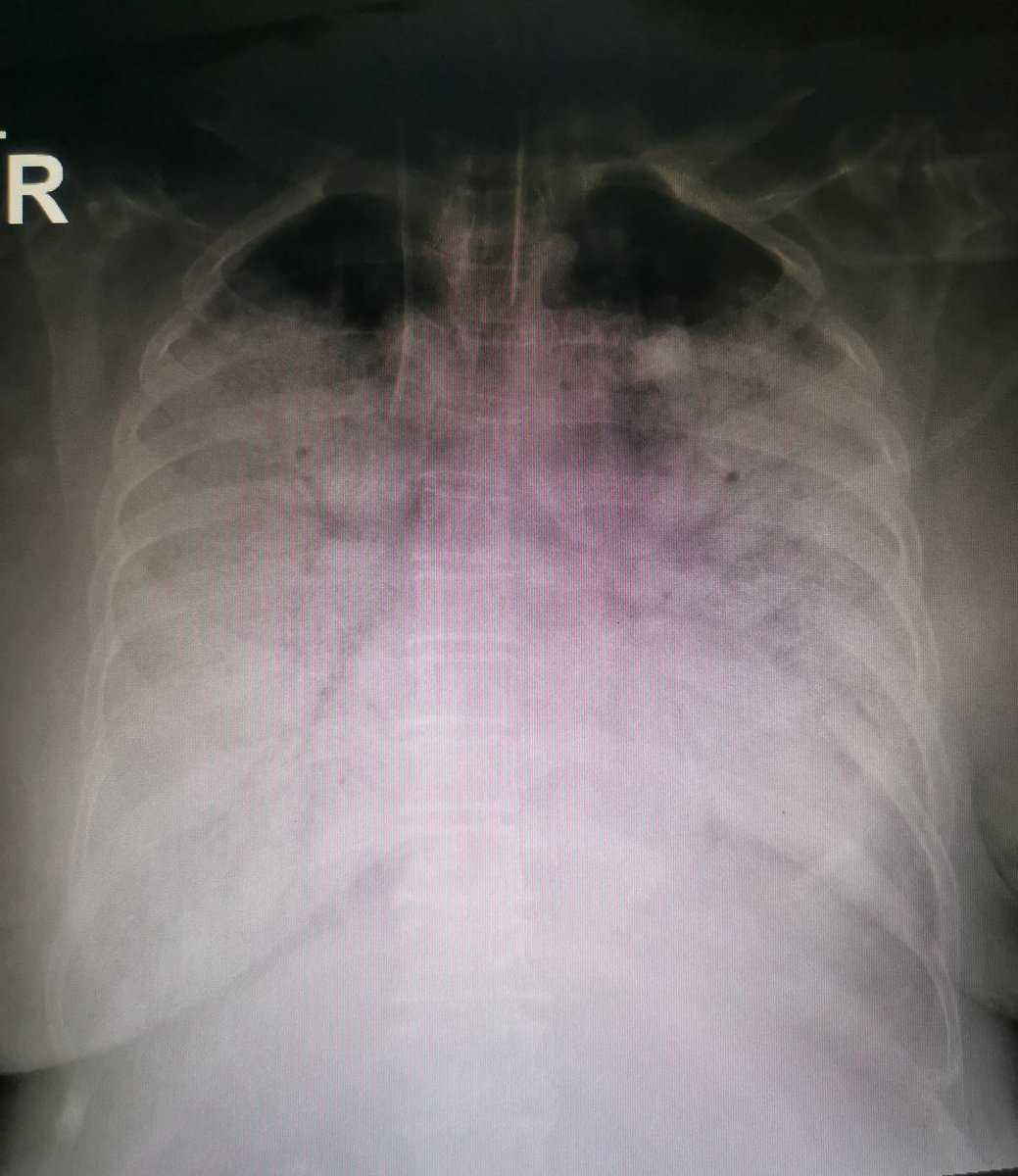
#ARDS. Approach the #ICU monster with an organized thought.
#MedTwitter #CriticalCare #ventilators #twittorial #respiratory_therapy
#COVID
#MedTwitter #CriticalCare #ventilators #twittorial #respiratory_therapy
#COVID
(1/10)
Acute respiratory distress syndrome is an impairment of alveolar-interstatium capillary-relationship + an inflammatory distruction.
Berlin definition has an objective criteria so all teams can speak a common language.
Acute respiratory distress syndrome is an impairment of alveolar-interstatium capillary-relationship + an inflammatory distruction.
Berlin definition has an objective criteria so all teams can speak a common language.
(2/10)
A protein rich inflammatory fluid will fill the airspace (so called wet lung) in a heterogeneous distribution.
A protein rich inflammatory fluid will fill the airspace (so called wet lung) in a heterogeneous distribution.
(3/10)
This will result in:
- impair gas exchange
- smaller aireated area (baby lung)
- decrease lung compliance (so called stiff lung)
- pulmonary hypertension.
This will result in:
- impair gas exchange
- smaller aireated area (baby lung)
- decrease lung compliance (so called stiff lung)
- pulmonary hypertension.
(4/10)
Management is divided into:
- ventilator management
- non- ventilator (pharmacological and non-pharmaceutical) management.
Management is divided into:
- ventilator management
- non- ventilator (pharmacological and non-pharmaceutical) management.
(5/10)
Lung protecive ventilation with halmark of low tidal volume, targeted platue pressure(<30) and using optimal PEEP.
ARDS network (ARMA) trial was the landmark fot that.
You can review choosing optimal PEEP here. https://twitter.com/Mosapositive/status/1280483859637862400?s=19">https://twitter.com/Mosaposit...
Lung protecive ventilation with halmark of low tidal volume, targeted platue pressure(<30) and using optimal PEEP.
ARDS network (ARMA) trial was the landmark fot that.
You can review choosing optimal PEEP here. https://twitter.com/Mosapositive/status/1280483859637862400?s=19">https://twitter.com/Mosaposit...
(6/10)
Non pharmacological mainly is positional management i.e prone ventilation.
Look for it there https://twitter.com/Mosapositive/status/1290709292153176066?s=19">https://twitter.com/Mosaposit...
Non pharmacological mainly is positional management i.e prone ventilation.
Look for it there https://twitter.com/Mosapositive/status/1290709292153176066?s=19">https://twitter.com/Mosaposit...
(7/10)
Pharmacological intervention include:
Nueromuscular blocking agent.
The last evidence from a large Meta-analysis of RCTs doesn& #39;t recommend routine use but in case once deep sedation is needed. (keep in mind the difference between bolus Vs infusion)
Pharmacological intervention include:
Nueromuscular blocking agent.
The last evidence from a large Meta-analysis of RCTs doesn& #39;t recommend routine use but in case once deep sedation is needed. (keep in mind the difference between bolus Vs infusion)
(8/10)
Conservative fluid management (despite volume status) is preferred although mortality benefit is not clear.
FACTT trial was the one looking for.
Conservative fluid management (despite volume status) is preferred although mortality benefit is not clear.
FACTT trial was the one looking for.
(9/10)
Steroid use is still controversial with different suggested regimen.
Steroid use is still controversial with different suggested regimen.
(10/10)
N.B:
More important is to manage the underlying cause.
Rescue therapies are beyond the aim of this thread.
The end.
N.B:
More important is to manage the underlying cause.
Rescue therapies are beyond the aim of this thread.
The end.

 Read on Twitter
Read on Twitter