THREAD: 5yrs ago we began the TRUST study. Excited to see it finally published in @BMJ_Qual_Saf . This kicked off my interest in using simulation to support patient safety and simulation-informed clinical design.
Here’s some thoughts & reflections
https://qualitysafety.bmj.com/content/early/2020/10/23/bmjqs-2020-011363.info">https://qualitysafety.bmj.com/content/e...
Here’s some thoughts & reflections
https://qualitysafety.bmj.com/content/early/2020/10/23/bmjqs-2020-011363.info">https://qualitysafety.bmj.com/content/e...
2/ Study goal = identify/quantify latent safety threats during trauma ISS & analyze using framework analysis
We published other data including tracking movement within the clinical space https://stel.bmj.com/content/5/2/78
&">https://stel.bmj.com/content/5... debriefing content during systems sim.
https://stel.bmj.com/content/early/2020/08/07/bmjstel-2020-000650.info">https://stel.bmj.com/content/e...
We published other data including tracking movement within the clinical space https://stel.bmj.com/content/5/2/78
&">https://stel.bmj.com/content/5... debriefing content during systems sim.
https://stel.bmj.com/content/early/2020/08/07/bmjstel-2020-000650.info">https://stel.bmj.com/content/e...
3/ This study was only possible with substantial support from @UnityHealthTO , our dept & @Sim_StMikes
My mentor, @HumanFact0rz taught me the importance of pitching an idea to the right people. When we started simulation for systems eval & patient safety was uncommon
My mentor, @HumanFact0rz taught me the importance of pitching an idea to the right people. When we started simulation for systems eval & patient safety was uncommon
4/ Having an easily memorable name to a project is key. Who doesn’t want to be part of a study called “TRUST”! But seriously, naming the study was key when communicating to stakeholders.
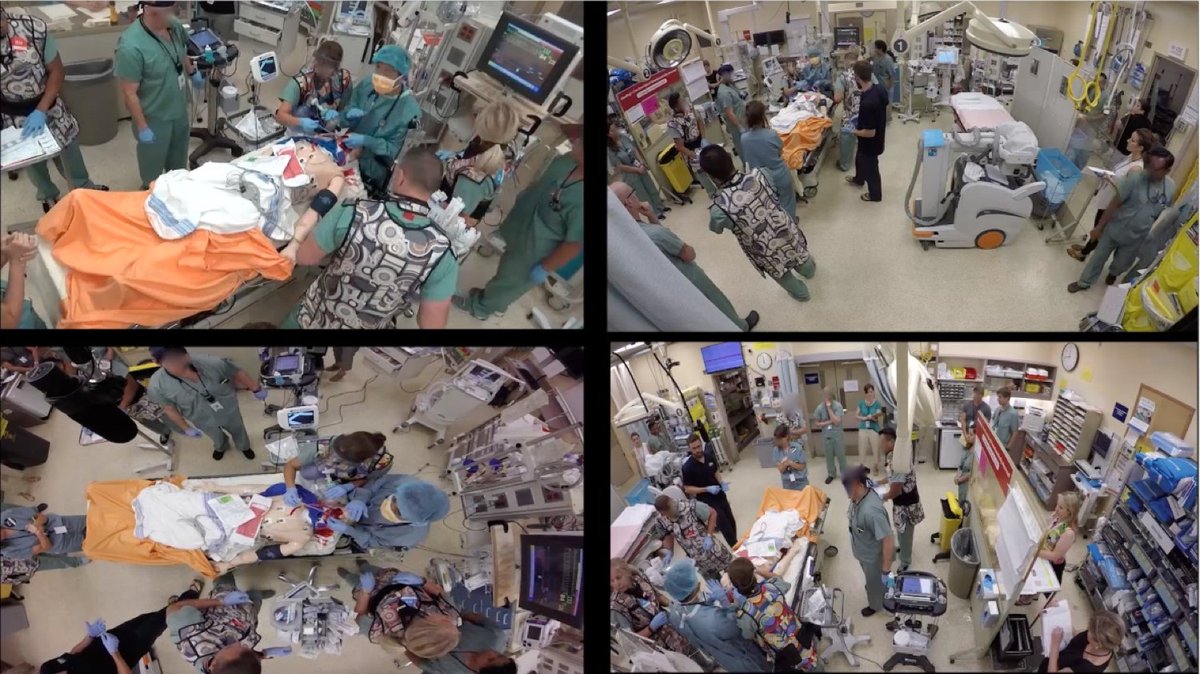
5/ We spent hours building capacity and interest in what was previously thought to be “impossible” = regular, unannounced video-recorded in situ simulations at a Level 1 trauma centre. This represented a big shift for us. It was novel, but now our dept fully embraces #simulation
6/ I wont lie, we did reframe questions of “can we do this?” to statement/question combos like “when we run the simulation, how can we get your support for this important study?”
7/ We pulled together a multi-disciplinary team which was critical. Having a research coordinator, like the amazing @MelissaAMcG was invaluable. She consented 100s of possible participants and was a logistical magician.
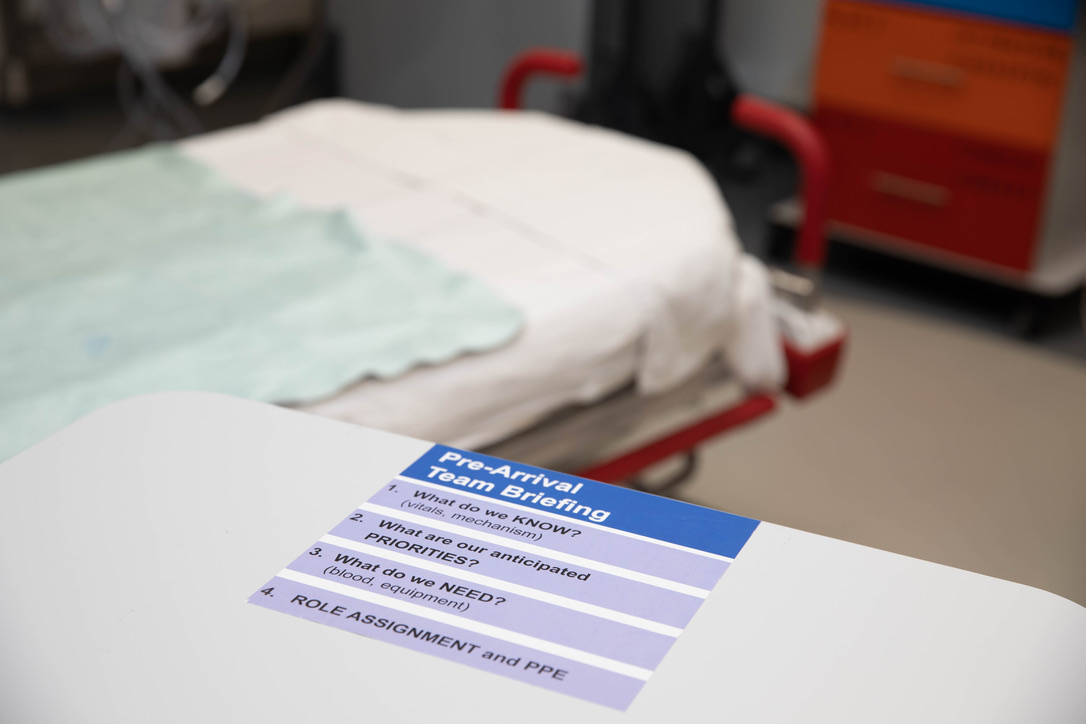
8/ A key partnership was with human factors experts - Mark Fan & Patricia Trbovich. They opened our eyes to new ways of looking at work.
Work as imagined is rarely the same as work as done.
Work as imagined is rarely the same as work as done.
9/ Now the study.
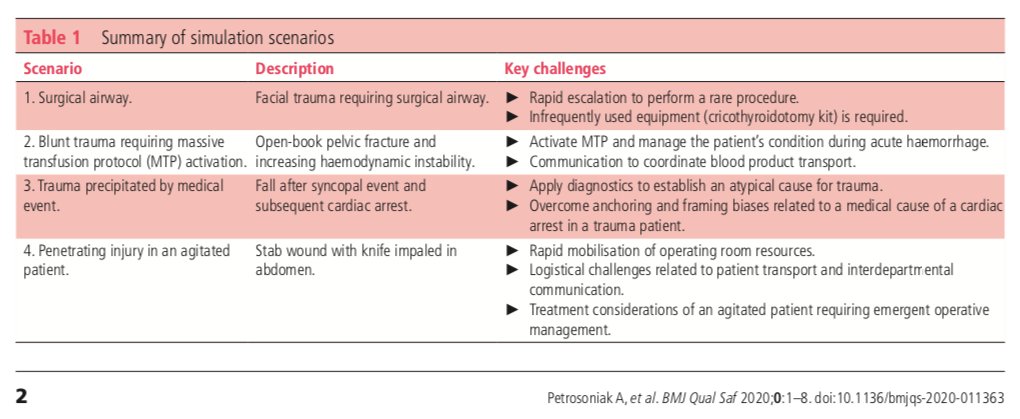
We believe that with simulation there’s no such thing as “rare” events anymore. We can literally recreate a surgical airway every week if needed. We prospectively designed cases to elicit LSTs based on review of adverse events
We believe that with simulation there’s no such thing as “rare” events anymore. We can literally recreate a surgical airway every week if needed. We prospectively designed cases to elicit LSTs based on review of adverse events
10/ This can be conceptualized as Living M&Ms. Rather than just look back at problems (relying on recall), the ability to simulate the same case repeatedly, varying a few environmental, system factors, generates a rich data set that can be inputted towards system improvement
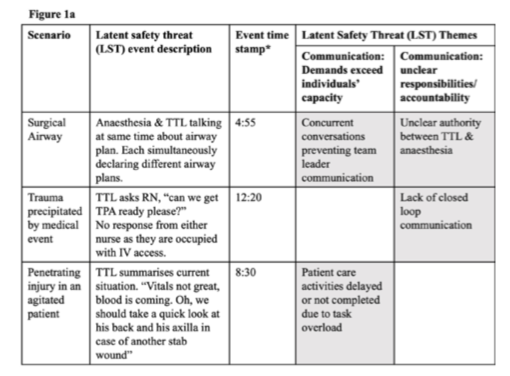
11/ Using a framework analysis allowed us to identify how a single LST event could be related to multiple themes. This is important once we look to solutions. We also prioritized each LST theme using a hazard matrix
12/ We identified 7 themes, further classified into 38 subthemes. This is much more detailed than existing literature as its grounded on HF expert analysis.
13/ A deep understanding of each LST is critical. E.g. significant delay to perform a cric in one session. If only a comms issue then solution could be more team training…but physical workspace was also identified, so we redesigned the workspace which improves both problems.

 Read on Twitter
Read on Twitter