to the SVN and is separated from it laterally by a vertical ridge of bone, called Bill’s Bar.
27. In the inferior portion we have cochlear nerve and inferior vestibular nerve (IVN), the cochlear nerve is situated anteriorly. You may have heard the acronym 7 up, coke down? That helps with the location of CN VII and CN VIIIc.
28. What do you think the likely diagnosis is? Do you know of any other CPA lesions which can be common?
29. Some examples include meningioma, ependymoma, metastasis. So, do you know what the characteristic features of vestibular schwannoma are?
30. On imaging, they present with an intracanalicular component and widening of the porus acousticus..
31. Vestibular schwannomas are benign Schwann cell sheath tumours (WHO I) which arise from the inferior division of the vestibular nerve. Vestibular schwannoma arises as a result of the loss of tumour suppressor gene on the long arm of chromosome 22
32. Does anyone know of any genetic condition which can result in bilateral vestibular schwannomas?
33. Yes! Neurofibromatosis Type 2 (NF-2). This is a rare genetic disorder, it can be inherited or arise spontaneously. It affects 1 in 100,000 and also can cause multiple intracranial schwannomas, meningiomas and ependymomas.
34. You discuss the findings with the patient and present the options. What options are there for the treatment of vestibular schwannoma?
35. Management consists of (1) expectant management which is following the symptoms, audiometry and monitoring the tumour growth on serial imaging. Some may show little or no growth, slow growth which is ~2mm/ year or rapid growth ~10mm/ year.
36. (2)Radiotherapy alone or combined with surgery. This is usually in the form of stereotactic radiosurgery and can be a single dose or fractionated. (3) Surgical management or (4) chemotherapy.
37. There are several factors which influence the decisions for management. Can you think of a few? (Hint, Mr Alalade has discussed some of these already!)
38. Good ideas guys! Some factors include the hearing in the contralateral ear, size of the tumour, natural growth history of the tumour and natural history of hearing function
39. Quick pause! The code word for this week& #39;s feedback is & #39;dizzy& #39;. For certificates - input this into the feedback form which will be posted at the end of the thread  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🙂" title="Leicht lächelndes Gesicht" aria-label="Emoji: Leicht lächelndes Gesicht">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🙂" title="Leicht lächelndes Gesicht" aria-label="Emoji: Leicht lächelndes Gesicht">
40. You discuss the findings with the patient. She is keen to undergo surgical management. You counsel her on some of the complications. What complications of surgery can you think of?
41. Facial nerve palsy, hearing loss, injury to cranial nerves, CSF leak. Facial nerve palsy is actually one of the most common complications following this surgery.
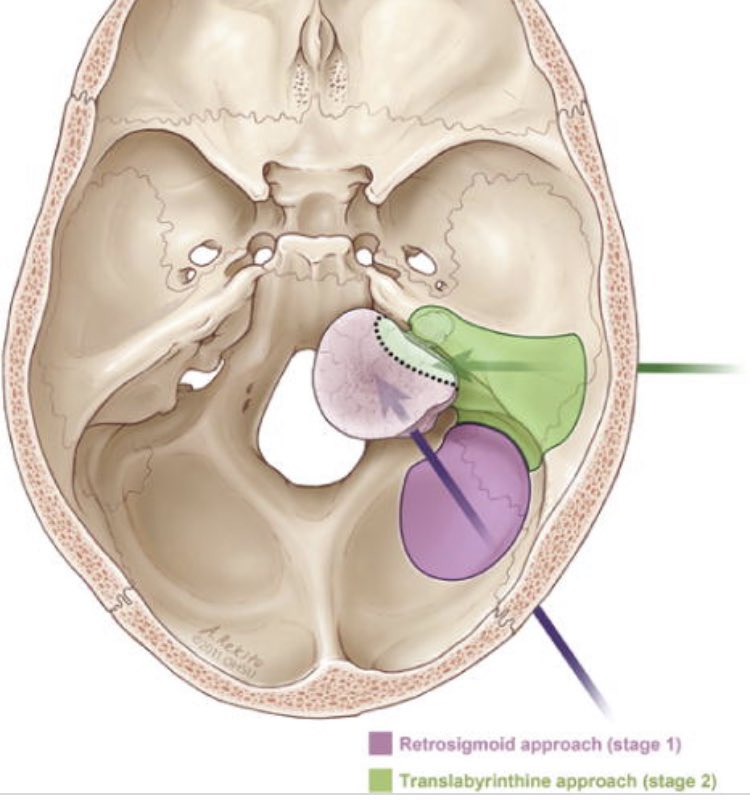
42. What surgical options do you know? Are there any pros and cons for the different options?
43. This was a tough one! @AFAlalade has shared a fab picture to demonstrate the approaches
44. How would you position the patient? Are you aware of the important surgical landmarks or any preoperative investigations that would be necessary?
45. The following month the patient is brought in for surgery. Her pre-op assessment is fine and she is prepared for surgery. Are there any specialties you’d like to involve for the surgery?
46. ENT surgeons and Neuro-physiology! It’s important to undertake neuro-monitoring through the surgery, particularly as you’re in a very eloquent area with a number of cranial nerves.
47. Typically CN’s V, VII, VIII, IX, X, XI, XII are monitored. The neuromonitoring could also involve the long tracts (corticospinal tracts), SSEP and brainstem auditory evoked potentials.
48. For monitoring the trigeminal nerve (nerve V), needle electrodes are placed into the masticator muscles (masseter, temporalis).
49. Function of CN VII muscles (nerve VII, facial nerve EMG) is recorded using steel needle electrodes inserted subd dermally into the orbicularis muscles of the eyes and mouth for two channel recordings.

 Read on Twitter
Read on Twitter