Now that my Dad is out of the hospital, I feel more comfortable sharing what worked for him: 9 Ivermectin per day for 5 days, Zinc, Vitamin D, Vitamin C, Heparin, Remdesivir. He entered hospital on 3/1. He didn’t get Ivermectin until 3/6. I wish it would have been earlier.
My Dad was mostly on a heated nasal cannula but sometimes was on a bipap. If your loved one has to be on the bipap, I suggest asking the hospital to use Precedex to calm patient. It’s like a wind tunnel. Drugs like Ativan seem to cause a bad reaction with some COVID patients.
Precedex was a lifesaver for keeping my dad calm when he had to be on Bipap. At the 1st hospital, he was kept on bipap for 18 hours and not given food or drink. It was traumatizing. Let hospital know you want your loved one to have control when possible.
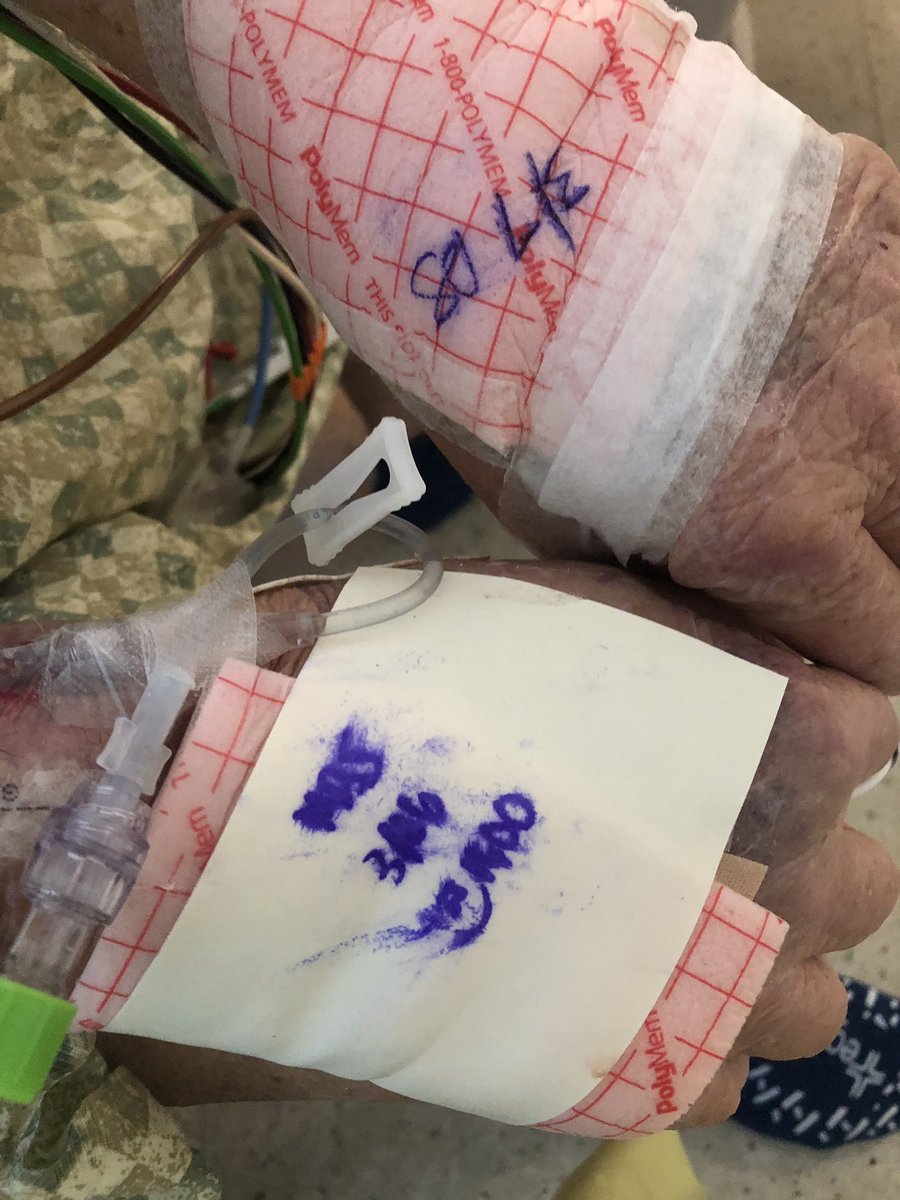
One night his nasal cannula kept falling out while he slept. The nurse was annoyed with having to gown up and go in to fix it. So, 2 male nurses chose to restrain my Dad. We were told later restraining Covid patients isn’t advised. After the night he was restrained, I flipped.
I asked for him to be moved to another hospital but they offered ICU instead. When he got to ICU they bandaged his hands from the damage of the restraints and dated them. I don’t blame them. I wouldn’t want to be blamed for that either.
I’m adamant change needs to happen regarding visitation of Covid patients. Patients need an advocate. The 2nd hospital allowed my mom to stay from 9-9 daily & my Dad was much more relaxed. The first hospital allowed only 30 minutes per day and no visits on Saturday.
I believe the majority of nurses are wonderful, and at the second hospital, ALL were exceptional. The 1st hospital was a ghost town because of visitor policy & that is dangerous to patients in my opinion.
At the first hospital, the best nurse was a traveling nurse. They have a major culture problem there. I was told to seek help from the patient advocate. She was also awful. She had no desire to help my dad. Her only interest was defending nurses
The other major issue is some nurses get tired of gowning up to go deal with Covid patients. They think watching patients on IPad is sufficient. That isn’t patient care. People need human contact and conversation. Watching very sick people on IPad isn’t cutting it.
As a Covid survivor, I can tell you it effected me emotionally. I was very angry and raged. Covid patients need help processing that and being isolated is terrifying.
If you have a Covid + loved one, you have to advocate. Facetime them, call the nurses station, visit any time they allow, ask questions, call the admin office, and do not ever ever sign the order to allow them to vent at any time.
The 1st hospital had given up on my Dad. They told us he was aspirating liquid into his lungs and started making him put a thickener in his drinks and limiting liquids. When he got to the 2nd hospital, they said that was not accurate. The 1st hospital asked is to sign a DNR
Or the paperwork to vent him. After discussions with a friend, I decided to do neither and move him. If there is an emergency and they need to vent, they can call you. I’m so glad I did not give them the option because my dad didn’t need that.
I moved him to the second hospital a week ago today and today he came home. A week ago they told me my dad was aspirating liquid into his lungs, it was day to day and we would likely lose him. Y’all, I’m terrified abt the # of ppl who died unnecessarily from Covid
The 1st hospital looked at my dad and saw a 71 year old man, lymphoma survivor who had just finished chemo, diabetic and decided he wasn’t going to make it. Palliative care is the word they used. They didn’t see a Dad, grandad, husband, best friend & brother.
That’s why you have to advocate. Demand therapies. Everyone hates me at the 1st hospital and that’s fine. I never had to call the 2nd hospital one time. I think that’s because they allow visitors and that means accountability.
Not allowing visits for Covid patients MUST stop. There are ways to do it safely.
Oh one other note: my dad is a lymphoma survivor so we watch his hemoglobin. For 2 days, hospital 1 ran no blood work, none, so they had no idea what any of his numbers were. I confronted them and they said “we can see his vitals” as if that gives same info as bloodwork.
Wrapping it up: advocate and don’t be afraid to move your loved one if needed. The difference in care was amazing. Best thing I did!
One more thing. This was what my mom wore from 9-9 at the 2nd hospital every day. She wasn’t allowed to leave the room. She was glad to do it for my Dad. She’s freaking amazing.
The pic on the left was my Dad 8 days ago when they told me he would likely die. I moved him the next day. The pic on the right was 5 days later. Transfer your loved one if something feels off.
I forgot one therapeutic. My dad was also given convalescent plasma.
I forgot to add to this thread: my dad was fully vaccinated. He received Moderna on 1/6 and 2/2. He tested positive on 3/1 almost a month after second shot .

 Read on Twitter
Read on Twitter