Thread to follow giving overview of new papers from @bmj_latest special collection: & #39; #Covid19: The road to equity and solidarity& #39; https://www.bmj.com/pmac-2021 ">https://www.bmj.com/pmac-2021... cc @CroakeyNews #PMAC2021 @baumfran @WePublicHealth
The collection explores political economy of the response, role of international institutions, overwhelmed health systems, #SDOH, value of indices of preparedness, need for all countries to act together to reduce inequality, protect health, and act on climate #PMAC2021
"As we move forward, it is vital that we explore the drivers of the pandemic, learn from the global response, and become more prepared for the future." Also, you can watch the launch featuring various authors, inc @baumfran https://www.youtube.com/watch?v=mazvOZo22Hg&feature=youtu.be">https://www.youtube.com/watch... #PMAC2021 #HealthEquity https://www.youtube.com/watch...
First up: & #39;Are overwhelmed health systems an inevitable consequence of #COVID19? Experiences from China, Thailand, & New York State& #39;
https://www.bmj.com/content/372/bmj.n83
By">https://www.bmj.com/content/3... Viroj Tangcharoensathien from Thailand & colleagues from US, China and UK. See key messages below.
https://www.bmj.com/content/372/bmj.n83
By">https://www.bmj.com/content/3... Viroj Tangcharoensathien from Thailand & colleagues from US, China and UK. See key messages below.
The research highlights the importance of governance. New York State faced failure of governance on many fronts, plus inconsistent messaging. By contrast, strong and unified governance structures in China & Thailand ensured consistent communications.
"The politicising of covid-19 & poor coordination between federal & state, & state & city governments impeded responses in US compared with China & Thailand. .. universal health coverage in China & Thailand ensured full access to public health interventions & medical treatment.
Also, US libertarian values of emphasising personal liberty and disregarding official advice, and public discourse framing this public health measure as an infringement on personal liberty, meant the decision to wear a mask reflected a political position.
The researchers conclude: "timely and decisive policy decisions, effective and adequately funded public health and social measures, and citizen trust and adherence to these measures are critical elements of effective pandemic control"
What can Australia learn from this study [my commentary]: DON& #39;T BE LIKE THE U.S. Also, #GovernanceReallyMatters. Politicisation of pandemic responses is a threat to public health ping @ScottMorrisonMP @GladysB
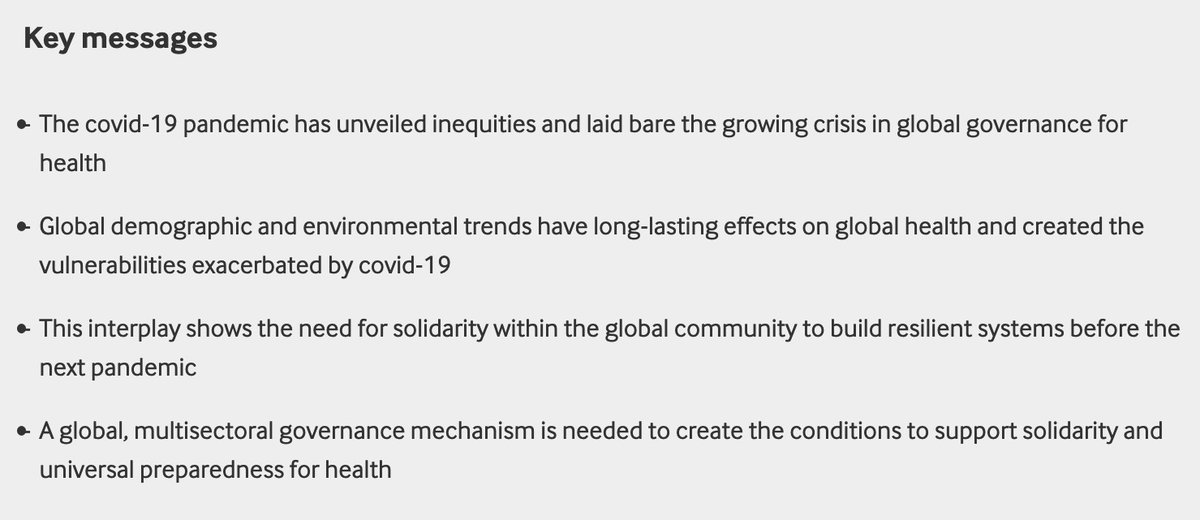
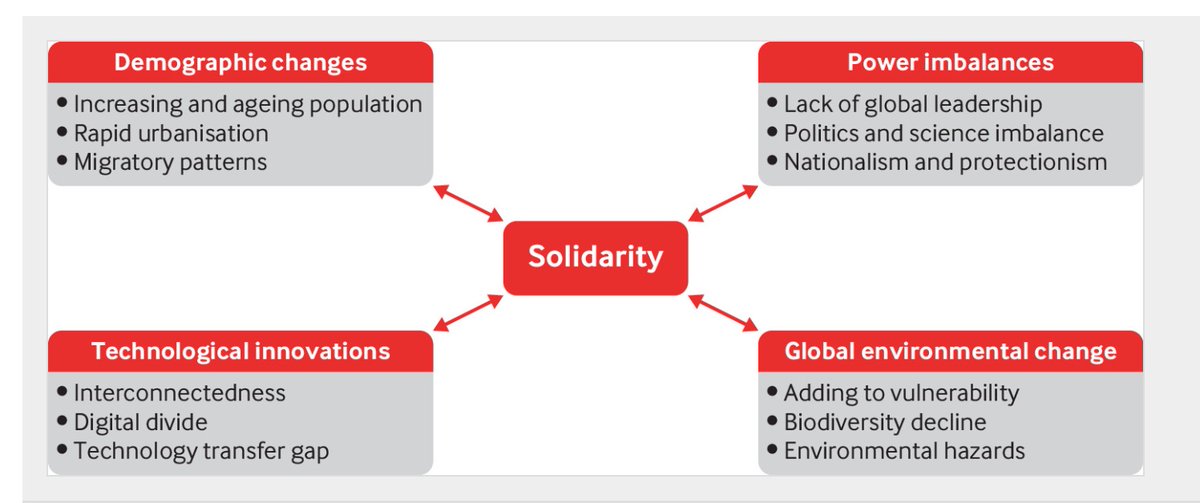
Next article: & #39;Solidarity and universal preparedness for health after #covid19" https://www.bmj.com/content/372/bmj.n59">https://www.bmj.com/content/3... By Göran Tomson and others from Sweden, and colleagues from Uganda, Bangladesh and US. See key messages below
The article identifies four megatrends that have created the vulnerabilities exacerbated by #covid19. eg re the digital divide, research shows that half of the world’s population, including 360 million young people, do not have access to the internet
While social media has shared validated information and contributed to connection during the pandemic, "it has also been a driver of false information, fuelling conspiracies and supporting detrimental social behaviours". cc @mariemcinerney #RegulateDigitalPlatforms
The article says: & #39;Over the past few decades, power imbalances have contributed significantly to inequities in health. many countries have effectively ceded power to international financial institutions & multinational corporations, reducing their capacity to meet health needs.
As well, UN system has weakened; @WHO has seen its authority eroded, with a gradual reduction of financial support from all member states and threatened withdrawal by US. Plus, increased nationalism and protectionism; politics often taking precedence over science.
The authors argue that the interplay between megatrends and covid-19 shows the need for structural responses to the systemic drivers of health and social inequities within and across countries.
"The pandemic should unite the entire global community to build societal resilience to cope with the next crisis... solidarity & unity of action is required to mitigate or reverse the megatrends that have left the world vulnerable to the spread of disease."
What can Australia learn from this article? [...it& #39;s a reminder of the gulf between public health discourse and political discourse...has "solidarity" ever been mentioned at a pandemic press conference in Aus?]
3rd article in the @bmj_latest series: & #39;Political economy of #covid19: extractive, regressive, competitive& #39;: https://www.bmj.com/content/372/bmj.n73">https://www.bmj.com/content/3... By @JesseBump @baumfran & colleagues in Thailand, UK and South Africa. cc @WePublicHealth @CroakeyNews
The article explores historic and contemporary manifestations of colonialism & intersections with the pandemic & argues strongly for global governance reform. Key messages below  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">
The disproportionate impact on poor & marginalised people, and the competitive scramble for vaccines and supplies indicate "a political economy of extraction, following longstanding patterns of exploitation", reflecting colonialism
While the global economic disruption of #COVID19 has harmed poorer people and poorer countries the most, many countries in the global south have public health containment strategies developed through considerable experience with epidemic diseases.
"However, in keeping with the old colonial pattern of the flow of knowledge from north to south, these ideas and strategies have struggled to gain visibility in mainstream global health discussions."
The authors call for G7 and G20 countries to cross subsidise vaccine purchases for low and middle income countries and ensure long term availability by enforcing compulsory licensing as they have already pledged to do through the World Trade Organization.
"The shared disaster of the covid-19 pandemic has drawn attention to the many regressive realities of our world, each one calling for immediate reform in the governance of global health....
"Without such measures, the unfair, extractive, and regressive patterns of the past will continue to plague the present."
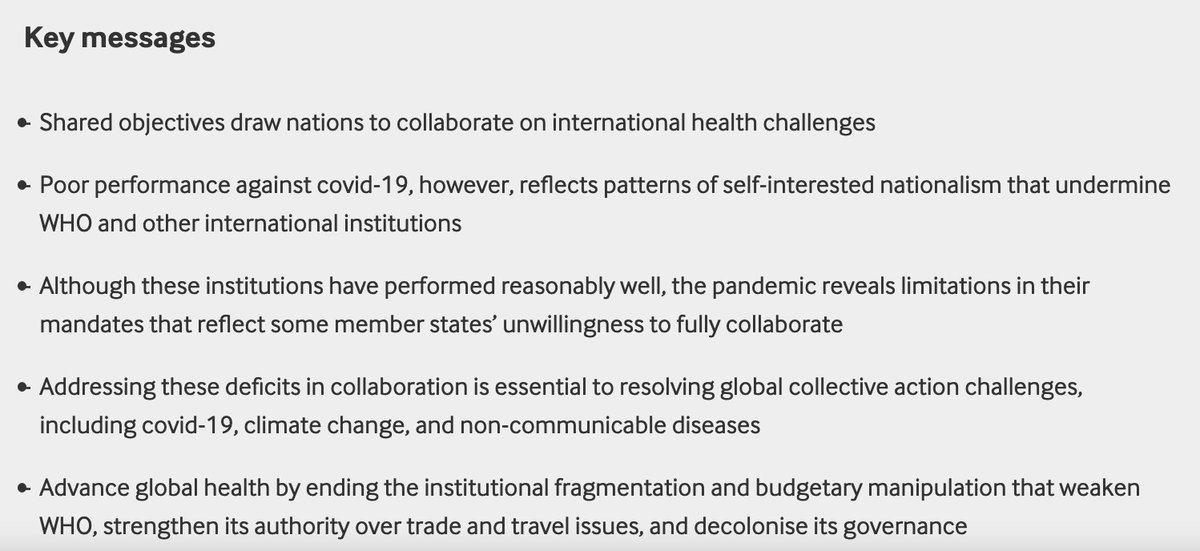
4th article in the series: & #39;International collaboration and covid-19: what are we doing and where are we going?& #39;. https://www.bmj.com/content/372/bmj.n180">https://www.bmj.com/content/3... By @JesseBump & colleagues from Norway, Sweden & UK. Key messages below  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">
I recommend reading this article in full; it& #39;s really impt (and also I did not know the story about the World Bank and pandemic bonds before) https://www.bmj.com/content/372/bmj.n180">https://www.bmj.com/content/3...
It ends with 3 clear calls to action: 1. member states of @WHO must end the systematic weakening of WHO; 2. they must support its independence - increase core @WHO budget and build its authority over trade and travel related issues..
And thirdly, states must grant @WHO powers to hold members accountable, including for overcoming deficiencies in national data, and by decolonising its governance to address the undue influence of a small number of powerful member states.
5th article in the series: & #39;Explaining covid-19 performance: what factors might predict national responses?& #39; https://www.bmj.com/content/372/bmj.n91">https://www.bmj.com/content/3... By @baumfran @drtobyfreeman & @Flinders @ANURegNet colleagues, & others from US, Brazil, Belgium, Vietnam, South Africa, UK & Peru.  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">
This is another must-read. The paper notes that 2 measures for how well countries were prepared for pandemics – the Global Health Security Index & the Epidemic Preparedness Index – had both rated US and UK highly, although they went on to have had disastrous pandemic outcomes.
The researchers propose 10 factors that may explain why the GHSI failed to predict performance in the covid-19 pandemic; and provide guidance for the development of a new index on preparedness.
[As a side note, the team builds on an existing network of researchers—the Punching Above Weight Network, which has considered why some countries achieve higher health status than their economic performance would suggest]
A summary of the 10 factors: 1. Limited consideration of globalisation, geography, and global governance.
The GSHI measures the performance of individual nations but did not consider the importance of geography. For example, islands nations like Oz could close their borders
The GSHI measures the performance of individual nations but did not consider the importance of geography. For example, islands nations like Oz could close their borders
2. The index is biased to high income countries through its emphasis on biosecurity and more authoritarian approaches to public health. Yet the pandemic has highlighted the importance of more comprehensive, social determinants driven, participatory and rights based approaches
3. The index failed to assess health system capacity.
Nations with universal publicly funded health systems that were not financially distressed and had strong public health capacity seem to have been relatively well prepared for covid-19: eg Thailand, Vietnam, Australia, NZ.
Nations with universal publicly funded health systems that were not financially distressed and had strong public health capacity seem to have been relatively well prepared for covid-19: eg Thailand, Vietnam, Australia, NZ.
"Conversely, the pandemic highlighted the weaknesses of fragmented systems relying on for-profit healthcare providers, such as in the US..[and England]".
4. The index overlooked the role that political leadership and ideology plays in shaping public health responses. The GHSI rated NZ lower than many other high income countries. Yet many praise @jacindaardern for strong political leadership during #COVID19, say the researchers.
The paper says egs of poor governance during covid-19 include "growing concern about corruption in the procurement of essential equipment and the absence of transparency when contracting with private companies".
"Given the vital importance of trust during a pandemic, political leaders who promote transparent government are more likely to mount a more effective response," the researchers say.
5. Importance of context overlooked, ie future predictive work would benefit from a qualitative, context assessment of each country, informed by a range of expertise.
6. Limits of national wealth as predictive factor.
6. Limits of national wealth as predictive factor.
"Lower income countries may allocate their scarce resources more appropriately and tailored to context." Rwanda and Vietnam cited as examples of low income countries using their resources efficiently and innovatively to achieve good health.
7. Future iterations of the GHSI should include measures of the scale and nature of inequalities within a country.
Importance of social security provisions 8. Pandemic has highlighted importance of social security provisions yet the GHSI does not consider them in its assessment
Importance of social security provisions 8. Pandemic has highlighted importance of social security provisions yet the GHSI does not consider them in its assessment
"In many countries the availability of sick leave has been an effective public health measure as people without this provision have found it difficult to follow public health advice to self-isolate. Including measures of social protection would improve future indices."
9. Civil society capacity was not assessed by GHSI, yet social solidarity built on civil society engagement can offer protection even where trust in government is weak
And the final point, #10: Although GHSI assessed the theoretical capacity of a country to respond to a pandemic it did not examine the actual capacity and willingness to respond - eg US scored high on applied epidemiology training programs BUT...
...political intervention prevented CDC from applying epidemiological science to responses to the pandemic.
"A complex system is only as strong as its weakest point."
"A complex system is only as strong as its weakest point."
The authors conclude: "The crucial lesson from the covid-19 pandemic is that an effective response does not rely just on a strong public health system but also requires a society that is fair and offers all its citizens and residents social and economic security."
Next article in the series: & #39;Covid-19—a rehearsal to build a greener and healthier society& #39;: https://www.bmj.com/content/372/bmj.n127">https://www.bmj.com/content/3... By researchers in Sweden, Côte d’Ivoire, Switzerland. See key messages  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">
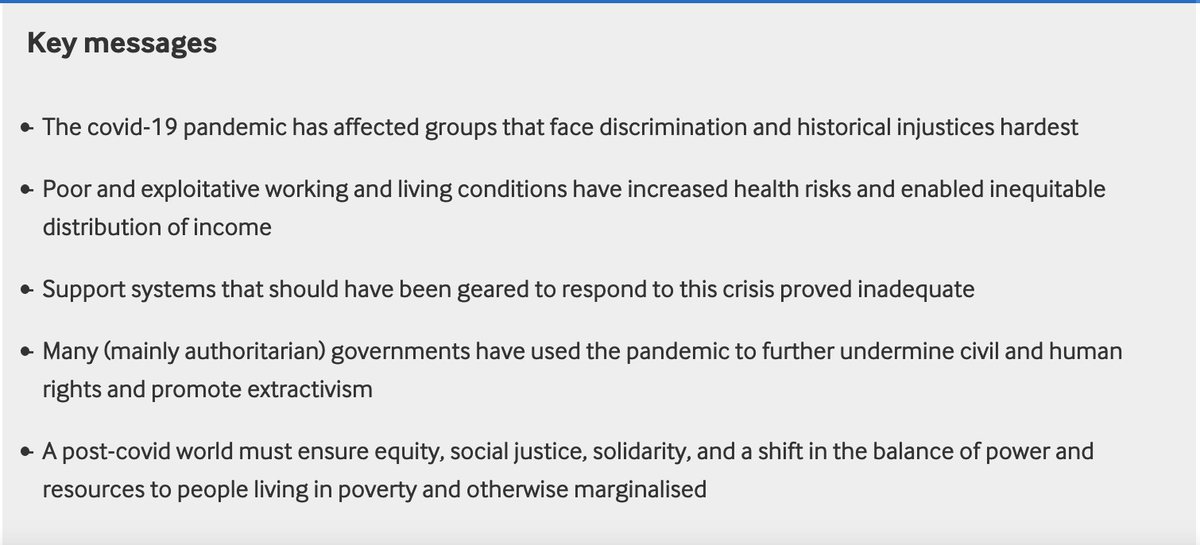
Final article in the series: & #39;Covid-19 pandemic and the social determinants of health& #39;: https://www.bmj.com/content/372/bmj.n129">https://www.bmj.com/content/3... #SDOH See key messages  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">
@threadreaderapp Please unroll this thread

 Read on Twitter
Read on Twitter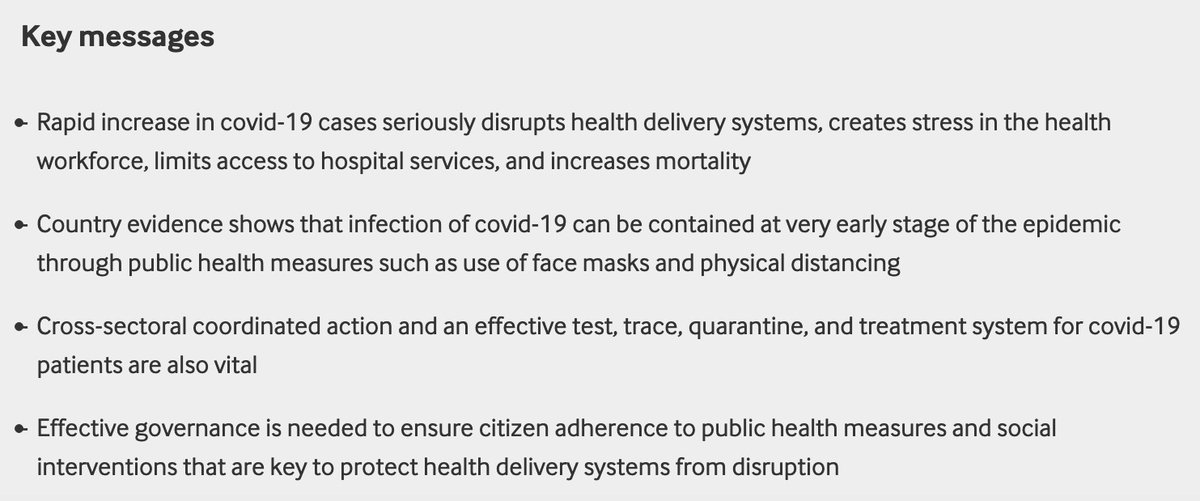
 " title="The article explores historic and contemporary manifestations of colonialism & intersections with the pandemic & argues strongly for global governance reform. Key messages below https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">" class="img-responsive" style="max-width:100%;"/>
" title="The article explores historic and contemporary manifestations of colonialism & intersections with the pandemic & argues strongly for global governance reform. Key messages below https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">" class="img-responsive" style="max-width:100%;"/>
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">" title="4th article in the series: & #39;International collaboration and covid-19: what are we doing and where are we going?& #39;. https://www.bmj.com/content/3... By @JesseBump & colleagues from Norway, Sweden & UK. Key messages below https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">" class="img-responsive" style="max-width:100%;"/>
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">" title="4th article in the series: & #39;International collaboration and covid-19: what are we doing and where are we going?& #39;. https://www.bmj.com/content/3... By @JesseBump & colleagues from Norway, Sweden & UK. Key messages below https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">" class="img-responsive" style="max-width:100%;"/>
 " title="5th article in the series: & #39;Explaining covid-19 performance: what factors might predict national responses?& #39; https://www.bmj.com/content/3... By @baumfran @drtobyfreeman & @Flinders @ANURegNet colleagues, & others from US, Brazil, Belgium, Vietnam, South Africa, UK & Peru. https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">" class="img-responsive" style="max-width:100%;"/>
" title="5th article in the series: & #39;Explaining covid-19 performance: what factors might predict national responses?& #39; https://www.bmj.com/content/3... By @baumfran @drtobyfreeman & @Flinders @ANURegNet colleagues, & others from US, Brazil, Belgium, Vietnam, South Africa, UK & Peru. https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">" class="img-responsive" style="max-width:100%;"/>
 " title="Next article in the series: & #39;Covid-19—a rehearsal to build a greener and healthier society& #39;: https://www.bmj.com/content/3... By researchers in Sweden, Côte d’Ivoire, Switzerland. See key messages https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">" class="img-responsive" style="max-width:100%;"/>
" title="Next article in the series: & #39;Covid-19—a rehearsal to build a greener and healthier society& #39;: https://www.bmj.com/content/3... By researchers in Sweden, Côte d’Ivoire, Switzerland. See key messages https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">" class="img-responsive" style="max-width:100%;"/>
 " title="Final article in the series: & #39;Covid-19 pandemic and the social determinants of health& #39;: https://www.bmj.com/content/3... #SDOH See key messages https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">" class="img-responsive" style="max-width:100%;"/>
" title="Final article in the series: & #39;Covid-19 pandemic and the social determinants of health& #39;: https://www.bmj.com/content/3... #SDOH See key messages https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">" class="img-responsive" style="max-width:100%;"/>


