Happy to share the latest paper from our team in @nature
A comprehensive characterization of post acute sequelae of COVID-19
#longcovid #PASC
https://www.nature.com/articles/s41586-021-03553-9
https://www.nature.com/articles/... href="https://twitter.com/VAResearch">@VAResearch @vahsrd @WUSTL @WUSTLpubhealth @WUSTLmed @WUSTLnews @VREFSTL @Biostayan @BCBowe
A comprehensive characterization of post acute sequelae of COVID-19
#longcovid #PASC
https://www.nature.com/articles/s41586-021-03553-9
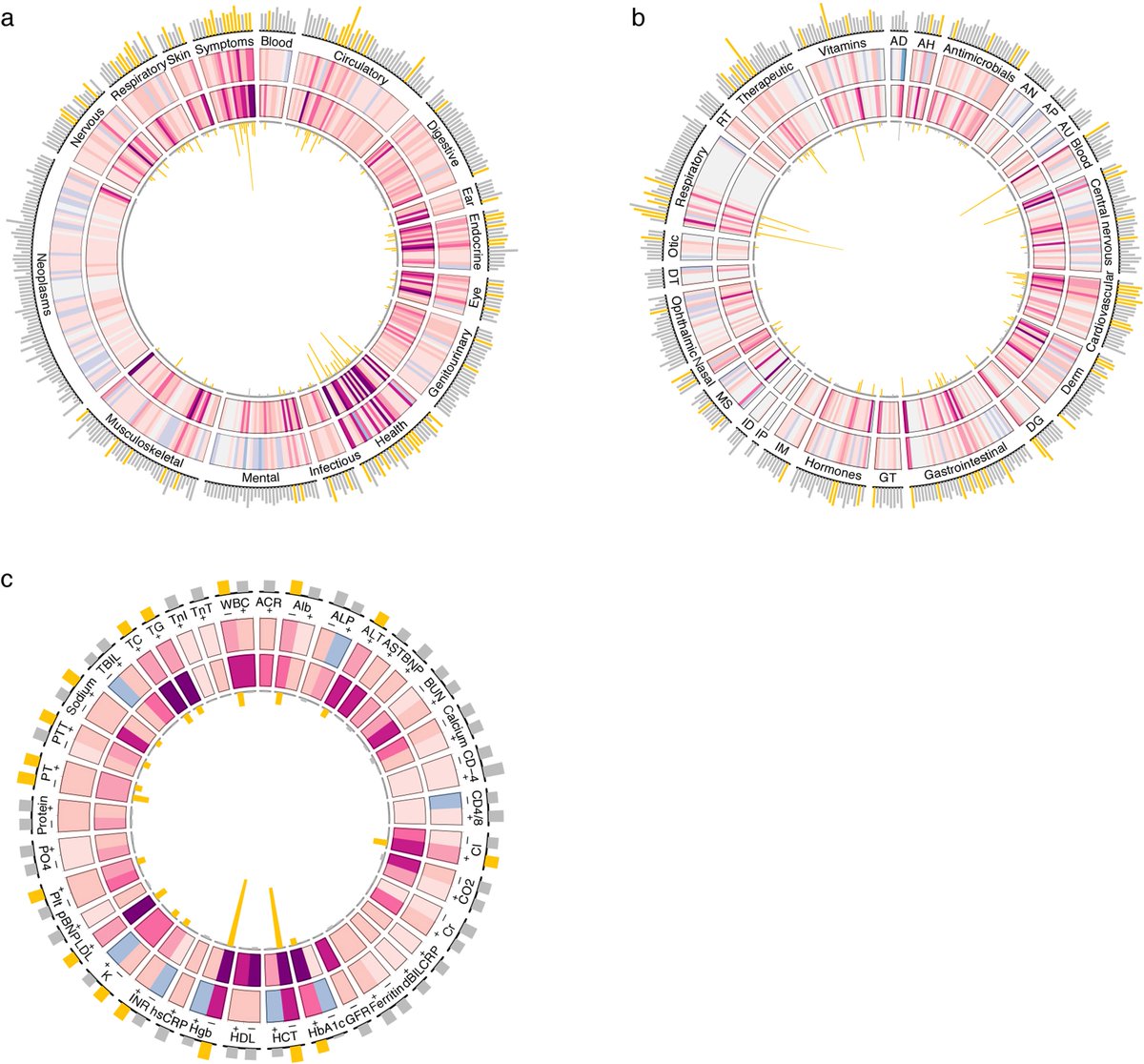
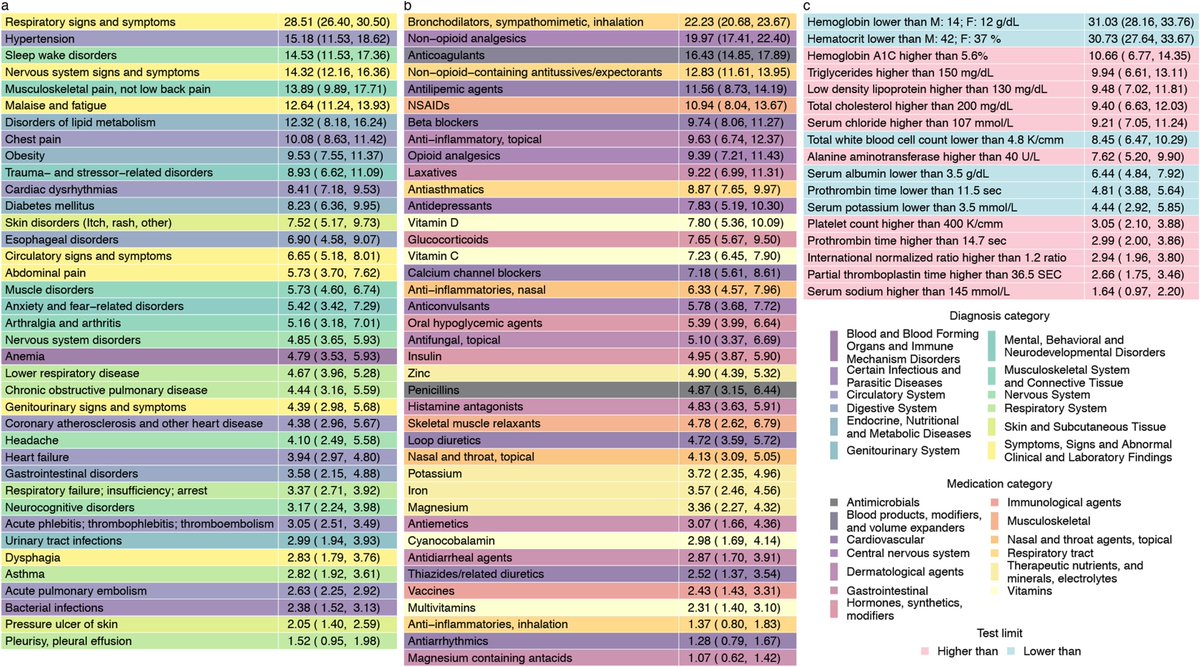
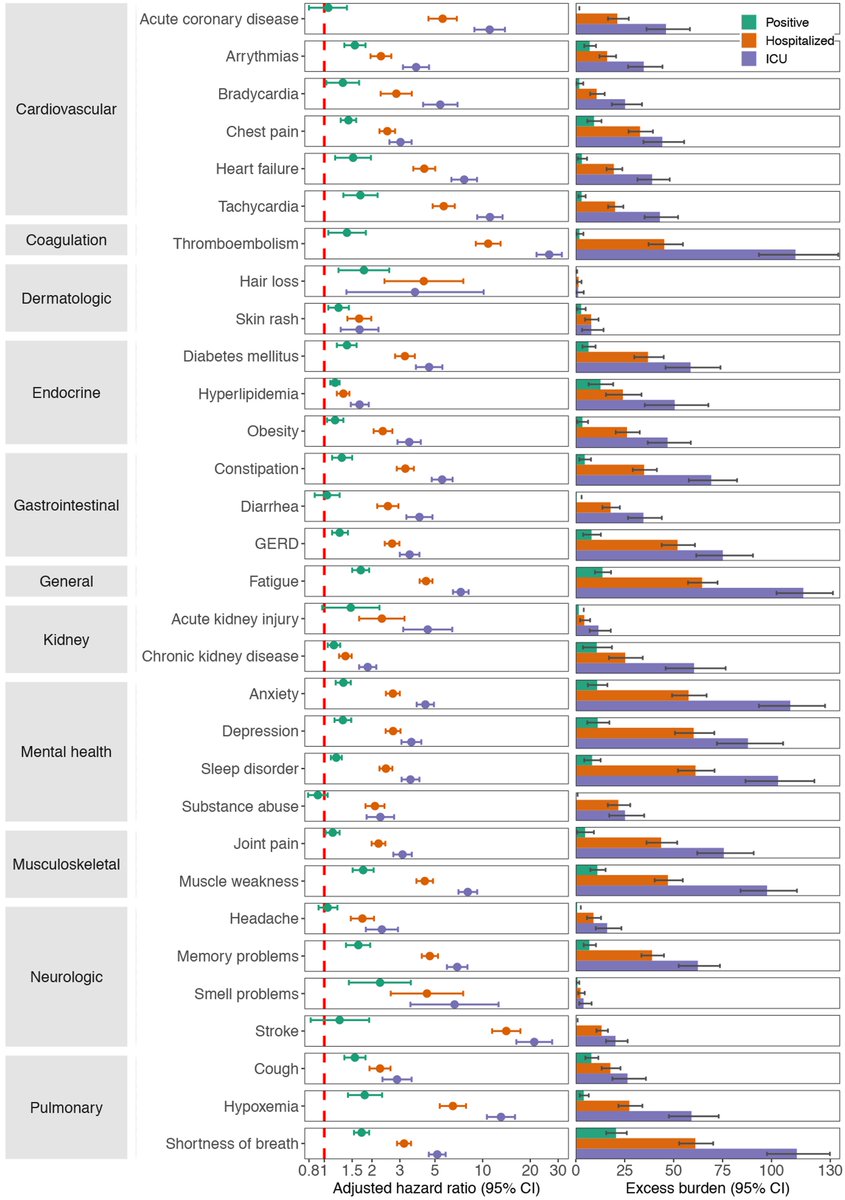
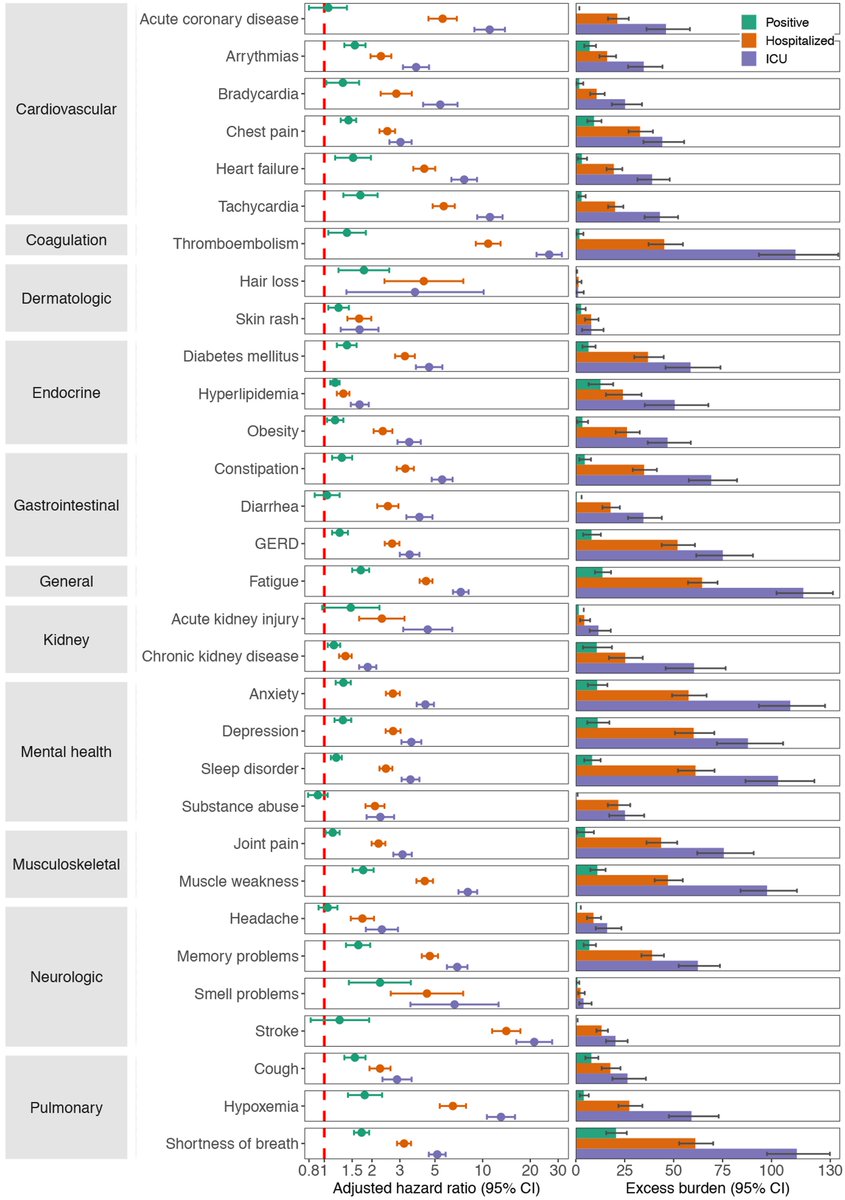
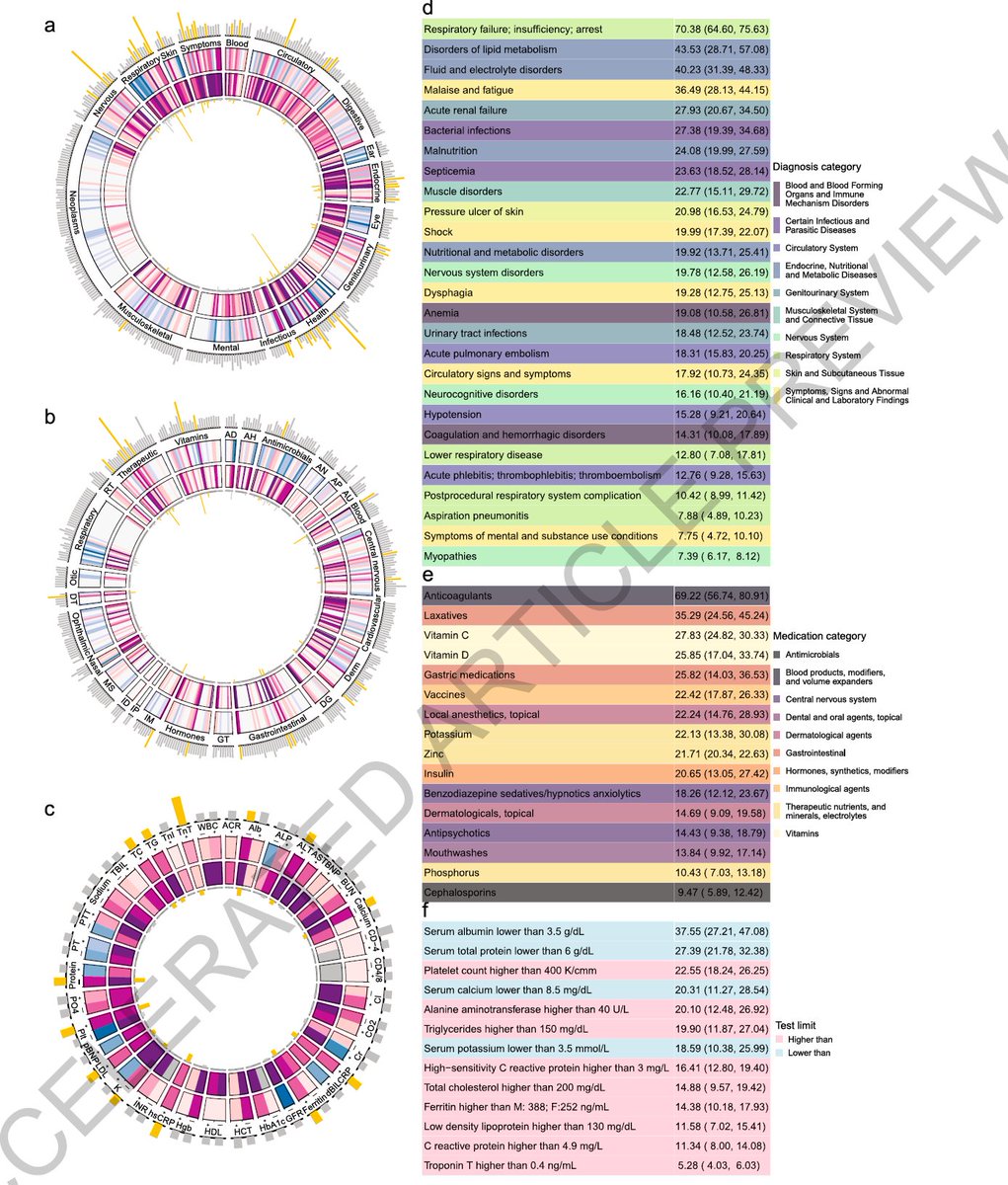
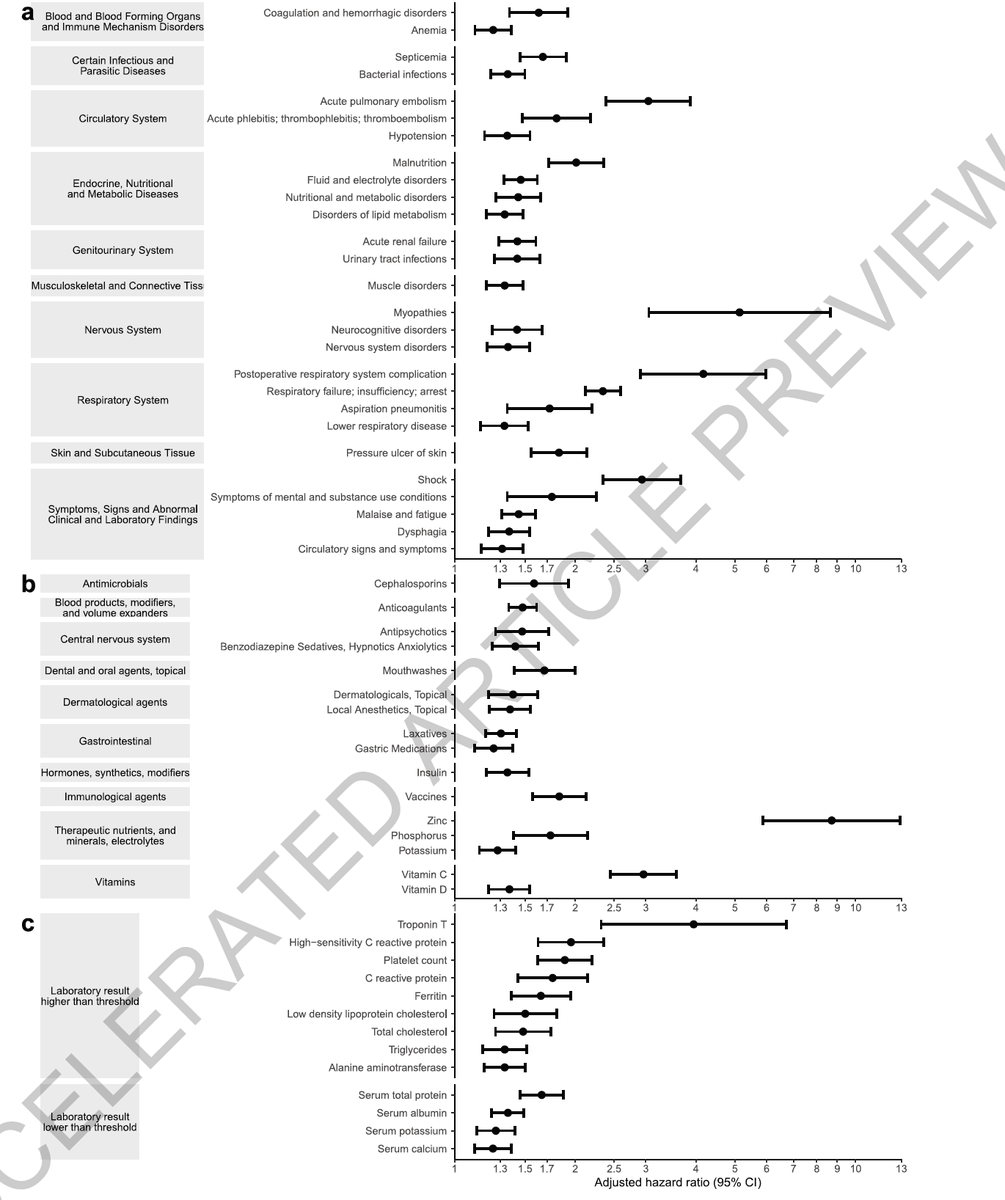
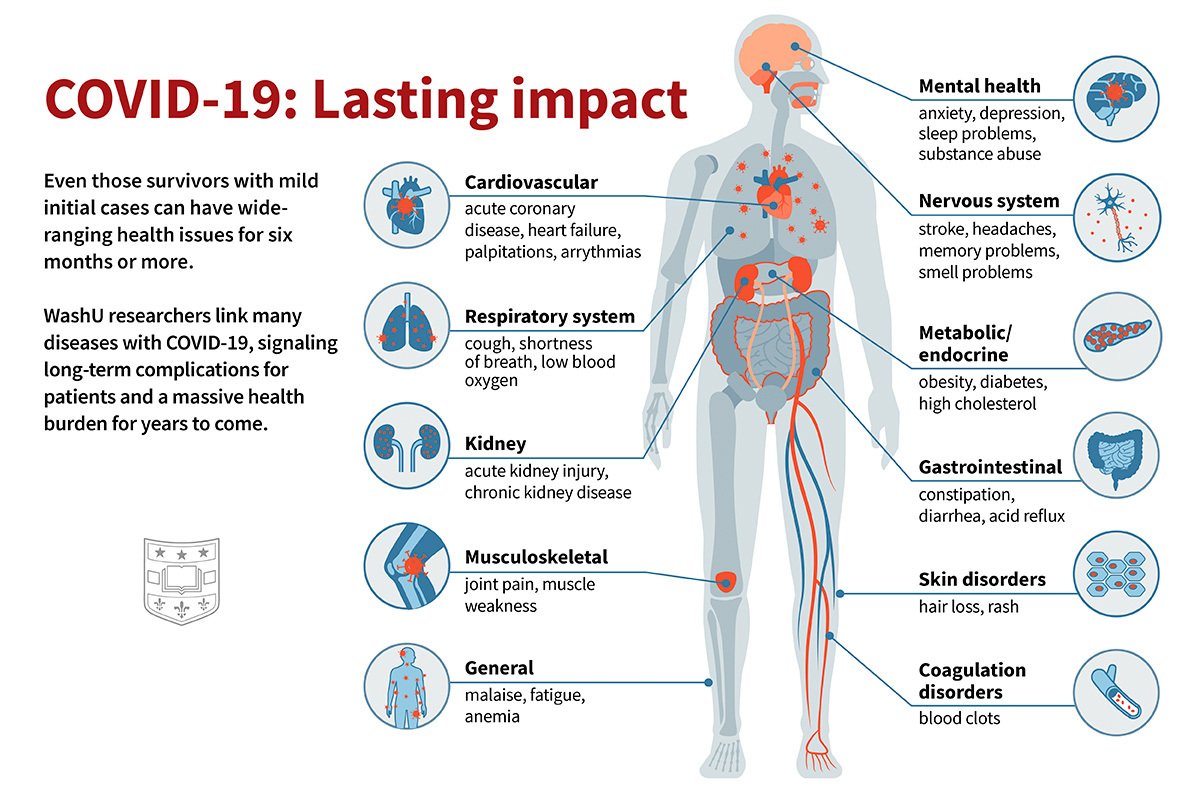
#Longcovid is a multifaceted disease; it can affect multiple organ systems including respiratory, cardiovascular, nervous, mental health, metabolic, gastrointestinal, kidneys, and other organ systems.
People with #longcovid have increased risk of incident use of several therapeutics including pain medications (opioids and non-opioids), antidepressants, anxiolytics, antihypertensives, and oral antihyperglycemics and evidence of laboratory abnormalities in multiple organ systems
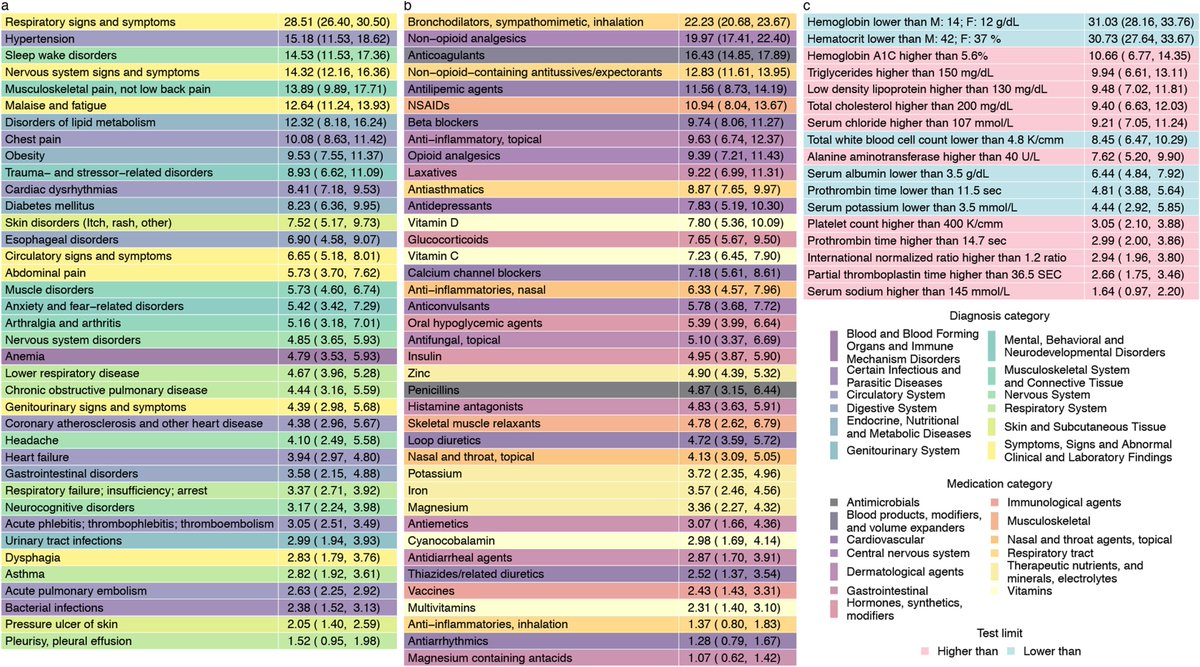
#Longcovid is evident even in those who had mild acute disease which did not require hospitalization during the acute phase of the infection
Burden of #longCOVID increases substantially in those who required hospitalization, and is most pronounced in those who needed ICU care during the acute phase of the infection
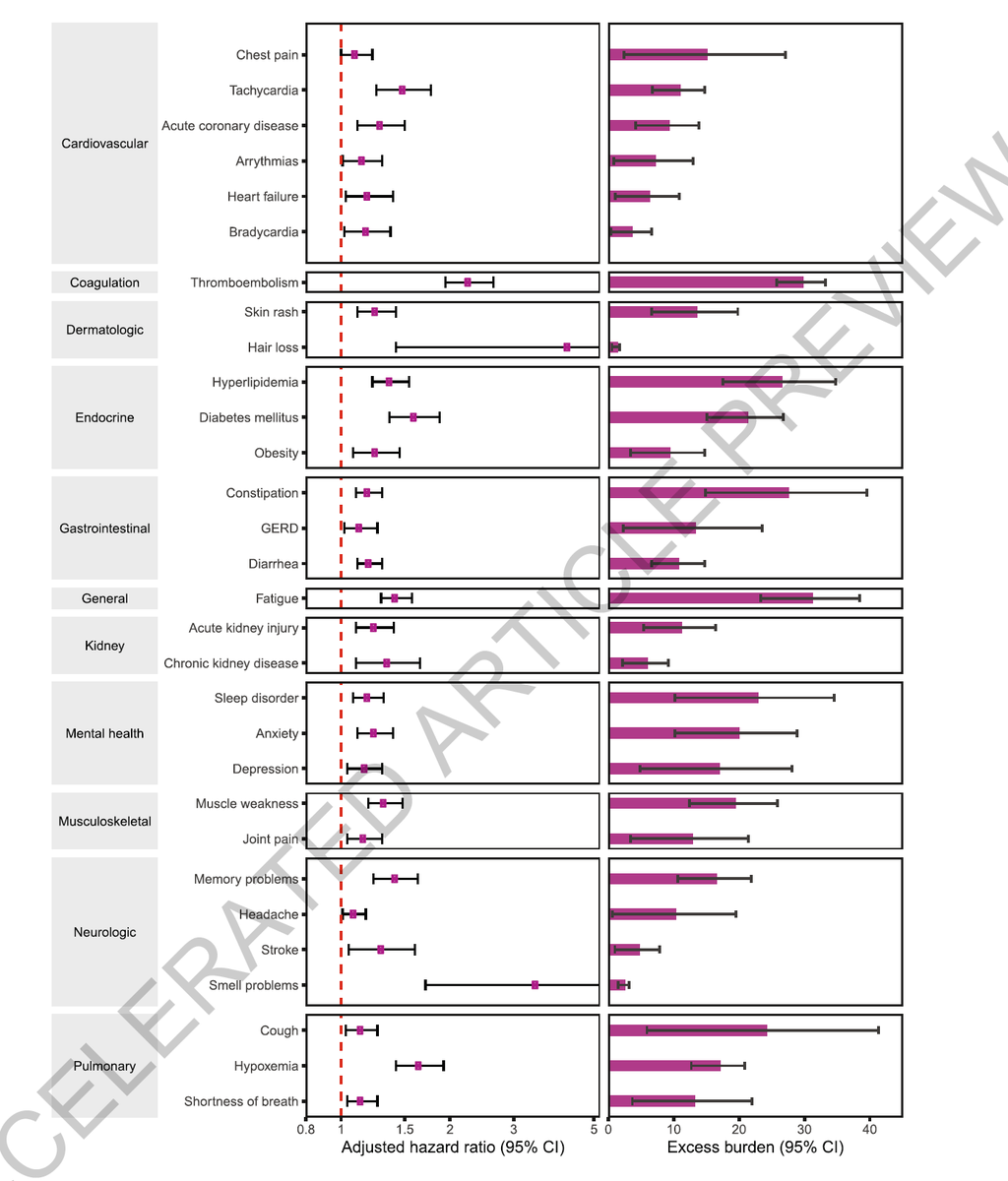
When comparing the post-acute sequelea of COVID vs flu, COVID exhibited remarkably higher burden of post-acute sequalae. Both the magnitude of risk AND extent of organ system involvement were much higher than post-acute flu manifestations.
People with #longcovid need multidisciplinary care.
If there ever was an exemplar in clinical medicine that best illustrates the importance of integrated multidisciplinary care, it is #longcovid. Health systems should quickly adapt to this reality.
If there ever was an exemplar in clinical medicine that best illustrates the importance of integrated multidisciplinary care, it is #longcovid. Health systems should quickly adapt to this reality.
I can’t believe that I have to say this, but yes, #longcovid is real. People with long covid should be listened to, and their experiences must be honored.
We got caught unprepared for Covid. Let’s not drop the ball on long Covid https://www.nytimes.com/2021/04/22/health/long-covid-risks.html">https://www.nytimes.com/2021/04/2...
Illustration by Sara Moser @WUSTL

 Read on Twitter
Read on Twitter