Using lung #POCUS during a COVID surge
Recognizing a (?) rare presentation of severe preeclampsia
The central importance of racism in American health.
And an injunction to vote to save lives.
(Full, enthusiastic pt permission)
1/20
Recognizing a (?) rare presentation of severe preeclampsia
The central importance of racism in American health.
And an injunction to vote to save lives.
(Full, enthusiastic pt permission)
1/20
30s woman, had a C-section 7 days ago, discharged feeling fine
Now in the ED with a severe headache, and marked marked HTN.
LFTs up
Hx of preeclampsia with a prior pregnancy, so … Dx made?
2/20
Now in the ED with a severe headache, and marked marked HTN.
LFTs up
Hx of preeclampsia with a prior pregnancy, so … Dx made?
2/20
Well, she *also* has dyspnea on exertion, orthopnea, and peripheral edema.
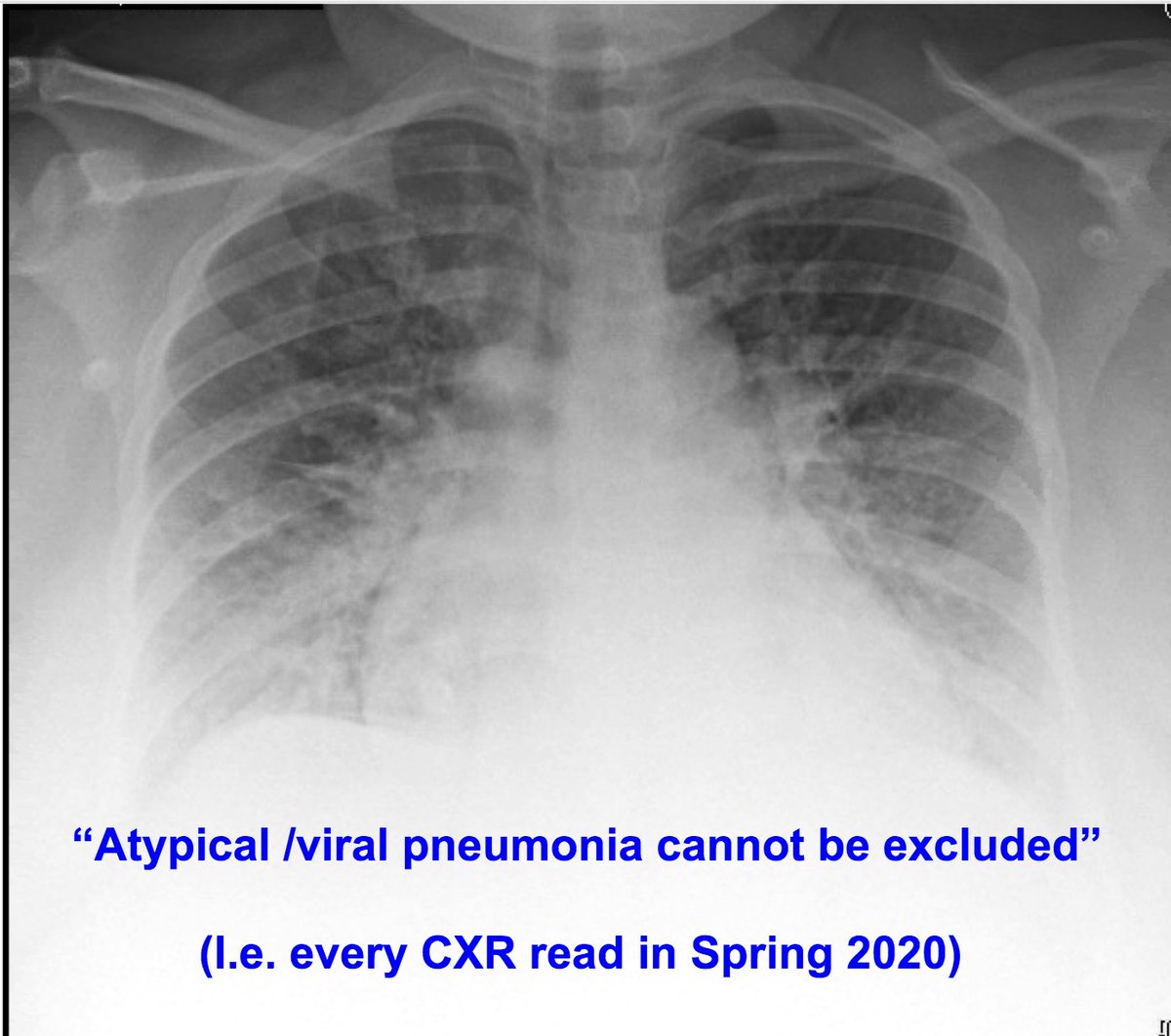
This is at the height of our COVID surge in the spring, mind you.
PCR is (-), but the CXR …
3/20
This is at the height of our COVID surge in the spring, mind you.
PCR is (-), but the CXR …
3/20
… is interpreted as “suggestive of viral pneumonia”
Furthermore, #POCUS of the lungs shows characteristic interstitial signs consistent with COVID pneumonia.
4/20
Furthermore, #POCUS of the lungs shows characteristic interstitial signs consistent with COVID pneumonia.
4/20
So, preeclampsia *and* COVID?
Doesn’t satisfy Occam.
OTOH, “COVID + ___” was a very common Dx at that time
Admitted a pt with femur Fx + COVID around that time, so plausible...
5/20
Doesn’t satisfy Occam.
OTOH, “COVID + ___” was a very common Dx at that time
Admitted a pt with femur Fx + COVID around that time, so plausible...
5/20
But the #POCUS shows some pretty good pleural effusions as well, which would be unusual for COVID PNA.
Also, the IVC is plethoric, which would be somewhat odd for COVID PNA
Hmm.
COVID may not be causing the hypoxia!
6/20
Also, the IVC is plethoric, which would be somewhat odd for COVID PNA
Hmm.
COVID may not be causing the hypoxia!
6/20
Peripartum cardiomyopathy would explain these findings of course
But the cardiac #POCUS shows pretty vigorous systolic activity
7/20
But the cardiac #POCUS shows pretty vigorous systolic activity
7/20
So, does this echo in a woman with postpartum preeclampsia mean that the edema is non-cardiogenic?
Told you it’s COVID
Something doesn’t seem right...
8/20
Told you it’s COVID
Something doesn’t seem right...
8/20
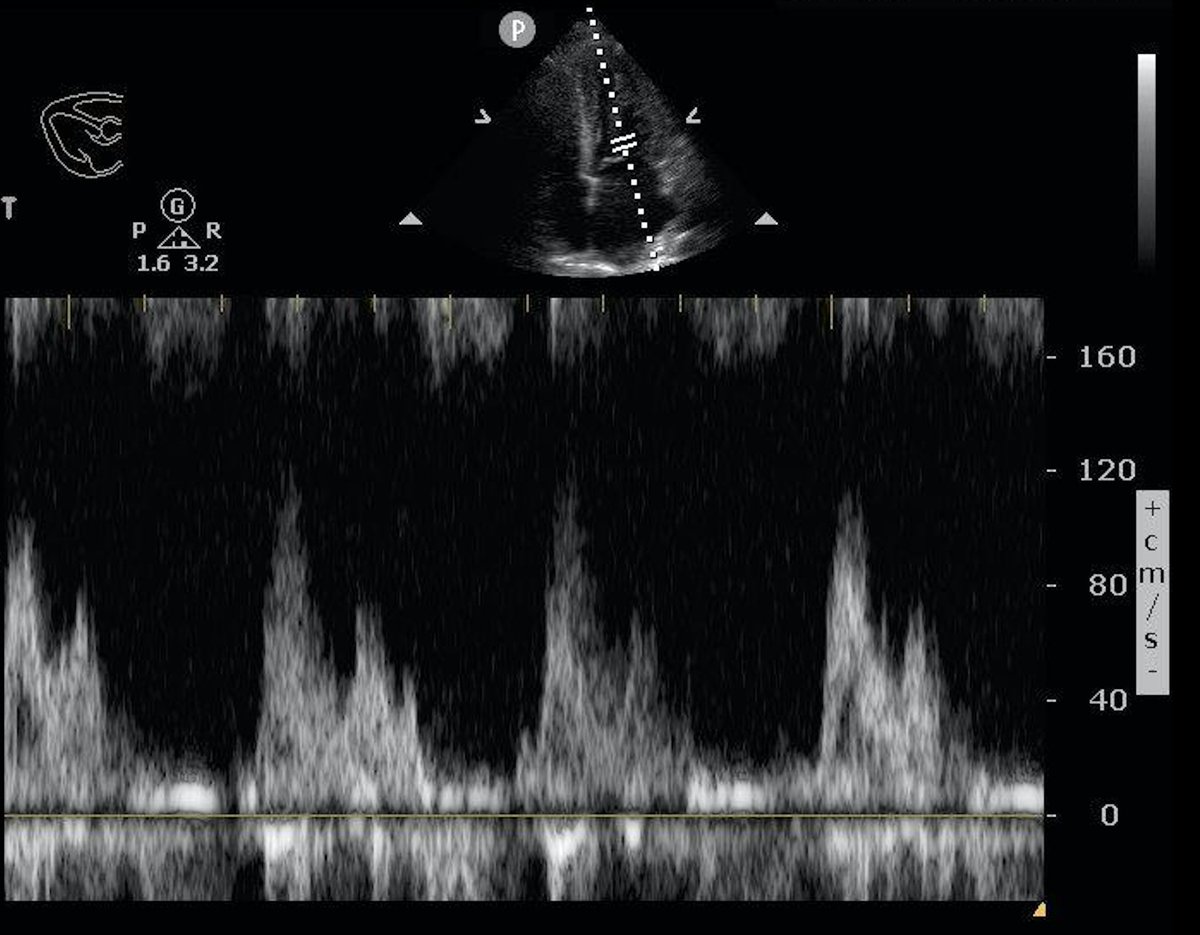
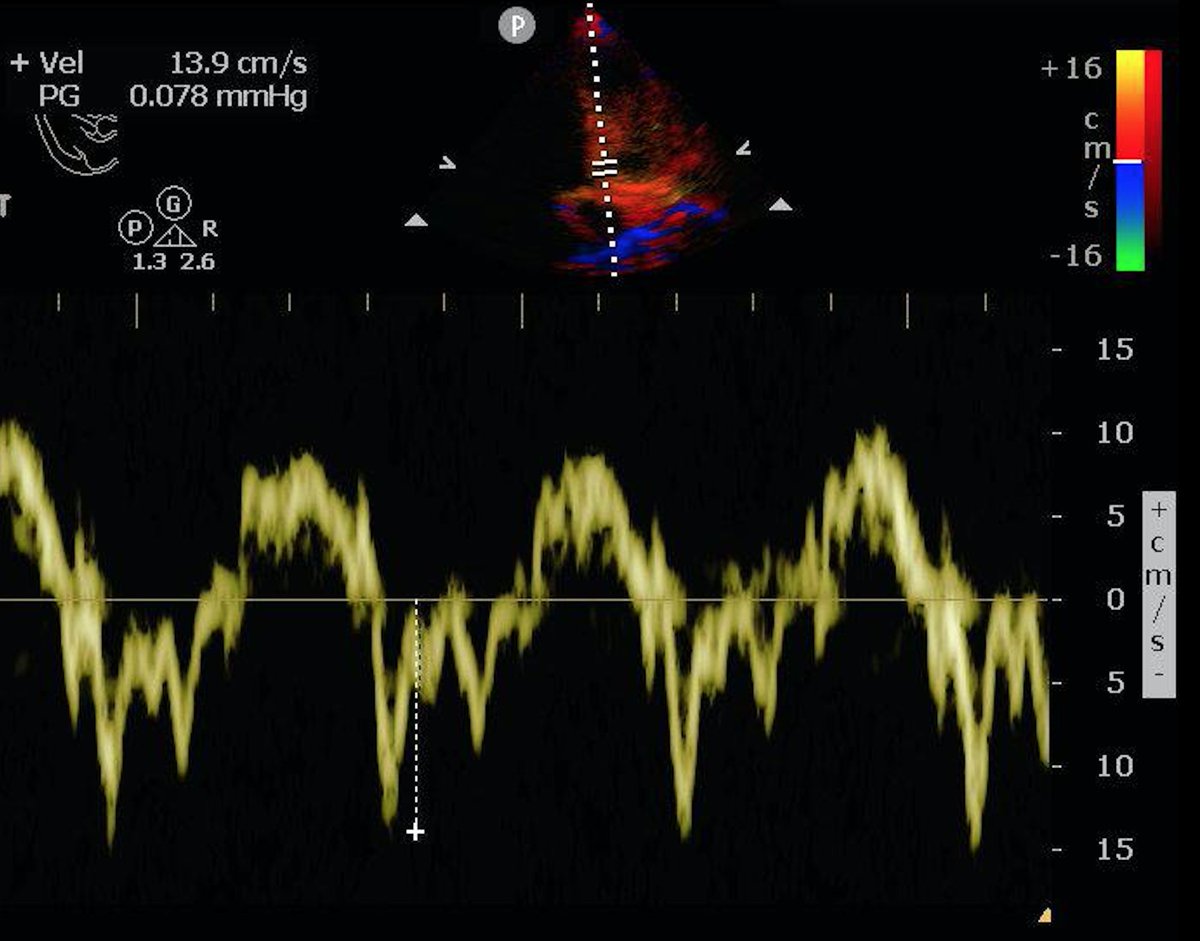
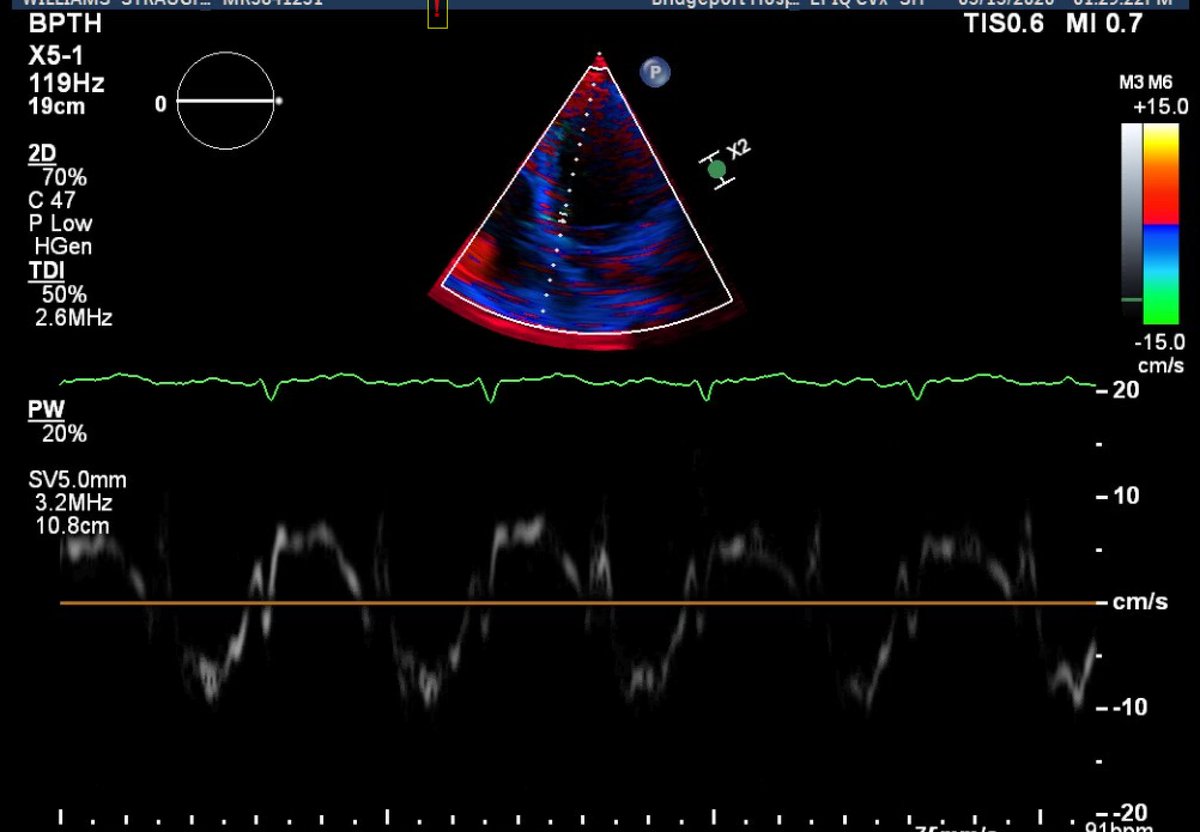
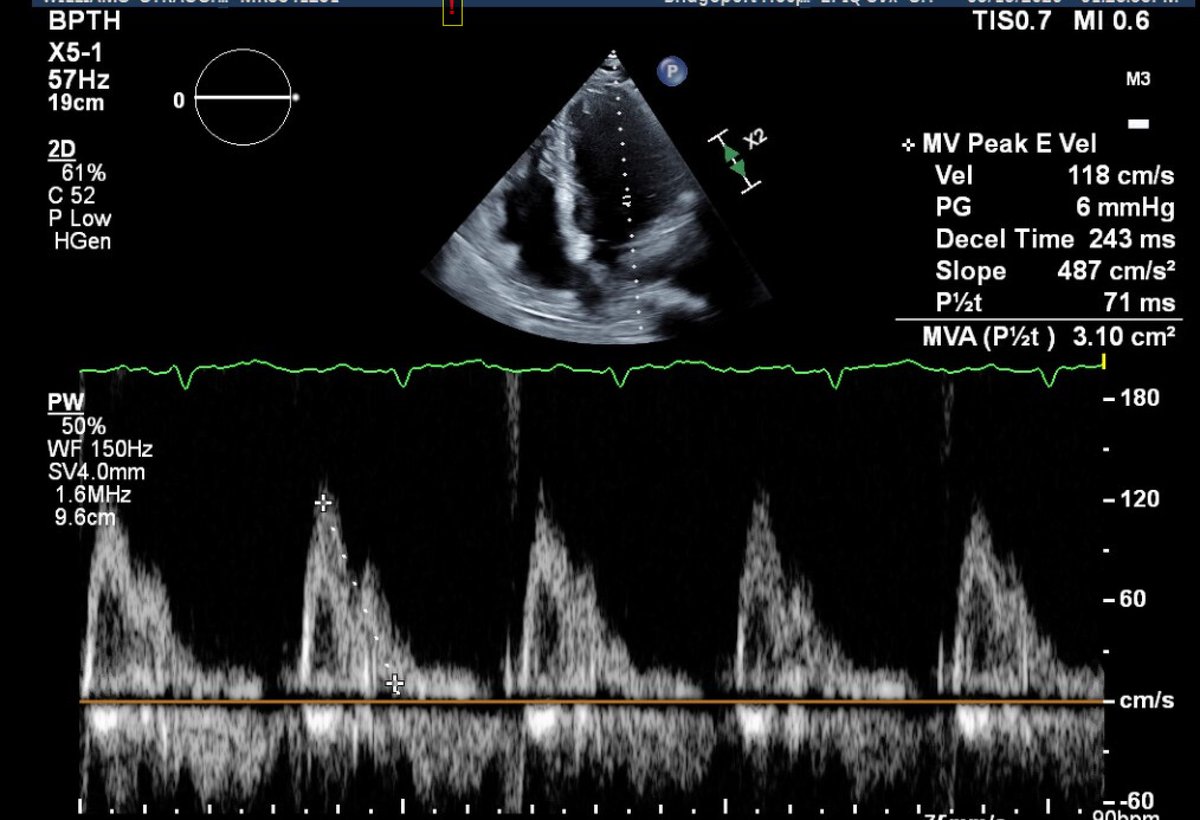
So back to the cardiac #POCUS
Some Doppler was shot, E and e’ waves recorded.
E around 120, maybe higher
E’ around 12-15
Making the E/e’ range come out around 8-10
9/20
Some Doppler was shot, E and e’ waves recorded.
E around 120, maybe higher
E’ around 12-15
Making the E/e’ range come out around 8-10
9/20
Generally need septal E/e’ > 15 to *properly* diagnose diastolic dysfunction.
But 8-10 ain’t normal in this population
Women < 39 y.o. usually have mean E/e’ around 5.5
https://pubmed.ncbi.nlm.nih.gov/29911006/
10/20">https://pubmed.ncbi.nlm.nih.gov/29911006/...
But 8-10 ain’t normal in this population
Women < 39 y.o. usually have mean E/e’ around 5.5
https://pubmed.ncbi.nlm.nih.gov/29911006/
10/20">https://pubmed.ncbi.nlm.nih.gov/29911006/...
In fact some experts are concerned that these diastolic criteria are too insensitive in this population...
https://link.springer.com/article/10.1007/s10554-020-01866-w
…">https://link.springer.com/article/1... and that E/e’ > 9.5 might be a better threshold in post-partum women
https://pubs.asahq.org/anesthesiology/article/120/4/906/11874/Lung-Ultrasound-Predicts-Interstitial-Syndrome-and
10/20">https://pubs.asahq.org/anesthesi...
https://link.springer.com/article/10.1007/s10554-020-01866-w
…">https://link.springer.com/article/1... and that E/e’ > 9.5 might be a better threshold in post-partum women
https://pubs.asahq.org/anesthesiology/article/120/4/906/11874/Lung-Ultrasound-Predicts-Interstitial-Syndrome-and
10/20">https://pubs.asahq.org/anesthesi...
But eh why care about diastolic function in our patient?
Because severe preeclampsia can cause pulmonary edema with *normal* EF!
And although this used to be thought of as rare, it can be seen in up to *10%* of women with severe preeclampsia
https://www.onlinejacc.org/content/72/1/1
11/20">https://www.onlinejacc.org/content/7...
Because severe preeclampsia can cause pulmonary edema with *normal* EF!
And although this used to be thought of as rare, it can be seen in up to *10%* of women with severe preeclampsia
https://www.onlinejacc.org/content/72/1/1
11/20">https://www.onlinejacc.org/content/7...
Also.
Our patient’s pro-BNP came back at 563
This would be diagnostically high for her age:
https://pubmed.ncbi.nlm.nih.gov/29544601/
In">https://pubmed.ncbi.nlm.nih.gov/29544601/... NON-preeclamptic women,the BNP peaks at a mean of 158 in post-partum women.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5683168/
So">https://www.ncbi.nlm.nih.gov/pmc/artic... 563 supports acute heart failure
12/20
Our patient’s pro-BNP came back at 563
This would be diagnostically high for her age:
https://pubmed.ncbi.nlm.nih.gov/29544601/
In">https://pubmed.ncbi.nlm.nih.gov/29544601/... NON-preeclamptic women,the BNP peaks at a mean of 158 in post-partum women.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5683168/
So">https://www.ncbi.nlm.nih.gov/pmc/artic... 563 supports acute heart failure
12/20
Further evidence on the comprehensive echo a day later...
-> increased wall thickness
-> increased indexed LA volume
-> E/e’ around 12
… supportive of HFpEF
13/20
-> increased wall thickness
-> increased indexed LA volume
-> E/e’ around 12
… supportive of HFpEF
13/20
To sum:
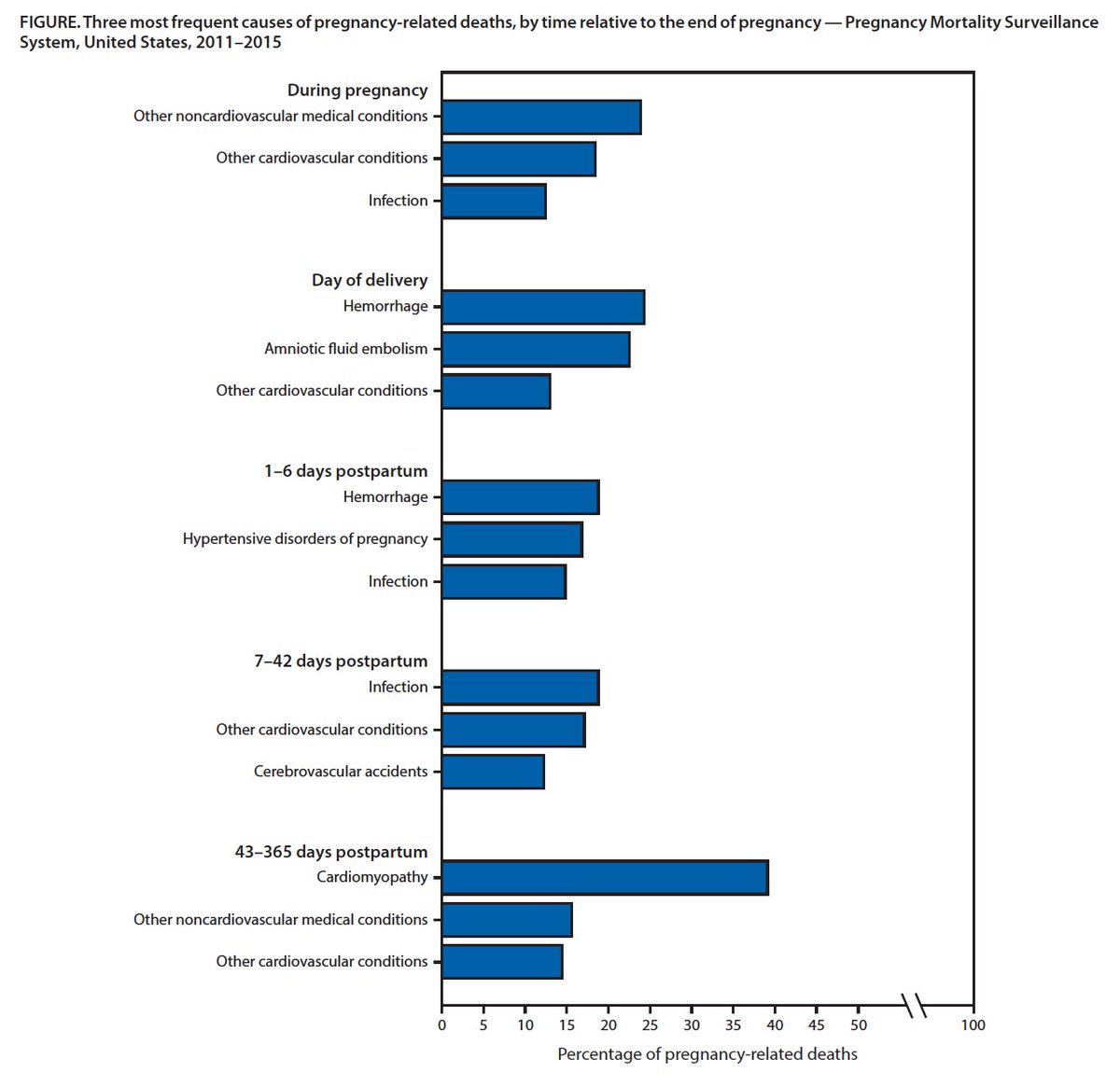
#POCUS showed that this wasn’t COVID PNA, and that this was likely cardiogenic pulmonary edema associated with her severe preeclampsia.
However, while bedside US can do a lot of things, it can’t address systemic racism.
How did that play a role here?
14/20
#POCUS showed that this wasn’t COVID PNA, and that this was likely cardiogenic pulmonary edema associated with her severe preeclampsia.
However, while bedside US can do a lot of things, it can’t address systemic racism.
How did that play a role here?
14/20
Our patient was African-American.
And preeclampsia (along with many other complications of pregnancy) is ravaging this American population.
15/20
And preeclampsia (along with many other complications of pregnancy) is ravaging this American population.
15/20
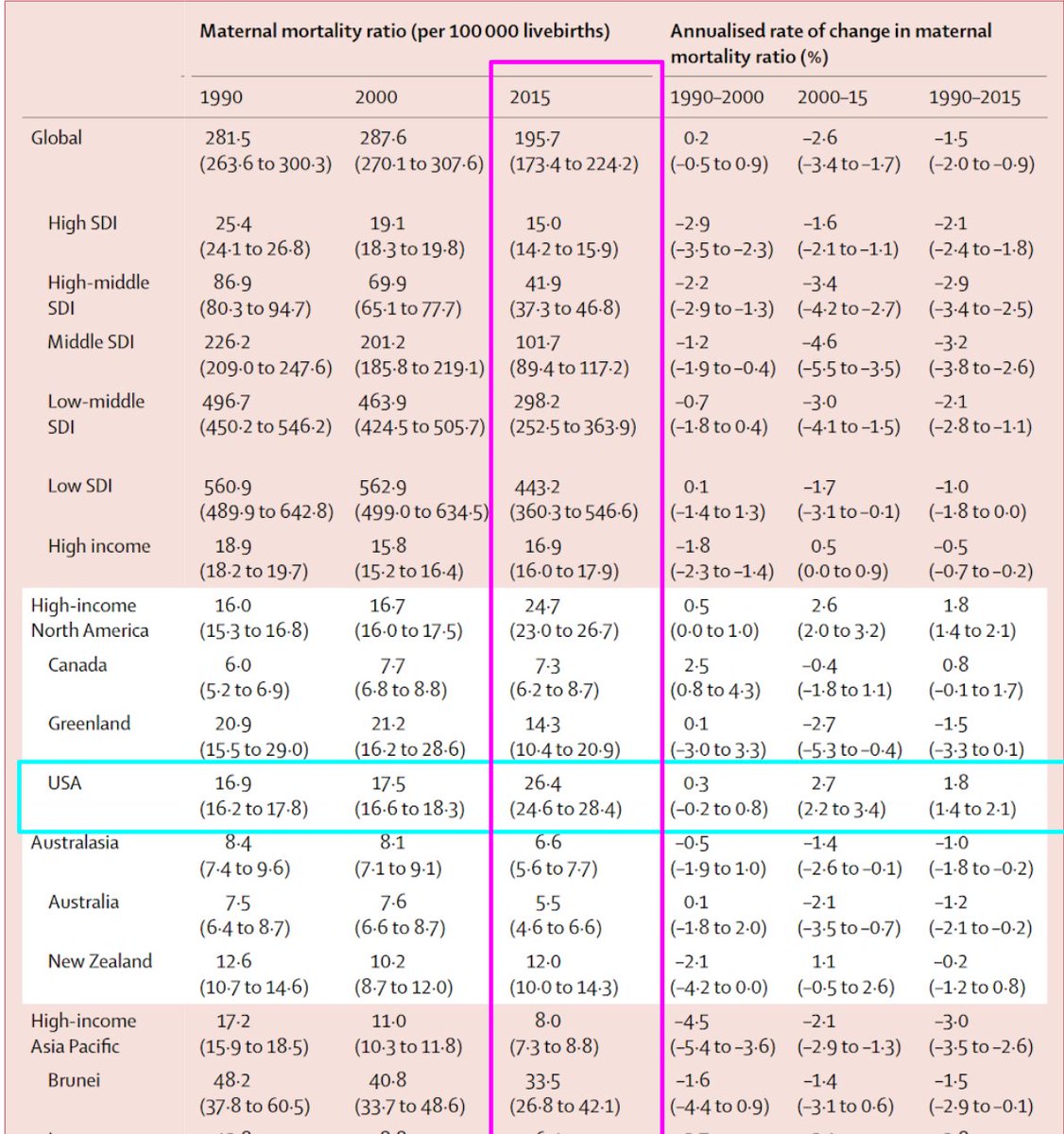
Look, maternal mortality is already horrific compared with our international peers.
E.g. our rate is 5 times higher than in Australia
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(16)31470-2/fulltext
16/20">https://www.thelancet.com/journals/...
E.g. our rate is 5 times higher than in Australia
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(16)31470-2/fulltext
16/20">https://www.thelancet.com/journals/...
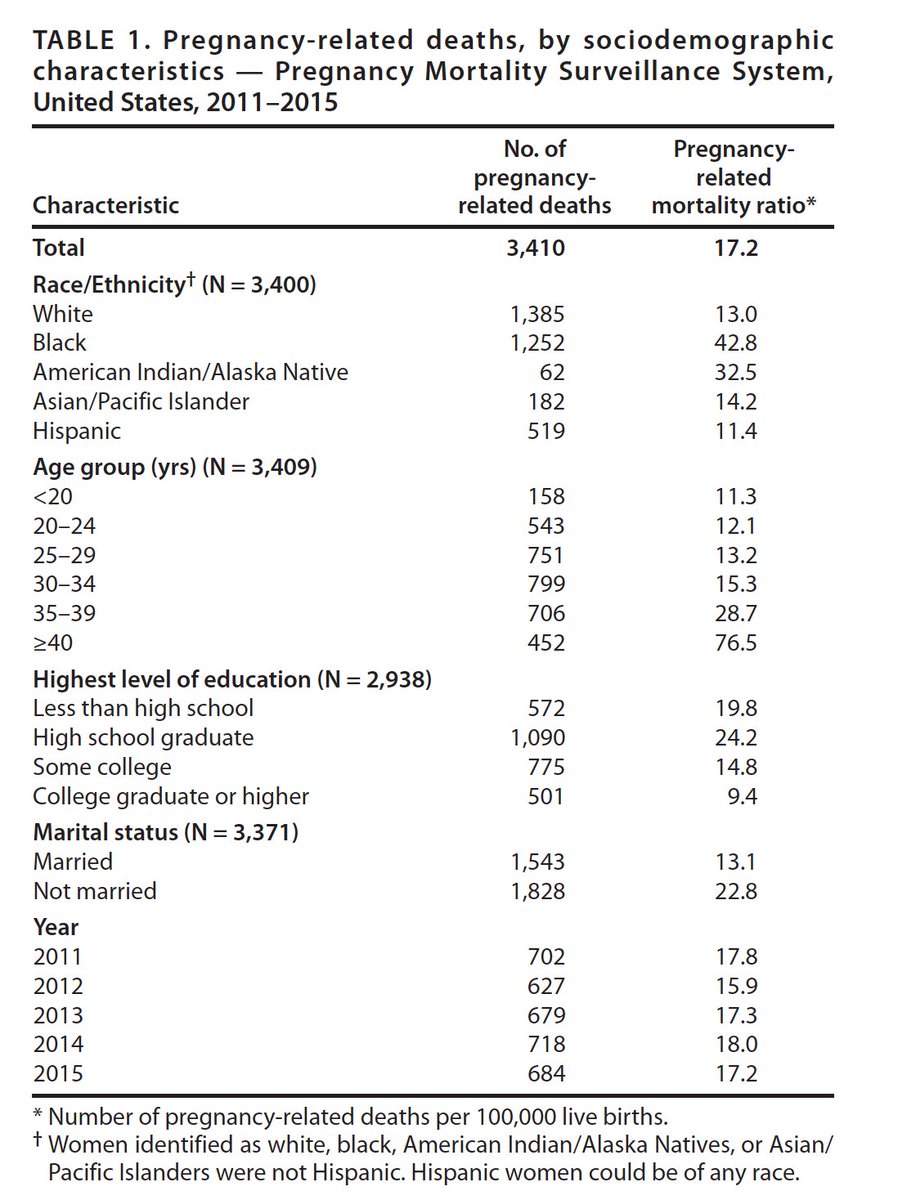
And that’s the *average* over the US population.
White women have maternal mortality rate of 13/100,000 live births (*Twice* the rate in Canada or Australia)
AA women die at a rate of 43/100,000 births
Over *3 times* as high as white women.
https://www.cdc.gov/mmwr/volumes/68/wr/mm6818e1.htm">https://www.cdc.gov/mmwr/volu...
17/20
White women have maternal mortality rate of 13/100,000 live births (*Twice* the rate in Canada or Australia)
AA women die at a rate of 43/100,000 births
Over *3 times* as high as white women.
https://www.cdc.gov/mmwr/volumes/68/wr/mm6818e1.htm">https://www.cdc.gov/mmwr/volu...
17/20
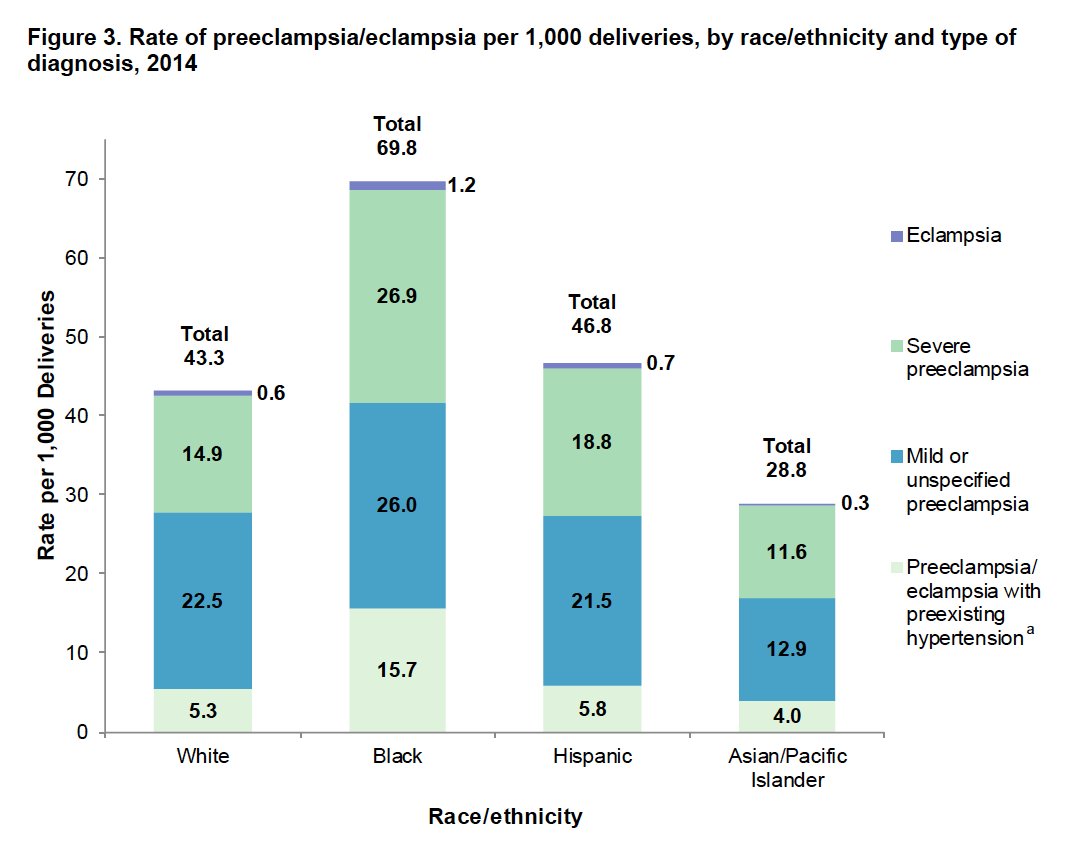
And why are African American women dying at this horrific rate?
More proximately:
-> More likely to *have* preeclampsia.
-> More likely to have *severe* preeclampsia
https://pubmed.ncbi.nlm.nih.gov/28722848/ ">https://pubmed.ncbi.nlm.nih.gov/28722848/...
18/
More proximately:
-> More likely to *have* preeclampsia.
-> More likely to have *severe* preeclampsia
https://pubmed.ncbi.nlm.nih.gov/28722848/ ">https://pubmed.ncbi.nlm.nih.gov/28722848/...
18/
So, I’d like to brag about being the clever one to use US to rule-out COVID, or how to use diastolic #POCUS in the ED to support a “rare” diagnosis...
20/20
20/20
But look at those charts above.
Until Black womens’ health is prioritized, a clever clinician with an US probe isn’t even a bandaid.
We need resources, policies, incentives, and penalties
So if you really want to treat these cases, vote.
21/20
Until Black womens’ health is prioritized, a clever clinician with an US probe isn’t even a bandaid.
We need resources, policies, incentives, and penalties
So if you really want to treat these cases, vote.
21/20

 Read on Twitter
Read on Twitter