For the first question: No trials showing higher pCR w/ higher dose. Trials are actually remarkably consistent (no difference):
INTERACT https://pubmed.ncbi.nlm.nih.gov/31005204/
RECTAL-BOOST">https://pubmed.ncbi.nlm.nih.gov/31005204/... https://pubmed.ncbi.nlm.nih.gov/32565319/
Dose-Effect">https://pubmed.ncbi.nlm.nih.gov/32565319/... https://pubmed.ncbi.nlm.nih.gov/22592048/
https://pubmed.ncbi.nlm.nih.gov/22592048/... href="https://twtext.com//hashtag/jc"> #jc questions #radonc https://twitter.com/CarmeloT2681/status/1330177386592301057">https://twitter.com/CarmeloT2...
INTERACT https://pubmed.ncbi.nlm.nih.gov/31005204/
RECTAL-BOOST">https://pubmed.ncbi.nlm.nih.gov/31005204/... https://pubmed.ncbi.nlm.nih.gov/32565319/
Dose-Effect">https://pubmed.ncbi.nlm.nih.gov/32565319/... https://pubmed.ncbi.nlm.nih.gov/22592048/
pCR doesn& #39;t matter to the patient! Only OS or QoL does! And pCR / tumour regression is not a surrogate for radiotherapy effects on OS, so why should we care about it? #radonc #jc
https://pubmed.ncbi.nlm.nih.gov/25611452/ ">https://pubmed.ncbi.nlm.nih.gov/25611452/... https://pubmed.ncbi.nlm.nih.gov/26723110/ ">https://pubmed.ncbi.nlm.nih.gov/26723110/...
If you think about it, we are actually unlikely to see a dose-response relationship for rectal cancer in the (neo-)adjuvant setting: Even if there exists a dose-response relationship, it must be very shallow https://twitter.com/cancerphysicist/status/1268839637889490945?s=20">https://twitter.com/cancerphy...
(Side note: pCR / tumour regression / neoadjuvant rectal score *might* be a surrogate for chemotherapy effects on OS or PFS, but not validated on trial level:
https://pubmed.ncbi.nlm.nih.gov/29206996/
https://pubmed.ncbi.nlm.nih.gov/29206996/... href=" https://pubmed.ncbi.nlm.nih.gov/29718095/
And">https://pubmed.ncbi.nlm.nih.gov/29718095/... data are inconsistent
https://pubmed.ncbi.nlm.nih.gov/19759186/
https://pubmed.ncbi.nlm.nih.gov/19759186/... href="https://twtext.com//hashtag/radonc"> #radonc #jc)
https://pubmed.ncbi.nlm.nih.gov/29206996/
And">https://pubmed.ncbi.nlm.nih.gov/29718095/... data are inconsistent
https://pubmed.ncbi.nlm.nih.gov/19759186/
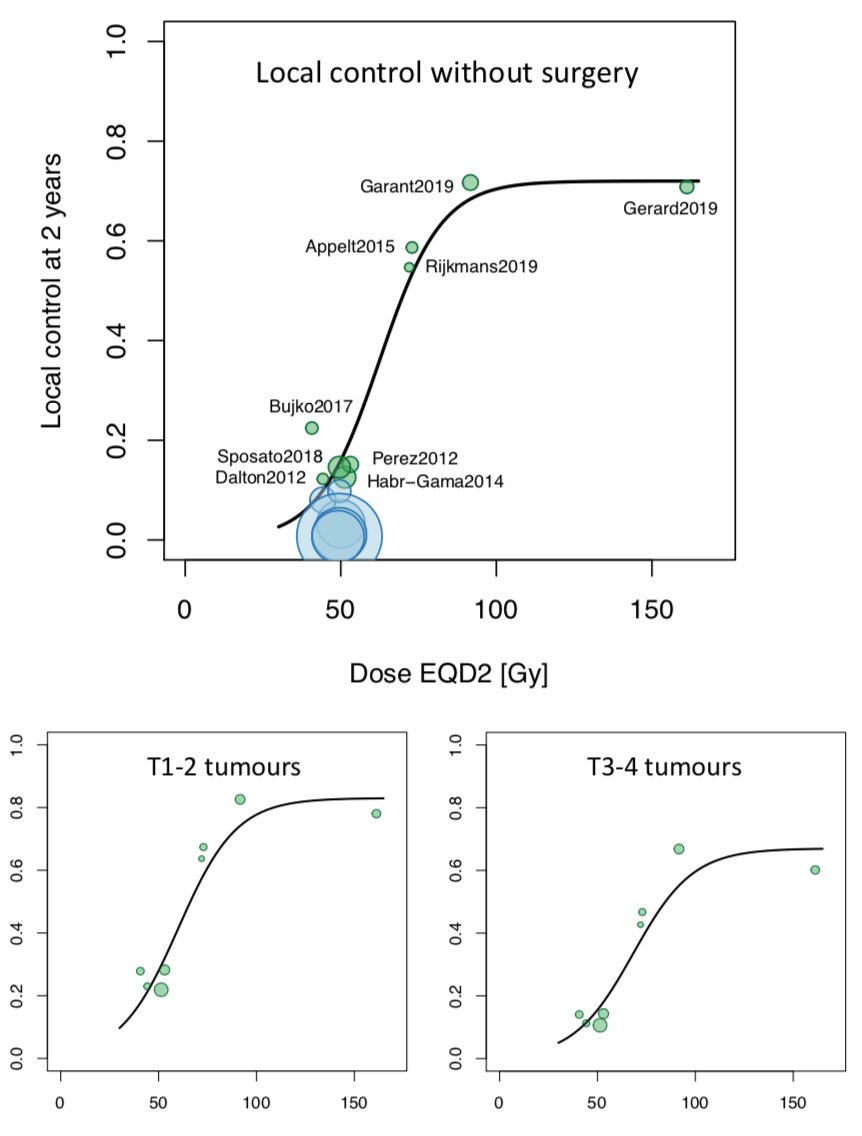
So what matters to patients? Organ preservation (NOM) would - but that depends on
1) clinical complete response (cCR), and
2) long term local control without surgery
#radonc #jc
1) clinical complete response (cCR), and
2) long term local control without surgery
#radonc #jc
Can we get more cCR with higher RT dose? pCR is different from cCR, so we can& #39;t rely just on the trials examining pCR. We only have the (old) data from Lyon R 96-02:
https://pubmed.ncbi.nlm.nih.gov/22579379/ ">https://pubmed.ncbi.nlm.nih.gov/22579379/... #radonc #jc
https://pubmed.ncbi.nlm.nih.gov/22579379/ ">https://pubmed.ncbi.nlm.nih.gov/22579379/... #radonc #jc
On the other hand, the trials quoted above (INTERACT, RECTAL-BOOST, Dose-Effect) are consistent in showing an effect of dose escalation on tumour regression (TRG1-2). OR=1.6, OR=2.7, OR=1.9. This is still path endpoint, though, so still doesn& #39;t matter to patients #radonc #jc
There are ongoing trials testing radiation dose escalation for organ preservation / NOM:
APHRODITE https://ctru.leeds.ac.uk/aphrodite/
WW3">https://ctru.leeds.ac.uk/aphrodite... https://clinicaltrials.gov/ct2/show/NCT04095299
So">https://clinicaltrials.gov/ct2/show/... we have to wait for the outcome of these https://abs.twimg.com/emoji/v2/... draggable="false" alt="😊" title="Lächelndes Gesicht mit lächelnden Augen" aria-label="Emoji: Lächelndes Gesicht mit lächelnden Augen">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="😊" title="Lächelndes Gesicht mit lächelnden Augen" aria-label="Emoji: Lächelndes Gesicht mit lächelnden Augen">
#radonc #jc
APHRODITE https://ctru.leeds.ac.uk/aphrodite/
WW3">https://ctru.leeds.ac.uk/aphrodite... https://clinicaltrials.gov/ct2/show/NCT04095299
So">https://clinicaltrials.gov/ct2/show/... we have to wait for the outcome of these
#radonc #jc
In the meantime, here are some data based on a literature-based meta-analyses #radonc #jc
https://www.estro.org/Congresses/ESTRO-2020/413/posterhighlights5cl-gi/543/istherearadiationdose-responserelationshipfornon-o">https://www.estro.org/Congresse...
https://www.estro.org/Congresses/ESTRO-2020/413/posterhighlights5cl-gi/543/istherearadiationdose-responserelationshipfornon-o">https://www.estro.org/Congresse...

 Read on Twitter
Read on Twitter