New NICE guidelines on postnatal care:
https://www.nice.org.uk/guidance/ng194/resources/postnatal-care-pdf-66142082148037
The">https://www.nice.org.uk/guidance/... committee responded to comments, including from us.
Our comments & the responses start on page 114:
https://www.nice.org.uk/guidance/ng194/documents/consultation-comments-and-responses
Here’s">https://www.nice.org.uk/guidance/... why we say some guidelines are #NotNICENotEvidenceBased
https://www.nice.org.uk/guidance/ng194/resources/postnatal-care-pdf-66142082148037
The">https://www.nice.org.uk/guidance/... committee responded to comments, including from us.
Our comments & the responses start on page 114:
https://www.nice.org.uk/guidance/ng194/documents/consultation-comments-and-responses
Here’s">https://www.nice.org.uk/guidance/... why we say some guidelines are #NotNICENotEvidenceBased
We highlighted grave concerns as parents whose babies experienced complications, including excessive weight loss, faltering growth, jaundice & hypertremic dehydration where exclusive breastfeeding was a significant contributing factor
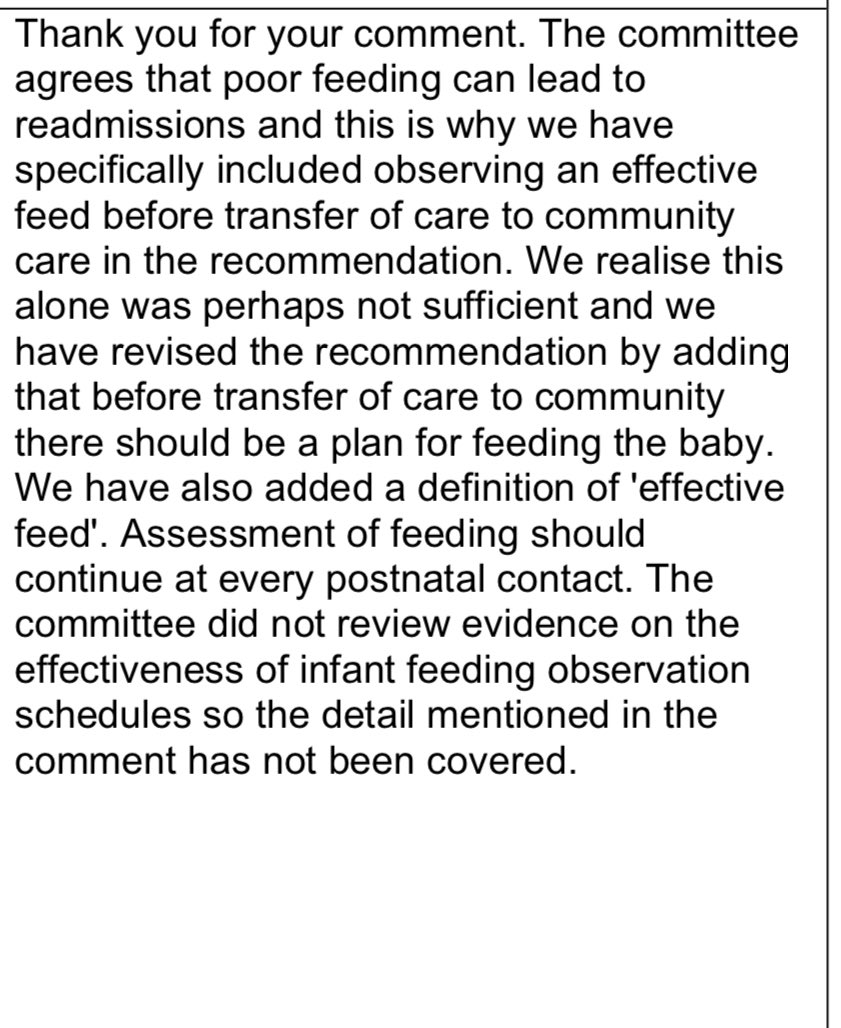
Hospital readmissions for feeding related complications are COMMON. We know of only one strategy demonstrated in RCTs to prevent them: limited supplementation of BFing with formula
Did the committee deem this important enough to even review?
No
#NotNICEnotevidencebased
Did the committee deem this important enough to even review?
No
#NotNICEnotevidencebased
We were pleased to see the committee acknowledge that combination feeding is possible, but they continue to refuse to offer this as a possible solution to feeding-related problems, or present it as an option to parents who are concerned about their baby’s breastmilk intake. Why?
No guidance on how to supplement & sustain breastfeeding.
Perhaps our friends at @FedIsBest could help? https://fedisbest.org/resources-for-parents/fed-best-guide-supplementing-breastfed-newborns/">https://fedisbest.org/resources...
Why so confident supplementation hinders BFing? Trials suggest limited early supplementation does not hinder BFing
#NotNICEnotevidencebased
Perhaps our friends at @FedIsBest could help? https://fedisbest.org/resources-for-parents/fed-best-guide-supplementing-breastfed-newborns/">https://fedisbest.org/resources...
Why so confident supplementation hinders BFing? Trials suggest limited early supplementation does not hinder BFing
#NotNICEnotevidencebased
Observational data has found up to 4oz formula a day in addition to breastmilk is not associated with stopping BFing earlier
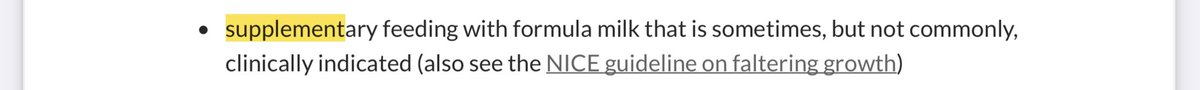
Also, why so confident supplementary feeding is not commonly clinically indicated when they didn’t review the evidence on this?
#NotNICEnotevidencebased
Also, why so confident supplementary feeding is not commonly clinically indicated when they didn’t review the evidence on this?
#NotNICEnotevidencebased
They endorse the Baby Friendly Initiative’s feeding observation schedules but don’t review evidence as to whether or not they adequately detect feeding difficulties, especially insufficient milk intake.
We had a look & what did we find: no evidence https://abs.twimg.com/emoji/v2/... draggable="false" alt="😱" title="Vor Angst schreiendes Gesicht" aria-label="Emoji: Vor Angst schreiendes Gesicht">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="😱" title="Vor Angst schreiendes Gesicht" aria-label="Emoji: Vor Angst schreiendes Gesicht">
#NotNICEnotevidencebased
We had a look & what did we find: no evidence
#NotNICEnotevidencebased
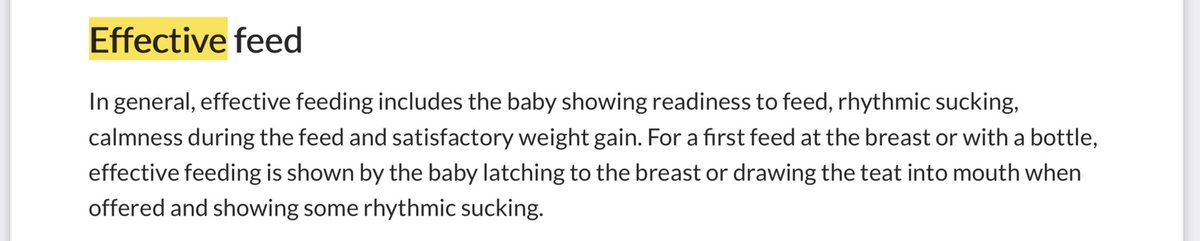
The definition of effective feed includes no mention of how to ensure actual milk intake or identify early signs of insufficient intake.
Not reassuring to us. We were told our babies were feeding well only to be readmitted to hospital as a result of underfeeding hours later
Not reassuring to us. We were told our babies were feeding well only to be readmitted to hospital as a result of underfeeding hours later
In any other context would it be acceptable to say food is indicated ONLY when a person is showing signs of serious undernutrition?
If a baby shows signs of hunger (e.g unsatisfied, overly frequent feeding, excessive sleepiness) then surely responsive feeding is to feed them?
If a baby shows signs of hunger (e.g unsatisfied, overly frequent feeding, excessive sleepiness) then surely responsive feeding is to feed them?
And of course there are other reasons families might want to mix feed: sharing responsibilities, taking the pressure off, giving all parents the chance to get adequate sleep at night, to give the lactating parent time to attend to other things ... Our families, our decision!
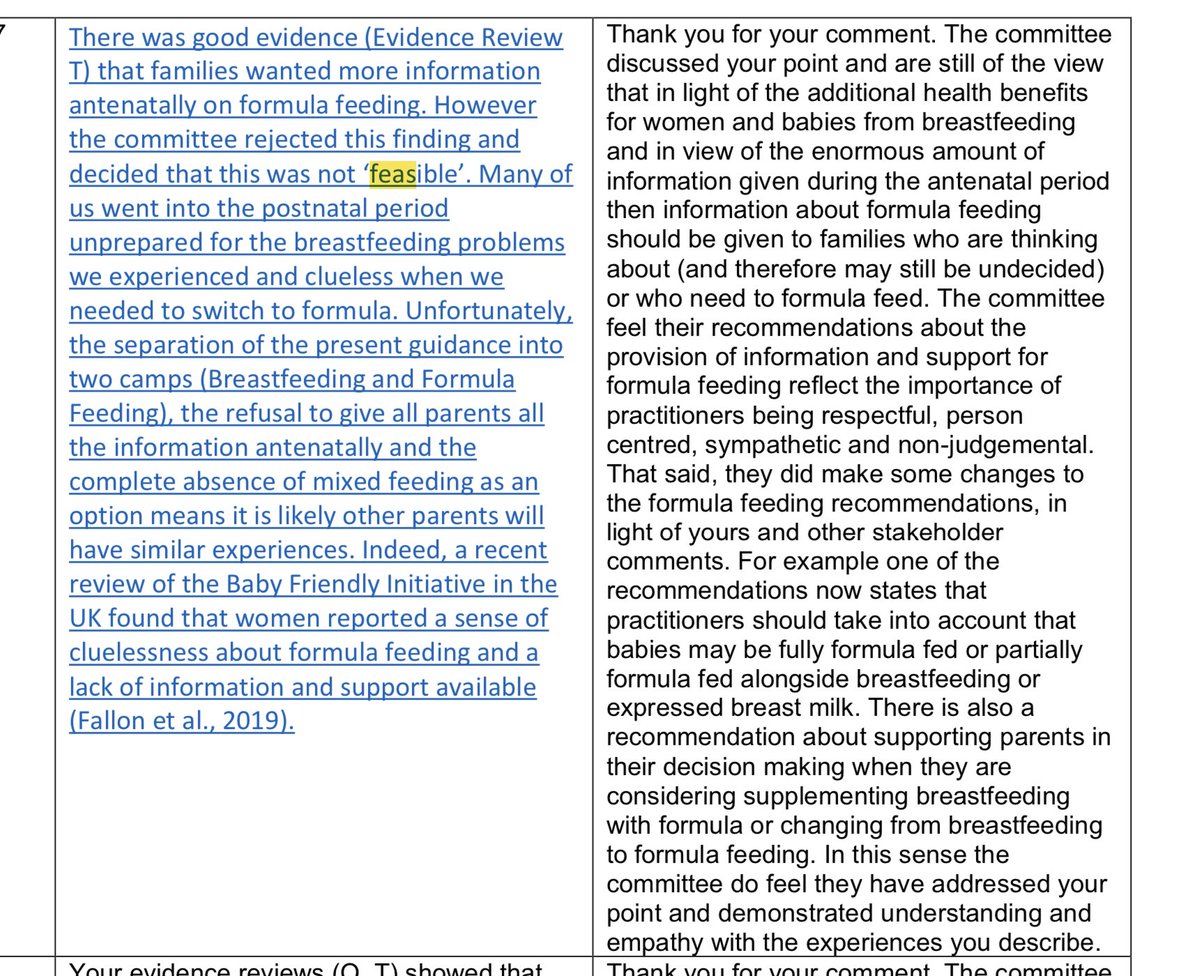
Their own review found that parents wanted information about all feeding methods regardless of their feeding intention. They conclude this is not feasible ...
#NotNICEnotevidencebased
#NotNICEnotevidencebased
They only recommend discussing formula with those considering using it.
Newsflash: the majority of parents who intend to exclusively breastfeed will use formula at some point. Get over it and make sure we are prepared to do so confidently & safely
#NotNICEnotevidencebased
Newsflash: the majority of parents who intend to exclusively breastfeed will use formula at some point. Get over it and make sure we are prepared to do so confidently & safely
#NotNICEnotevidencebased
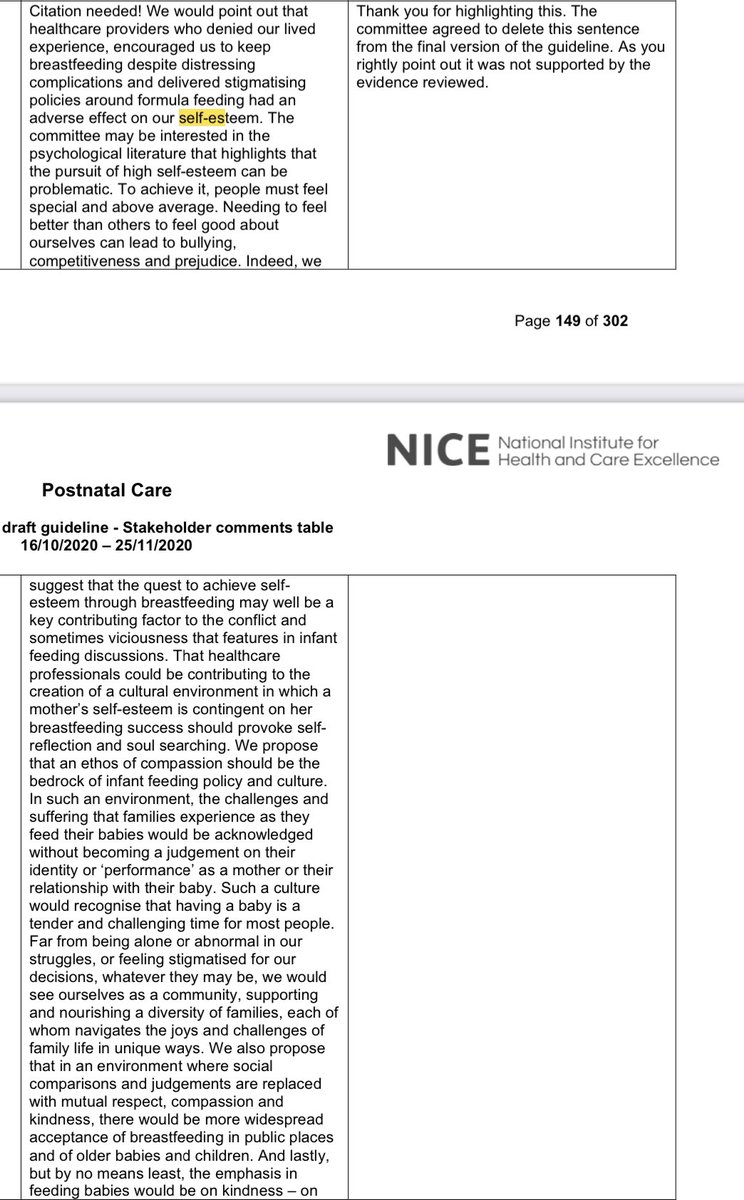
We were relieved to see that an original suggestion (we kid you not. This was actually proposed) that breastfeeding success could help improve women’s self-esteem was removed without any attempt to defend themselves.
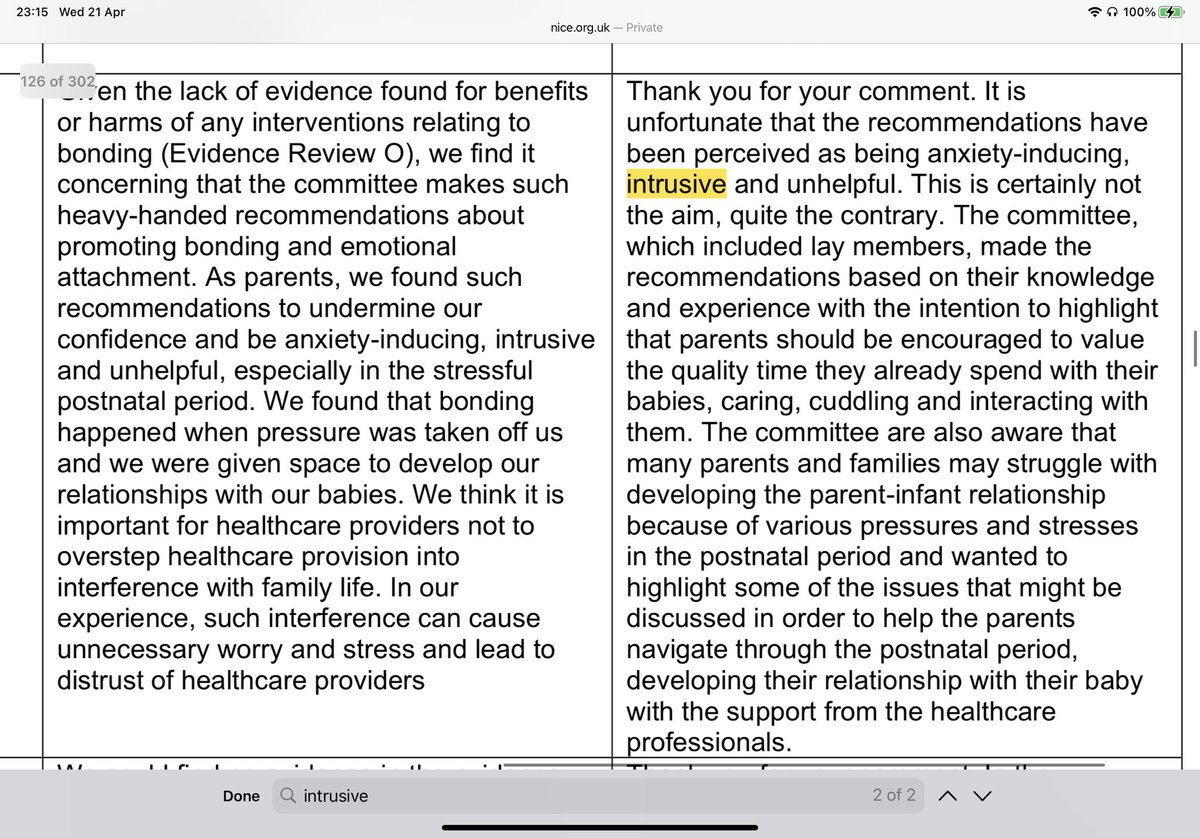
But they don’t constrain themselves to evidence when it comes to bonding. They are very keen on skin-to-skin to promote bonding esp for babies who are being formula fed.
Evidence in their review that skin-to-skin improves bonding, attachment or parent-child relationships: None!
Evidence in their review that skin-to-skin improves bonding, attachment or parent-child relationships: None!
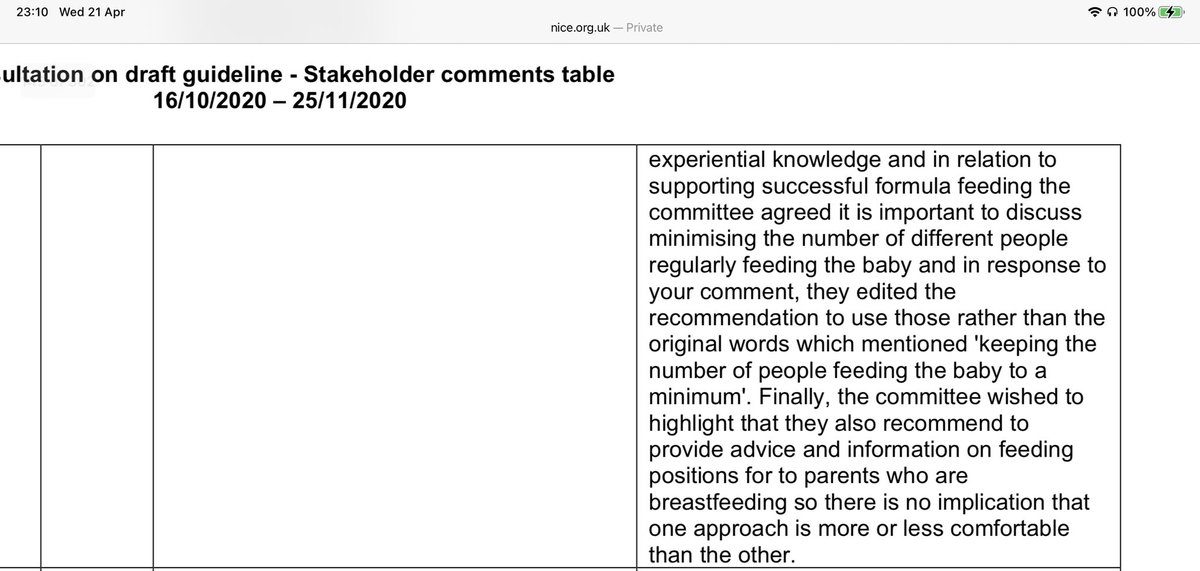
They’re also insistent that the number of people feeding a baby should be “kept to a minimum”. Evidence in their review that this improves any outcome: Also none!
#NotNICEnotevidencebased
#NotNICEnotevidencebased
This isn’t about improving health outcomes, ensuring babies are safely fed or that parents’ physical & psychological needs are attended to. This is healthcare providers telling us how to conduct our family life. They are confused about why this comes across as intrusive  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤷🏻♀️" title="Achselzuckende Frau (heller Hautton)" aria-label="Emoji: Achselzuckende Frau (heller Hautton)">.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤷🏻♀️" title="Achselzuckende Frau (heller Hautton)" aria-label="Emoji: Achselzuckende Frau (heller Hautton)">.
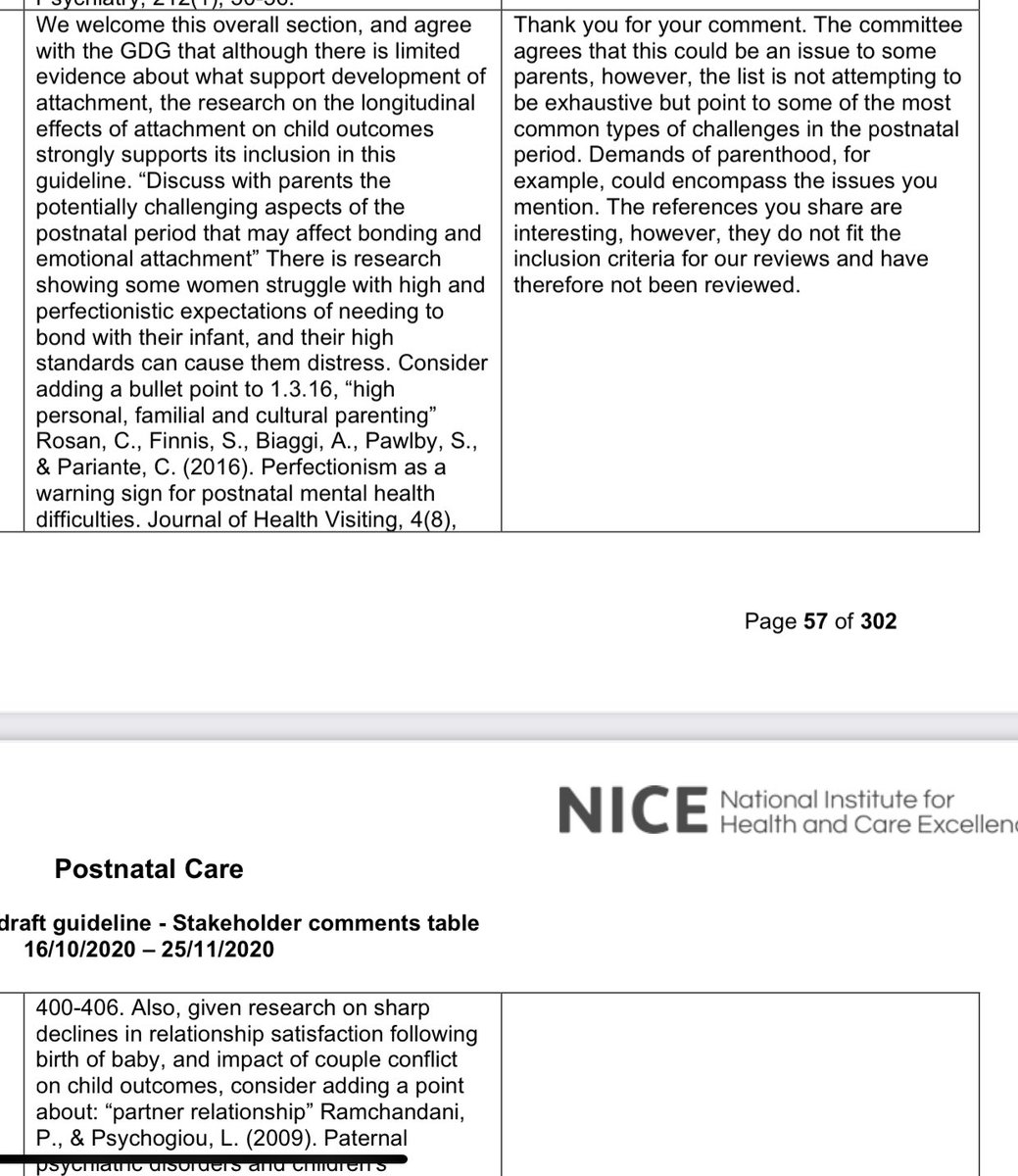
We were very interested to read @BABCP ‘s comment on perfectionistic expectations about bonding...
Can anyone else see how advice to exclusively BF, have lots of skin to skin, be constantly responsive to baby’s cues & limit the number of ppl who feed baby might contribute here?
Can anyone else see how advice to exclusively BF, have lots of skin to skin, be constantly responsive to baby’s cues & limit the number of ppl who feed baby might contribute here?
The committee don’t really address that, but given they are so keen to navigate the early postnatal period and their new relationship with their baby, why didn’t they review any research on developing attachment security?
If they had, they would have realised that a key concept in attachment science is the idea of ‘good enough parenting’. Parents whose children are securely attached to them are attuned & responsive about 20-30% of the time - old paper but classic: https://www.semanticscholar.org/paper/Interactive-mismatch-and-repair%3A-Challenges-to-the-Tronick-Gianino/34229e4887aa146bf4a7e9467a5c6d9136fb6d52">https://www.semanticscholar.org/paper/Int...
They might have discovered that experts in attachment, like the cognitive behavioural therapists at the @BABCP, emphasise that perfection is neither achievable nor desirable. Knowing that, is there a need for prescriptive suggestions or advice here?
#NotNICEnotevidencebased
#NotNICEnotevidencebased
They justify making these recommendations on the basis of the committee’s expertise. Ok...
Here’s the committee list....
Where’s the attachment expertise? Any social workers or psychologists who conduct specialist assessments of parent-infant attachment or interventions for attachment difficulties? Maybe the perinatal psychiatrist?
https://www.nice.org.uk/guidance/ng194/documents/committee-member-list-2">https://www.nice.org.uk/guidance/...
Where’s the attachment expertise? Any social workers or psychologists who conduct specialist assessments of parent-infant attachment or interventions for attachment difficulties? Maybe the perinatal psychiatrist?
https://www.nice.org.uk/guidance/ng194/documents/committee-member-list-2">https://www.nice.org.uk/guidance/...
Perhaps the best advice would be to meet baby’s needs, keep them clean, fed, enjoy them and make your own self care a priority (because who amongst us is at our best, most responsive self in any of our relationships when we are neglecting our own needs) & RELAX
All in all the guidelines:
Don’t address clinical safety issues re ensuring adequate milk intake
Ignore evidence that parents want to discuss all options
Refuse to present all options to all parents
Dish out advice about how to conduct family life
#NotNICEnotevidencebased
Don’t address clinical safety issues re ensuring adequate milk intake
Ignore evidence that parents want to discuss all options
Refuse to present all options to all parents
Dish out advice about how to conduct family life
#NotNICEnotevidencebased

 Read on Twitter
Read on Twitter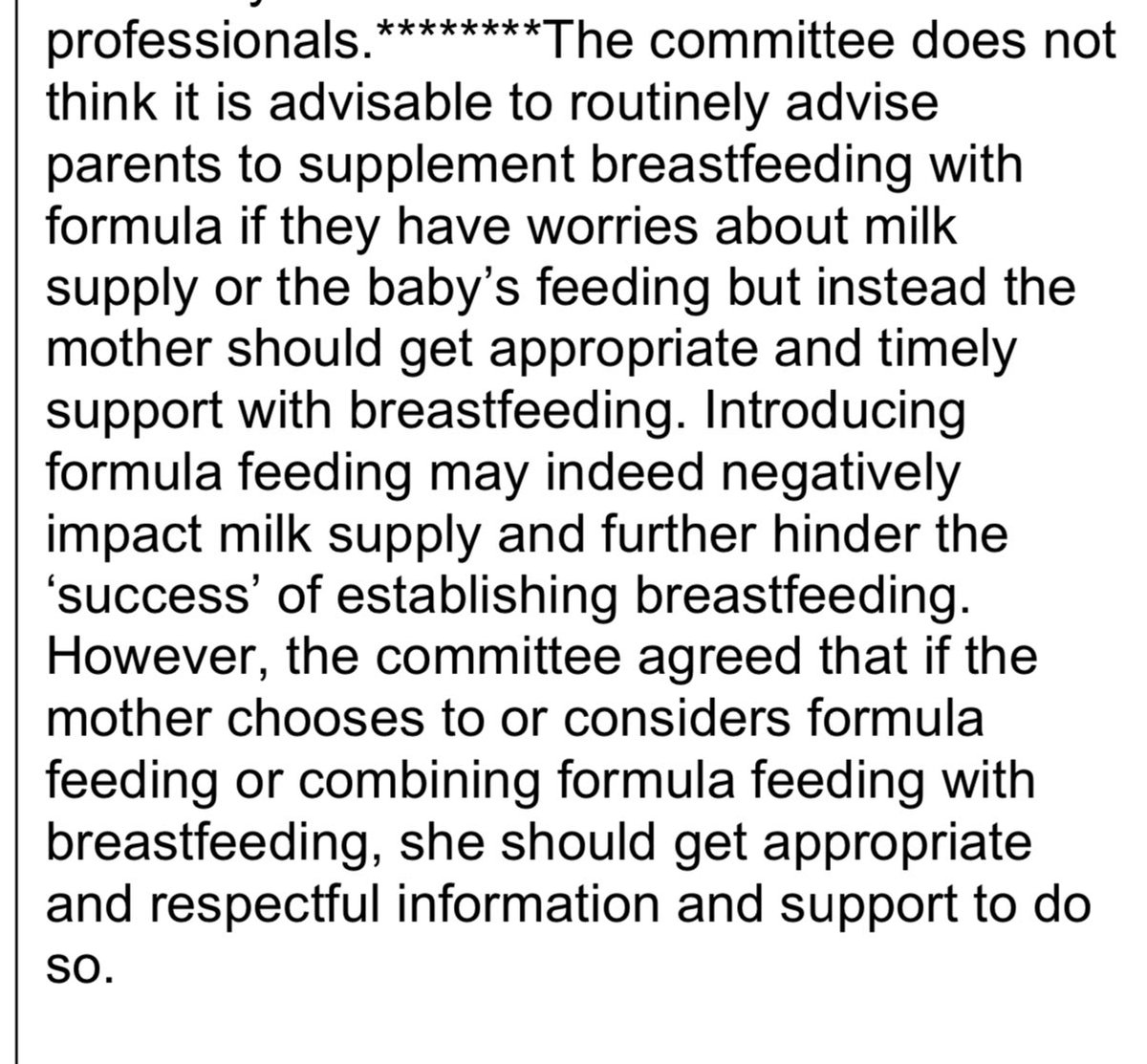
 #NotNICEnotevidencebased" title="They endorse the Baby Friendly Initiative’s feeding observation schedules but don’t review evidence as to whether or not they adequately detect feeding difficulties, especially insufficient milk intake.We had a look & what did we find: no evidence https://abs.twimg.com/emoji/v2/... draggable="false" alt="😱" title="Vor Angst schreiendes Gesicht" aria-label="Emoji: Vor Angst schreiendes Gesicht"> #NotNICEnotevidencebased" class="img-responsive" style="max-width:100%;"/>
#NotNICEnotevidencebased" title="They endorse the Baby Friendly Initiative’s feeding observation schedules but don’t review evidence as to whether or not they adequately detect feeding difficulties, especially insufficient milk intake.We had a look & what did we find: no evidence https://abs.twimg.com/emoji/v2/... draggable="false" alt="😱" title="Vor Angst schreiendes Gesicht" aria-label="Emoji: Vor Angst schreiendes Gesicht"> #NotNICEnotevidencebased" class="img-responsive" style="max-width:100%;"/>
 ." title="This isn’t about improving health outcomes, ensuring babies are safely fed or that parents’ physical & psychological needs are attended to. This is healthcare providers telling us how to conduct our family life. They are confused about why this comes across as intrusive https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤷🏻♀️" title="Achselzuckende Frau (heller Hautton)" aria-label="Emoji: Achselzuckende Frau (heller Hautton)">." class="img-responsive" style="max-width:100%;"/>
." title="This isn’t about improving health outcomes, ensuring babies are safely fed or that parents’ physical & psychological needs are attended to. This is healthcare providers telling us how to conduct our family life. They are confused about why this comes across as intrusive https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤷🏻♀️" title="Achselzuckende Frau (heller Hautton)" aria-label="Emoji: Achselzuckende Frau (heller Hautton)">." class="img-responsive" style="max-width:100%;"/>