Let& #39;s talk about infant LP stylet practices for insertion & removal. As an intern, I memorized these techniques, but didn& #39;t understand why.
I hope this #tweetorial helps explain the WHY and improves your procedural acumen! #PEM #PEMTwitter
1/
Img: NEJM
I hope this #tweetorial helps explain the WHY and improves your procedural acumen! #PEM #PEMTwitter
1/
Img: NEJM
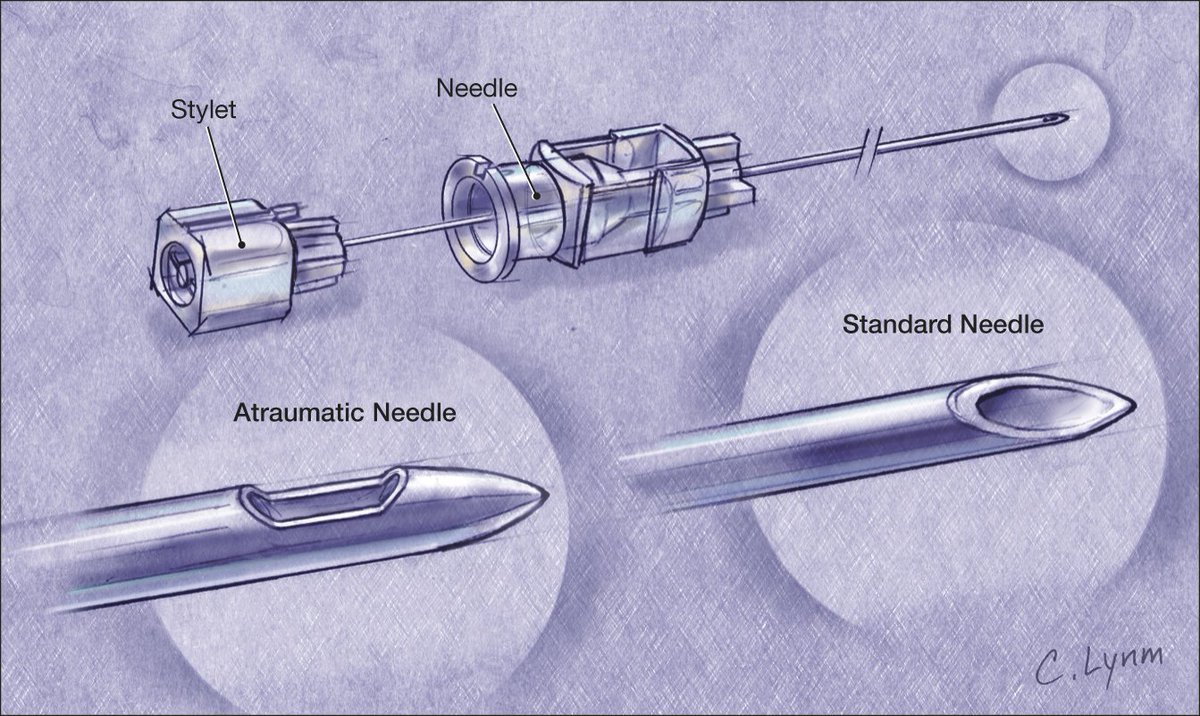
It& #39;s important to understand the anatomy of an LP needle/stylet. An LP needle is hollow with an inner stylet. Why the stylet? Why not just use a hollow needle to access the subarachnoid space?
2/
Img: JAMA
2/
Img: JAMA
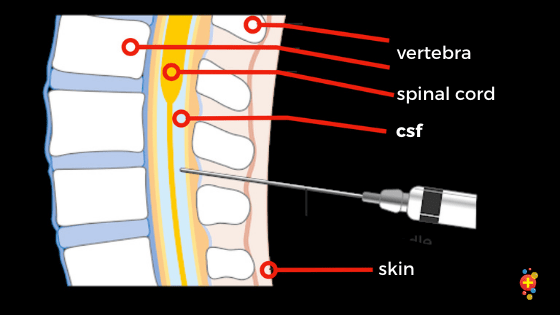
Standard LP needles are "cutting" (dissect soft tissue). A hollow needle without a stylet traps skin cells & pushes them into the subarachnoid space, causing a clogged needle, or in the long term, an epidermoid tumor. Adding a stylet prevents this.
3/
Img: @DFTBubbles
3/
Img: @DFTBubbles
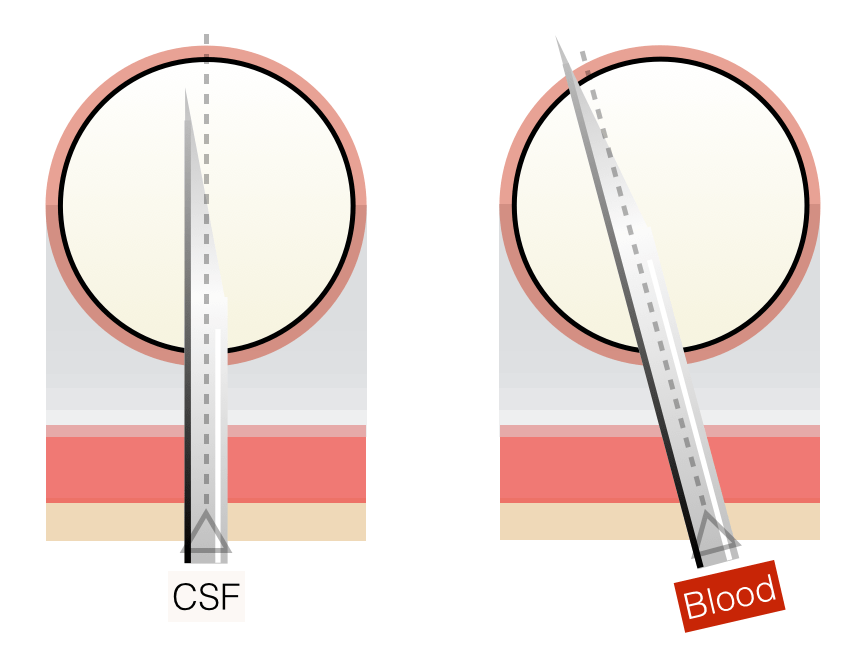
BUT, with a stylet, you can& #39;t see CSF return. In infants, it& #39;s easy to backwall into the surrounding venous plexus ("traumatic tap"). In early stylet removal (insert needle/stylet through dermis only, then remove stylet), you see CSF as soon as you& #39;re in.
4/
Img: @PEMTweets
4/
Img: @PEMTweets
So you& #39;re in the space ( https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍾" title="Flasche mit knallendem Korken" aria-label="Emoji: Flasche mit knallendem Korken">) and have collected your CSF. It& #39;s important to replace the stylet before you remove the needle. Why?
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍾" title="Flasche mit knallendem Korken" aria-label="Emoji: Flasche mit knallendem Korken">) and have collected your CSF. It& #39;s important to replace the stylet before you remove the needle. Why?
5/
Img: EM News
5/
Img: EM News
The short term reason to replace the stylet is that it decreases post-LP headache (in babies: fussiness). It& #39;s theorized that nerves are sucked into the needle then drawn through the dura as you remove the needle, resulting in prolonged CSF leakage.
6/
Img: Google
6/
Img: Google
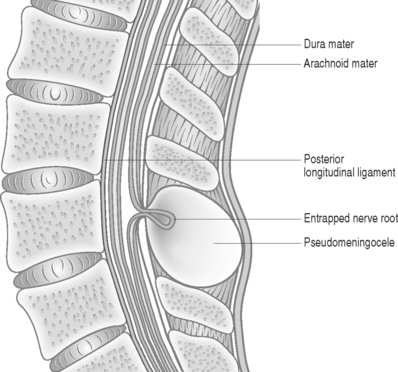
The long term reason is that dragging nerve fibers to outside the subarachnoid space can result in entrapped lumbar/sacral nerves and pseudomeningocele.
7/
Img: MSK Key
7/
Img: MSK Key
In summary:
*Using stylets to go through skin prevents epidermoid tumors & clogged needles
*Early stylet removal once through the skin minimizes "traumatic taps"
*Stylet replacement before needle removal decreases post LP headache & nerve entrapment
8/
*Using stylets to go through skin prevents epidermoid tumors & clogged needles
*Early stylet removal once through the skin minimizes "traumatic taps"
*Stylet replacement before needle removal decreases post LP headache & nerve entrapment
8/
#FOAMed summaries w/references:
https://pemcincinnati.com/blog/why-we-do-what-we-do-early-stylet-removal-for-lumbar-puncture-in-infants/
https://pemcincinnati.com/blog/why-... href=" https://rebelem.com/post-lumbar-puncture-headaches/
https://rebelem.com/post-lumb... href=" https://pedemmorsels.com/spinal-needle-stylet/
9/end">https://pedemmorsels.com/spinal-ne...
https://pemcincinnati.com/blog/why-we-do-what-we-do-early-stylet-removal-for-lumbar-puncture-in-infants/
9/end">https://pedemmorsels.com/spinal-ne...

 Read on Twitter
Read on Twitter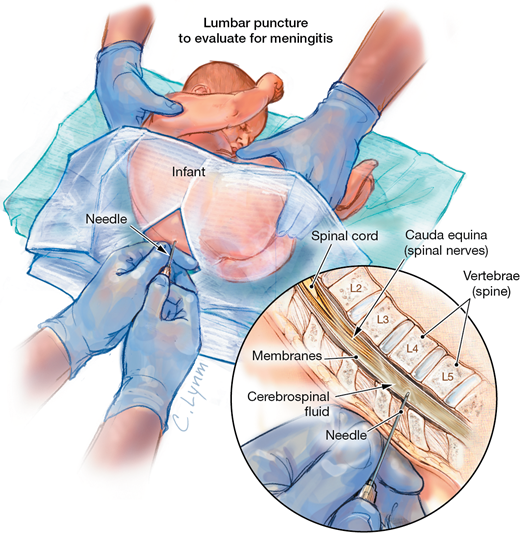
 ) and have collected your CSF. It& #39;s important to replace the stylet before you remove the needle. Why?5/Img: EM News" title="So you& #39;re in the space (https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍾" title="Flasche mit knallendem Korken" aria-label="Emoji: Flasche mit knallendem Korken">) and have collected your CSF. It& #39;s important to replace the stylet before you remove the needle. Why?5/Img: EM News" class="img-responsive" style="max-width:100%;"/>
) and have collected your CSF. It& #39;s important to replace the stylet before you remove the needle. Why?5/Img: EM News" title="So you& #39;re in the space (https://abs.twimg.com/emoji/v2/... draggable="false" alt="🍾" title="Flasche mit knallendem Korken" aria-label="Emoji: Flasche mit knallendem Korken">) and have collected your CSF. It& #39;s important to replace the stylet before you remove the needle. Why?5/Img: EM News" class="img-responsive" style="max-width:100%;"/>