1/  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧵" title="Thread" aria-label="Emoji: Thread">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧵" title="Thread" aria-label="Emoji: Thread">
Why can propofol infusion at high doses cause Propofol-related Infusion Syndrome (PRIS)?
To understand why we have to revisit the old adage of supply and demand.
#Tweetorial #MedTwitter
Why can propofol infusion at high doses cause Propofol-related Infusion Syndrome (PRIS)?
To understand why we have to revisit the old adage of supply and demand.
#Tweetorial #MedTwitter
2/
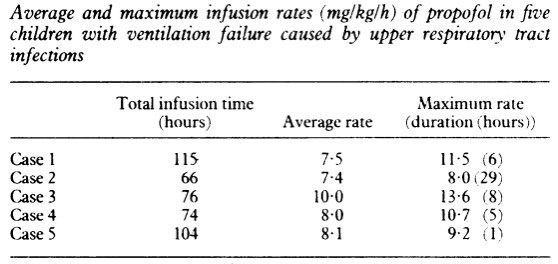
Propofol is a sedative-hypnotic developed in the 1970s.
PRIS was first described in the late 1980s when several children had cardiovascular collapse and severe bradyarrythmias while on propofol.
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔑" title="Schlüssel" aria-label="Emoji: Schlüssel">They all had received extended, high-dose infusions.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔑" title="Schlüssel" aria-label="Emoji: Schlüssel">They all had received extended, high-dose infusions.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1883365/">https://www.ncbi.nlm.nih.gov/pmc/artic...
Propofol is a sedative-hypnotic developed in the 1970s.
PRIS was first described in the late 1980s when several children had cardiovascular collapse and severe bradyarrythmias while on propofol.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1883365/">https://www.ncbi.nlm.nih.gov/pmc/artic...
3/
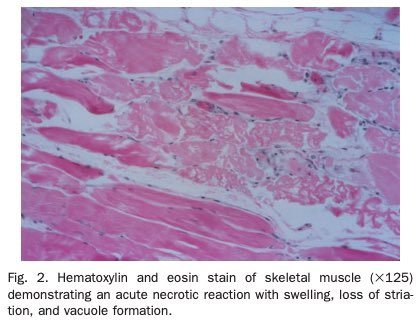
Subsequent case descriptions found that patients who developed PRIS also had:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Severe rhabdomyolysis and diffuse skeletal and cardiac muscular necrosis
https://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Severe rhabdomyolysis and diffuse skeletal and cardiac muscular necrosis
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Hypertriglyceridemia
https://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Hypertriglyceridemia
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Lactic acidosis
https://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Lactic acidosis
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Multiorgan failure
https://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Multiorgan failure
Kids seem to be more susceptible.
https://pubmed.ncbi.nlm.nih.gov/10759487/ ">https://pubmed.ncbi.nlm.nih.gov/10759487/...
Subsequent case descriptions found that patients who developed PRIS also had:
Kids seem to be more susceptible.
https://pubmed.ncbi.nlm.nih.gov/10759487/ ">https://pubmed.ncbi.nlm.nih.gov/10759487/...
4/
The pathogenesis of PRIS appears to be:
Skeletal/cardiac muscular necrosis https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> rhabdomyolysis, cardiac dysfunction, and metabolic sequelae.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> rhabdomyolysis, cardiac dysfunction, and metabolic sequelae.
So why can high dose, extended propofol infusions potentially cause necrosis of skeletal and cardiac muscle?
The pathogenesis of PRIS appears to be:
Skeletal/cardiac muscular necrosis
So why can high dose, extended propofol infusions potentially cause necrosis of skeletal and cardiac muscle?
5/
One clue emerged from a study in isolated rat mitochondria.
When the mitochondria were exposed to high doses of propofol their DNA production decreased dramatically.
https://pubmed.ncbi.nlm.nih.gov/2069600/ ">https://pubmed.ncbi.nlm.nih.gov/2069600/&...
One clue emerged from a study in isolated rat mitochondria.
When the mitochondria were exposed to high doses of propofol their DNA production decreased dramatically.
https://pubmed.ncbi.nlm.nih.gov/2069600/ ">https://pubmed.ncbi.nlm.nih.gov/2069600/&...
6/
Linking to PRIS pathophys (muscle necrosis), does propofol effect muscular mitochondrial function?
When guinea pig hearts were treated w/ propofol, O₂ consumption https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">.
This was evidenced by https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> myoglobin saturation and implied mitochondrial toxicity.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> myoglobin saturation and implied mitochondrial toxicity.
https://pubmed.ncbi.nlm.nih.gov/10667518/ ">https://pubmed.ncbi.nlm.nih.gov/10667518/...
Linking to PRIS pathophys (muscle necrosis), does propofol effect muscular mitochondrial function?
When guinea pig hearts were treated w/ propofol, O₂ consumption
This was evidenced by
https://pubmed.ncbi.nlm.nih.gov/10667518/ ">https://pubmed.ncbi.nlm.nih.gov/10667518/...
7/
This begs the question: how can propofol act as a mitochondrial toxin?
One potential mechanism is that propofol can block the function of the electron transport chain (via inhibition of co-enzyme Q). https://pubmed.ncbi.nlm.nih.gov/25296107/ ">https://pubmed.ncbi.nlm.nih.gov/25296107/...
This begs the question: how can propofol act as a mitochondrial toxin?
One potential mechanism is that propofol can block the function of the electron transport chain (via inhibition of co-enzyme Q). https://pubmed.ncbi.nlm.nih.gov/25296107/ ">https://pubmed.ncbi.nlm.nih.gov/25296107/...
8/
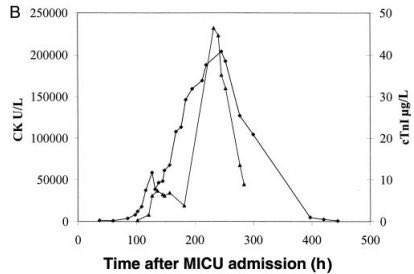
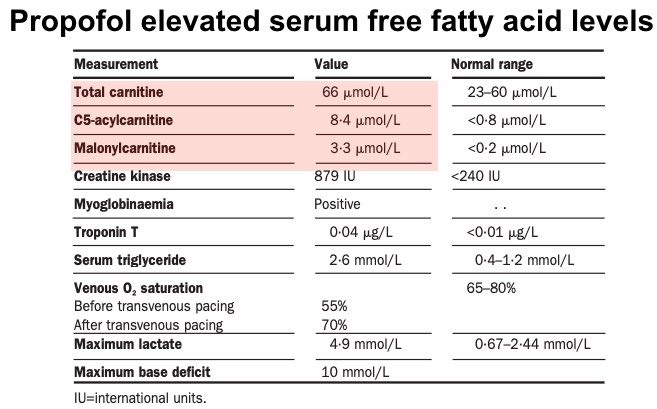
But electron transport chain inhibition may not be the whole story.
Patients with PRIS have been found to have elevated serum levels of free fatty acids (FFA), including C5-acylcarnitine (long chain) and malonylcarnitine (short chain).
https://pubmed.ncbi.nlm.nih.gov/11558490/ ">https://pubmed.ncbi.nlm.nih.gov/11558490/...
But electron transport chain inhibition may not be the whole story.
Patients with PRIS have been found to have elevated serum levels of free fatty acids (FFA), including C5-acylcarnitine (long chain) and malonylcarnitine (short chain).
https://pubmed.ncbi.nlm.nih.gov/11558490/ ">https://pubmed.ncbi.nlm.nih.gov/11558490/...
9/
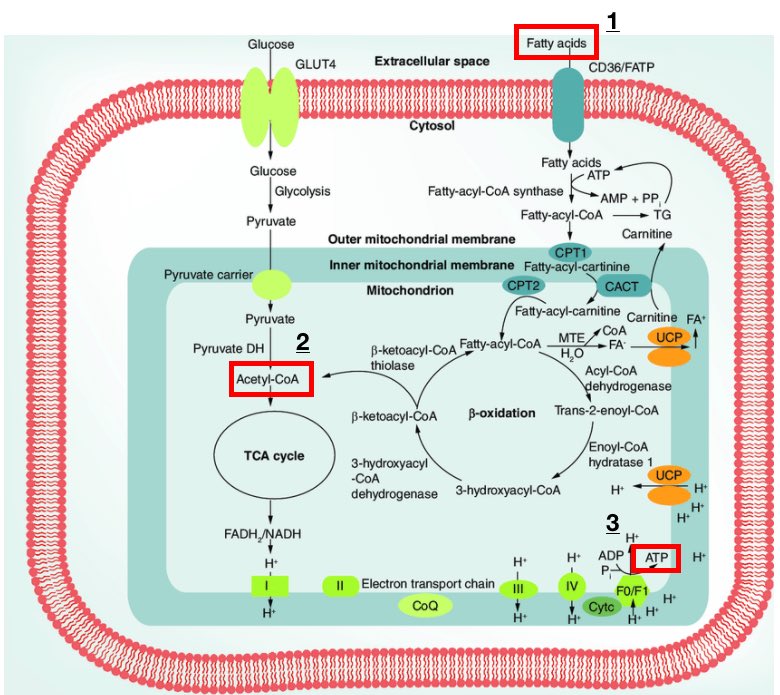
FFAs are an important source of ATP for tissues (including muscle), particularly during critical illness.
They mobilize from fat and are oxidized by mitochondria, generating ATP via the electron transport chain (steps 1-3 in the figure).
https://www.tandfonline.com/doi/abs/10.2217/clp.15.20">https://www.tandfonline.com/doi/abs/1...
FFAs are an important source of ATP for tissues (including muscle), particularly during critical illness.
They mobilize from fat and are oxidized by mitochondria, generating ATP via the electron transport chain (steps 1-3 in the figure).
https://www.tandfonline.com/doi/abs/10.2217/clp.15.20">https://www.tandfonline.com/doi/abs/1...
10/
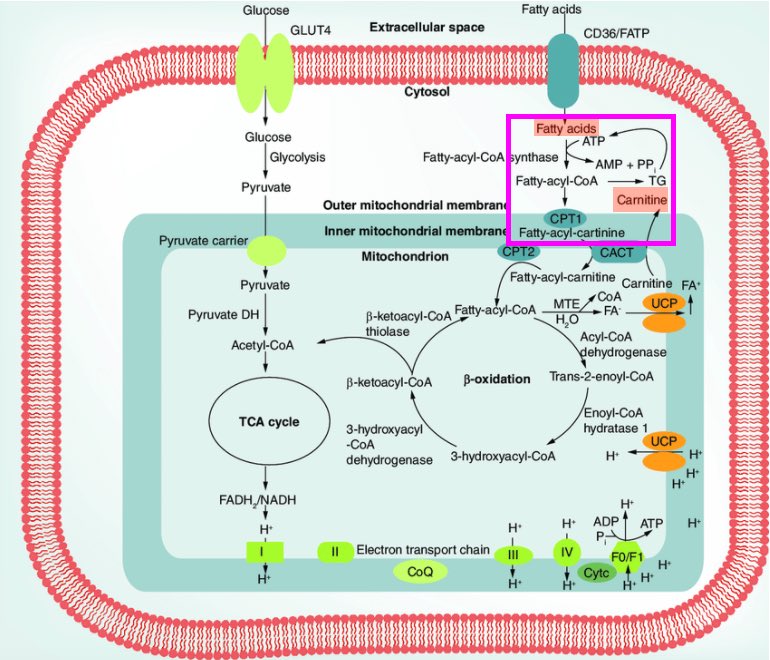
Long-chain FFAs require conjugation to carnitine in order to cross the mitochondrial membrane, undergo oxidation, and be utilized for ATP production (see boxes in figure).
Carnitine conjugation occurs via the enzyme carnitine palmityl transferase.
https://www.tandfonline.com/doi/abs/10.2217/clp.15.20">https://www.tandfonline.com/doi/abs/1...
Long-chain FFAs require conjugation to carnitine in order to cross the mitochondrial membrane, undergo oxidation, and be utilized for ATP production (see boxes in figure).
Carnitine conjugation occurs via the enzyme carnitine palmityl transferase.
https://www.tandfonline.com/doi/abs/10.2217/clp.15.20">https://www.tandfonline.com/doi/abs/1...
11/
Short-chain FFAs, on the other hand, can cross the mitochondrial membrane without conjugation.
Instead they go straight into oxidation and conversion to acetyl-CoA, prior to being used for ATP production (see step 2 in the figure).
https://pubmed.ncbi.nlm.nih.gov/12904852/ ">https://pubmed.ncbi.nlm.nih.gov/12904852/...
Short-chain FFAs, on the other hand, can cross the mitochondrial membrane without conjugation.
Instead they go straight into oxidation and conversion to acetyl-CoA, prior to being used for ATP production (see step 2 in the figure).
https://pubmed.ncbi.nlm.nih.gov/12904852/ ">https://pubmed.ncbi.nlm.nih.gov/12904852/...
12/
Recall from tweet #8 that PRIS associates w/ https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> short and long-chain FFAs in the serum.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> short and long-chain FFAs in the serum.
This suggests that propofol can inhibit both FFA conjugation and oxidation, blocking short and long chain FFA utilization for ATP production.
https://pubmed.ncbi.nlm.nih.gov/12904852/ ">https://pubmed.ncbi.nlm.nih.gov/12904852/...
Recall from tweet #8 that PRIS associates w/
This suggests that propofol can inhibit both FFA conjugation and oxidation, blocking short and long chain FFA utilization for ATP production.
https://pubmed.ncbi.nlm.nih.gov/12904852/ ">https://pubmed.ncbi.nlm.nih.gov/12904852/...
13/
The mechanism of PRIS seems to therefore be:
Extended, high-dose propofol infusion https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> blocked mitochondrial FFA utilization and electron transport chain function
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> blocked mitochondrial FFA utilization and electron transport chain function  https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> decreased ATP production
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> decreased ATP production  https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> muscular necrosis w/ sequela.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> muscular necrosis w/ sequela.
The mechanism of PRIS seems to therefore be:
Extended, high-dose propofol infusion
14/
At the same time, there are many other metabolic demands and stressors on muscle during critical illness.
PRIS reflects a mismatch between this demand and available energy supply, which culminates in muscle necrosis.
https://pubmed.ncbi.nlm.nih.gov/12904852/ ">https://pubmed.ncbi.nlm.nih.gov/12904852/...
At the same time, there are many other metabolic demands and stressors on muscle during critical illness.
PRIS reflects a mismatch between this demand and available energy supply, which culminates in muscle necrosis.
https://pubmed.ncbi.nlm.nih.gov/12904852/ ">https://pubmed.ncbi.nlm.nih.gov/12904852/...
15/
One final question, and then a caveat.
Children may be more susceptible to PRIS than adults. Why?
This may reflect https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> glycogen stores and higher dependence on FFAs for ATP production during critical illness, predisposing to muscular necrosis. https://pubmed.ncbi.nlm.nih.gov/19412155/ ">https://pubmed.ncbi.nlm.nih.gov/19412155/...
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> glycogen stores and higher dependence on FFAs for ATP production during critical illness, predisposing to muscular necrosis. https://pubmed.ncbi.nlm.nih.gov/19412155/ ">https://pubmed.ncbi.nlm.nih.gov/19412155/...
One final question, and then a caveat.
Children may be more susceptible to PRIS than adults. Why?
This may reflect
16/
Caveat:
I use propofol in my practice all of the time. I think it’s a terrific sedative.
PRIS is rare and preventable with serum creatine kinase (CK) level monitoring and avoidance of extended, high-dose propofol infusions.
Caveat:
I use propofol in my practice all of the time. I think it’s a terrific sedative.
PRIS is rare and preventable with serum creatine kinase (CK) level monitoring and avoidance of extended, high-dose propofol infusions.
17/
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💉" title="Spritze" aria-label="Emoji: Spritze">Propofol-related infusion syndrome (PRIS) is characterized by skeletal + cardiac muscular necrosis
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💉" title="Spritze" aria-label="Emoji: Spritze">Propofol-related infusion syndrome (PRIS) is characterized by skeletal + cardiac muscular necrosis
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💉" title="Spritze" aria-label="Emoji: Spritze">Blockade of free fatty acid utilization in mitochondria by propofol causes decreased ATP production
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💉" title="Spritze" aria-label="Emoji: Spritze">Blockade of free fatty acid utilization in mitochondria by propofol causes decreased ATP production
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="💉" title="Spritze" aria-label="Emoji: Spritze"> Mismatch between metabolic energy supply and demand leads to necrosis
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💉" title="Spritze" aria-label="Emoji: Spritze"> Mismatch between metabolic energy supply and demand leads to necrosis
Correction for tweet #5, which should read:
“When the mitochondria were exposed to high doses of propofol their ATP production decreased dramatically.”
“When the mitochondria were exposed to high doses of propofol their ATP production decreased dramatically.”

 Read on Twitter
Read on Twitter Why can propofol infusion at high doses cause Propofol-related Infusion Syndrome (PRIS)?To understand why we have to revisit the old adage of supply and demand. #Tweetorial #MedTwitter" title="1/ https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧵" title="Thread" aria-label="Emoji: Thread">Why can propofol infusion at high doses cause Propofol-related Infusion Syndrome (PRIS)?To understand why we have to revisit the old adage of supply and demand. #Tweetorial #MedTwitter" class="img-responsive" style="max-width:100%;"/>
Why can propofol infusion at high doses cause Propofol-related Infusion Syndrome (PRIS)?To understand why we have to revisit the old adage of supply and demand. #Tweetorial #MedTwitter" title="1/ https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧵" title="Thread" aria-label="Emoji: Thread">Why can propofol infusion at high doses cause Propofol-related Infusion Syndrome (PRIS)?To understand why we have to revisit the old adage of supply and demand. #Tweetorial #MedTwitter" class="img-responsive" style="max-width:100%;"/>
 They all had received extended, high-dose infusions. https://www.ncbi.nlm.nih.gov/pmc/artic..." title="2/Propofol is a sedative-hypnotic developed in the 1970s.PRIS was first described in the late 1980s when several children had cardiovascular collapse and severe bradyarrythmias while on propofol.https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔑" title="Schlüssel" aria-label="Emoji: Schlüssel">They all had received extended, high-dose infusions. https://www.ncbi.nlm.nih.gov/pmc/artic..." class="img-responsive" style="max-width:100%;"/>
They all had received extended, high-dose infusions. https://www.ncbi.nlm.nih.gov/pmc/artic..." title="2/Propofol is a sedative-hypnotic developed in the 1970s.PRIS was first described in the late 1980s when several children had cardiovascular collapse and severe bradyarrythmias while on propofol.https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔑" title="Schlüssel" aria-label="Emoji: Schlüssel">They all had received extended, high-dose infusions. https://www.ncbi.nlm.nih.gov/pmc/artic..." class="img-responsive" style="max-width:100%;"/>
 Severe rhabdomyolysis and diffuse skeletal and cardiac muscular necrosishttps://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Hypertriglyceridemiahttps://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Lactic acidosis https://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Multiorgan failureKids seem to be more susceptible. https://pubmed.ncbi.nlm.nih.gov/10759487/..." title="3/Subsequent case descriptions found that patients who developed PRIS also had:https://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Severe rhabdomyolysis and diffuse skeletal and cardiac muscular necrosishttps://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Hypertriglyceridemiahttps://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Lactic acidosis https://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Multiorgan failureKids seem to be more susceptible. https://pubmed.ncbi.nlm.nih.gov/10759487/...">
Severe rhabdomyolysis and diffuse skeletal and cardiac muscular necrosishttps://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Hypertriglyceridemiahttps://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Lactic acidosis https://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Multiorgan failureKids seem to be more susceptible. https://pubmed.ncbi.nlm.nih.gov/10759487/..." title="3/Subsequent case descriptions found that patients who developed PRIS also had:https://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Severe rhabdomyolysis and diffuse skeletal and cardiac muscular necrosishttps://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Hypertriglyceridemiahttps://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Lactic acidosis https://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Multiorgan failureKids seem to be more susceptible. https://pubmed.ncbi.nlm.nih.gov/10759487/...">
 Severe rhabdomyolysis and diffuse skeletal and cardiac muscular necrosishttps://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Hypertriglyceridemiahttps://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Lactic acidosis https://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Multiorgan failureKids seem to be more susceptible. https://pubmed.ncbi.nlm.nih.gov/10759487/..." title="3/Subsequent case descriptions found that patients who developed PRIS also had:https://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Severe rhabdomyolysis and diffuse skeletal and cardiac muscular necrosishttps://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Hypertriglyceridemiahttps://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Lactic acidosis https://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Multiorgan failureKids seem to be more susceptible. https://pubmed.ncbi.nlm.nih.gov/10759487/...">
Severe rhabdomyolysis and diffuse skeletal and cardiac muscular necrosishttps://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Hypertriglyceridemiahttps://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Lactic acidosis https://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Multiorgan failureKids seem to be more susceptible. https://pubmed.ncbi.nlm.nih.gov/10759487/..." title="3/Subsequent case descriptions found that patients who developed PRIS also had:https://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Severe rhabdomyolysis and diffuse skeletal and cardiac muscular necrosishttps://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Hypertriglyceridemiahttps://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Lactic acidosis https://abs.twimg.com/emoji/v2/... draggable="false" alt="❤️" title="Rotes Herz" aria-label="Emoji: Rotes Herz">Multiorgan failureKids seem to be more susceptible. https://pubmed.ncbi.nlm.nih.gov/10759487/...">

 .This was evidenced by https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> myoglobin saturation and implied mitochondrial toxicity. https://pubmed.ncbi.nlm.nih.gov/10667518/..." title="6/Linking to PRIS pathophys (muscle necrosis), does propofol effect muscular mitochondrial function?When guinea pig hearts were treated w/ propofol, O₂ consumption https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">.This was evidenced by https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> myoglobin saturation and implied mitochondrial toxicity. https://pubmed.ncbi.nlm.nih.gov/10667518/..." class="img-responsive" style="max-width:100%;"/>
.This was evidenced by https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> myoglobin saturation and implied mitochondrial toxicity. https://pubmed.ncbi.nlm.nih.gov/10667518/..." title="6/Linking to PRIS pathophys (muscle necrosis), does propofol effect muscular mitochondrial function?When guinea pig hearts were treated w/ propofol, O₂ consumption https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">.This was evidenced by https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> myoglobin saturation and implied mitochondrial toxicity. https://pubmed.ncbi.nlm.nih.gov/10667518/..." class="img-responsive" style="max-width:100%;"/>

 short and long-chain FFAs in the serum. This suggests that propofol can inhibit both FFA conjugation and oxidation, blocking short and long chain FFA utilization for ATP production. https://pubmed.ncbi.nlm.nih.gov/12904852/..." title="12/Recall from tweet #8 that PRIS associates w/ https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> short and long-chain FFAs in the serum. This suggests that propofol can inhibit both FFA conjugation and oxidation, blocking short and long chain FFA utilization for ATP production. https://pubmed.ncbi.nlm.nih.gov/12904852/..." class="img-responsive" style="max-width:100%;"/>
short and long-chain FFAs in the serum. This suggests that propofol can inhibit both FFA conjugation and oxidation, blocking short and long chain FFA utilization for ATP production. https://pubmed.ncbi.nlm.nih.gov/12904852/..." title="12/Recall from tweet #8 that PRIS associates w/ https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> short and long-chain FFAs in the serum. This suggests that propofol can inhibit both FFA conjugation and oxidation, blocking short and long chain FFA utilization for ATP production. https://pubmed.ncbi.nlm.nih.gov/12904852/..." class="img-responsive" style="max-width:100%;"/>



