Four years ago @leonscottmd asked if we could use #wearables to monitor & eventually reduce bone stress injury risks in runners. Based on our latest #biomechanics study I& #39;m more & more convinced answer is going to be: Yes!
What we figured out so far:
https://authors.elsevier.com/c/1byHRcBxf01UA
1/">https://authors.elsevier.com/c/1byHRcB...
What we figured out so far:
https://authors.elsevier.com/c/1byHRcBxf01UA
1/">https://authors.elsevier.com/c/1byHRcB...
Here& #39;s a few things to discuss...
#1 what causes overuse injuries like stress fractures?
#2 how do current wearables assess injury risk?
#3 benefits of multi-sensor algorithms
#4 epidemiological evidence from occupational health suggests this approach can work
2/
#1 what causes overuse injuries like stress fractures?
#2 how do current wearables assess injury risk?
#3 benefits of multi-sensor algorithms
#4 epidemiological evidence from occupational health suggests this approach can work
2/
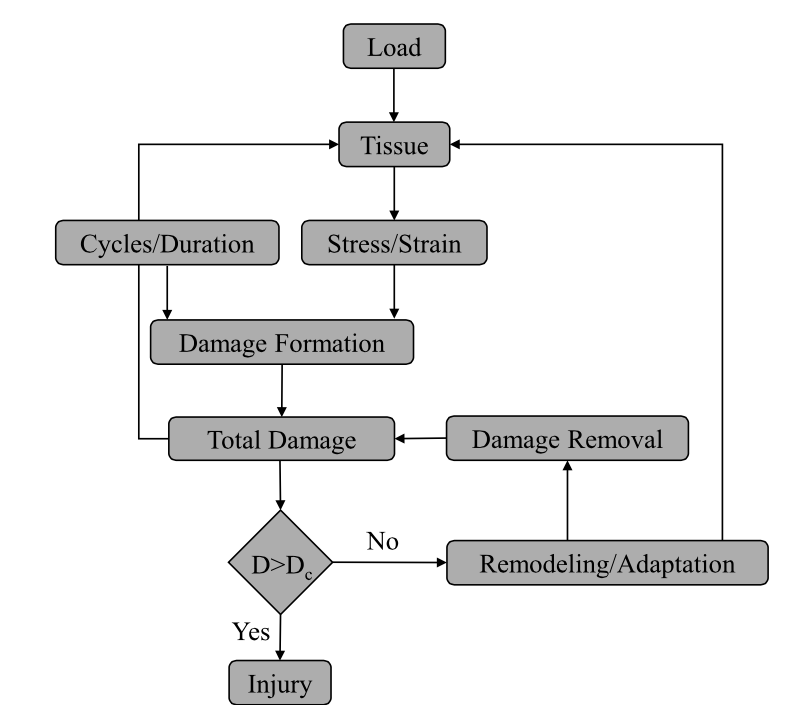
#1 What causes stress fractures (& other overuse injuries)?
Converging, multidisciplinary evidence indicates overuse injuries are consistent with a mechanical fatigue failure process, in which tissues accumulate microdamage due to repetitive loading. (Fig from Edwards 2018)
3/
Converging, multidisciplinary evidence indicates overuse injuries are consistent with a mechanical fatigue failure process, in which tissues accumulate microdamage due to repetitive loading. (Fig from Edwards 2018)
3/
When the rate of microdamage outpaces the rate at which a tissue can heal itself then you& #39;re "cruising for a bruising" (or stress fracture) as they say.
4/
4/
We expect that by developing new tools that can monitor tissue loading in daily life we can better understand overuse injury risk factors, as well as better manage/regulate tissue loading to help maximize health & performance in the future.
5/
5/
As a tangible example & first step towards this vision we explored ways to monitor tibia* (lower leg) bone loads using signals obtainable from existing types of wearable sensors.
*The tibia is a common place for bone stress injuries in runners (& military cadets & others).
6/
*The tibia is a common place for bone stress injuries in runners (& military cadets & others).
6/
#2 How do existing wearables try to assess overuse injury risks like tibial stress fractures?
Traditionally a big focus has been on monitoring how hard the foot impacts the ground in running, then equating impact or rate of loading to "wear & tear" or injury risk. However...
7/
Traditionally a big focus has been on monitoring how hard the foot impacts the ground in running, then equating impact or rate of loading to "wear & tear" or injury risk. However...
7/
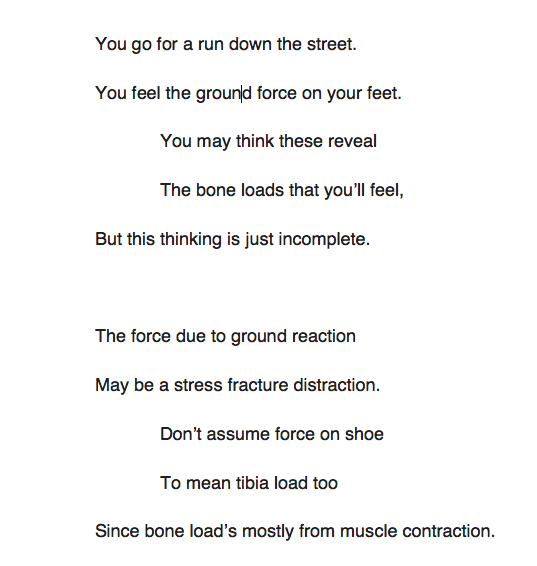
As detailed in our 2019 paper, directly inferring tibial bone load & injury risk from ground forces/impacts is invalid. It stems from a #biomechanical misconception that is best refuted by reviewing the current state of scientific evidence, & poetry!
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0210000
8/">https://journals.plos.org/plosone/a...
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0210000
8/">https://journals.plos.org/plosone/a...
Analogy:
To understand loading/damage to engine rods in your car you wouldn’t measure forces under the tires.
To monitor loading/damage to tissues in your body like the tibia you can& #39;t just rely on force under your feet (like ground impacts) or surrogates like tibial shock.
9/
To understand loading/damage to engine rods in your car you wouldn’t measure forces under the tires.
To monitor loading/damage to tissues in your body like the tibia you can& #39;t just rely on force under your feet (like ground impacts) or surrogates like tibial shock.
9/
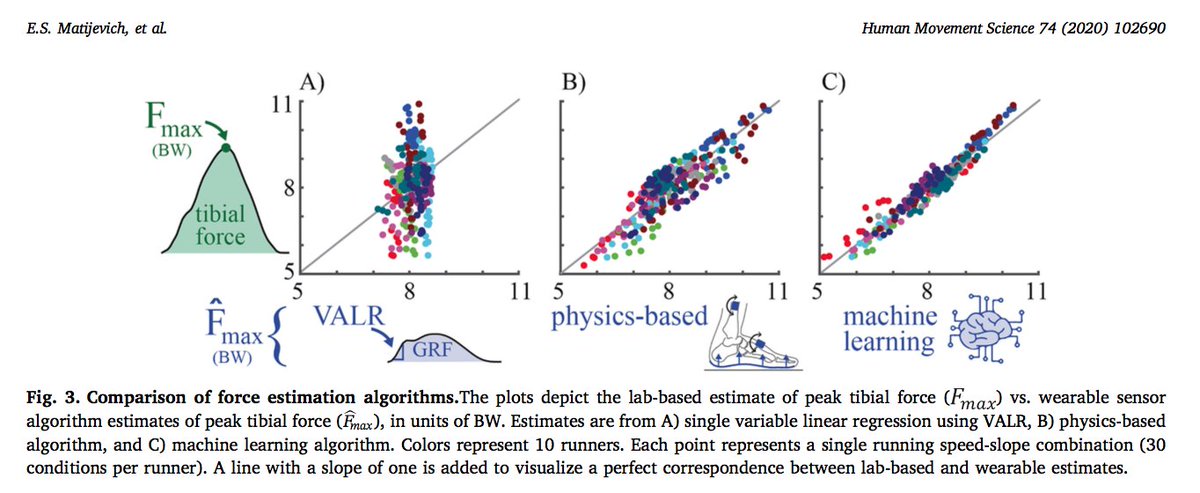
In our new paper we introduce an alternative approach aimed at monitoring tissue-level forces using non-invasive #wearable sensor signals. For this work we combined multi-sensor algorithms, machine learning & #biomechanics to improve estimates of tibial force by factor of 4.
10/
10/
I believe one of the best (and most important) things we did in this initial study was use lab-based instrumentation, and convert this data into idealized wearable sensor signals b/c it allowed us to explore a much broader combination of potential solutions.
11/
11/
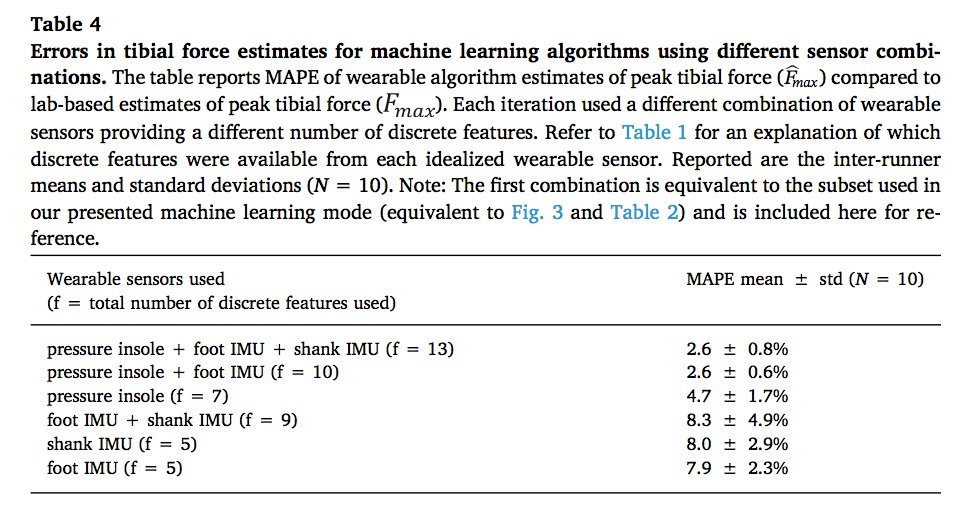
I’m excited about this interdisciplinary & exploratory approach to developing next-gen wearables. We simultaneously gain insight on minimum # of sensors, which types, where to place them, & which algorithms to use. See paper for full approach details
12/ https://authors.elsevier.com/c/1byHRcBxf01UA ">https://authors.elsevier.com/c/1byHRcB...
12/ https://authors.elsevier.com/c/1byHRcBxf01UA ">https://authors.elsevier.com/c/1byHRcB...
#3 Benefits of multi-sensor algorithms?
Accuracy of estimating bone load (& damage due to repetitive loading). B/c of the exponential relationship between tissue force & microdamage, accuracy is super important. 10% error in force can equate to 100% error in tissue damage.
13/
Accuracy of estimating bone load (& damage due to repetitive loading). B/c of the exponential relationship between tissue force & microdamage, accuracy is super important. 10% error in force can equate to 100% error in tissue damage.
13/
Some major findings from our study...
Relying on impact metrics like ground rxn force (GRF) loading rate to estimate bone load was no better (no more accurate) than just counting steps & assuming peak bone load was the same for every step (regardless of speed/slope).
14/
Relying on impact metrics like ground rxn force (GRF) loading rate to estimate bone load was no better (no more accurate) than just counting steps & assuming peak bone load was the same for every step (regardless of speed/slope).
14/
Stated again for emphasis:
If you& #39;re trying to understand tibial bone loading or overuse injuries that result from repetitive tissue loading by monitoring how hard the foot impacts the ground then this study indicates that you may be doing no better than just counting steps
15/
If you& #39;re trying to understand tibial bone loading or overuse injuries that result from repetitive tissue loading by monitoring how hard the foot impacts the ground then this study indicates that you may be doing no better than just counting steps
15/
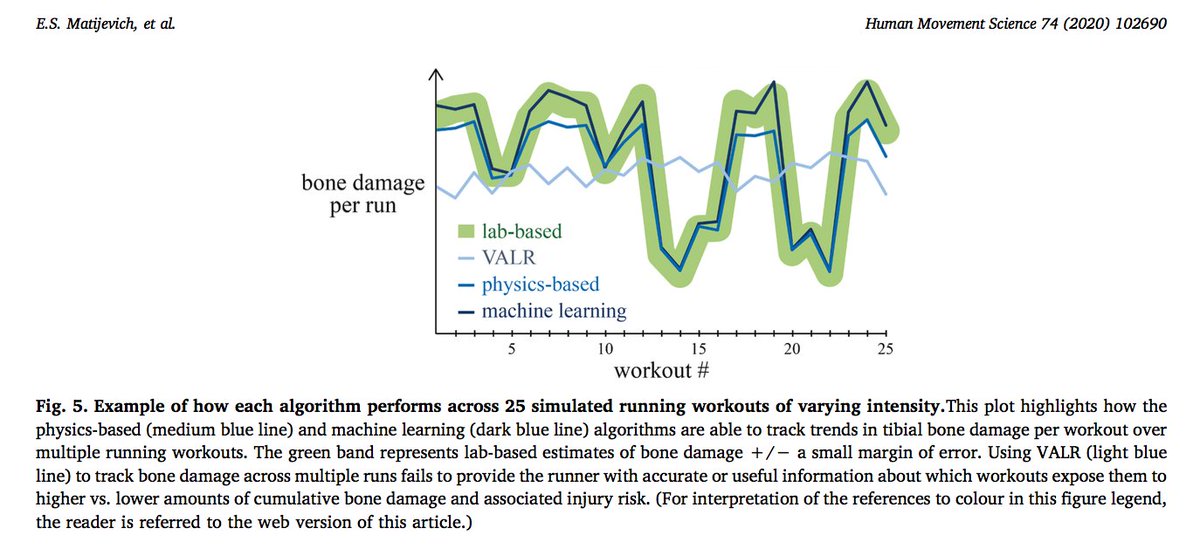
The difference between using multi-sensor algorithms vs. traditional approaches (e.g., using vertical average loading rate, VALR) was the difference btw being able to accurately track key trends in bone load/damage across workouts vs. not being able to track trends at all.
16/
16/
We also explored how well we would expect different subsets of sensors to perform. For example, comparing how accurate bone force estimates would be with only a foot IMU vs. only a pressure-sensing insole vs. using both together.
17/
17/
Using a multi-sensor algorithm that combines signals obtainable from a pressure-sensing insole & one IMU on the foot/shoe yielded average errors in peak tibial force of 2.6%. A 4-fold improvement in accuracy vs. load rate, & 2-3-fold improvement vs. single-sensor solutions.
18/
18/
So what are drawbacks? Not seeing too many at this point. Accuracy is important, & traditional impact & GRF metrics, & single sensors, etc. aren’t cutting it. They haven’t shown consistent ability to explain/predict stress fracture risks. We have to advance state of the art.
19/
19/
One concern we’ve heard is if need for two diff sensors (pressure-insole + IMU) is a problem. Short answer: No. Your cell phone has over a dozen diff sensors. Key to usability & user adoption isn’t minimizing # sensors. It’s about value added, packaging, design, cost, etc.
20/
20/
The great news: there are already wearables on the commercial market that contain a pressure-sensing insole and IMU on the foot (the most accurate sensor subset identified in this study). So the hardware exists, is mature, fairly inexpensive & already practical for daily use.
21/
21/
Our paper contains extended commentary on how we see this wearable tech evolving & translating into the real-world to influence health & performance. Learn more in paper section: “Path from new tools to scientific understanding and societal impact”
https://authors.elsevier.com/c/1byHRcBxf01UA
22/">https://authors.elsevier.com/c/1byHRcB...
https://authors.elsevier.com/c/1byHRcBxf01UA
22/">https://authors.elsevier.com/c/1byHRcB...
Ok… so another question we get it is: how do we know for sure that monitoring bone force or associated damage will be good indicator of bone stress injury risk? And how do we know the best bone load metrics, & precise accuracy needed right now? Short answer: We don’t...
23/
23/
...This would be akin to asking: Before invention of the pulse oximeter, how did they know it could be used to screen neonates for Critical Congenital Heart Disease, know precise oximetry metrics to track & what level of accuracy of these metrics was necessary? They didn& #39;t.
24/
24/
The reason we& #39;re excited about this new study & progress thus far is b/c this type of wearable would be practical for daily use & provide new capability to monitor tissue-level load & damage, which evidence indicates are central factors in etiology of bone stress injuries.
25/
25/
Stated simply: We think this new wearable tool can provide a practical, everyday way to measure what matters when it comes to understanding bone load & stress injuries. And it can be used/adapted to monitor other tissues too.
Also there’s another reason to be optimistic...
26/
Also there’s another reason to be optimistic...
26/
#4 Epidemiological evidence from occupational health suggests this approach can work
A risk assessment tool for monitoring low back disorders at work used a similar approach (estimating load & damage) and has been validated against two epidemiological injury databases.
27/
A risk assessment tool for monitoring low back disorders at work used a similar approach (estimating load & damage) and has been validated against two epidemiological injury databases.
27/
Gallagher et al. 2017 showed that this tool (linked below, it’s a risk table/calculator, not a wearable device) explained 72–95% of the deviance in low back disorders in occupational epidemiological injury databases.
http://lifft.pythonanywhere.com/en/unit/english/
28/">https://lifft.pythonanywhere.com/en/unit/e...
http://lifft.pythonanywhere.com/en/unit/english/
28/">https://lifft.pythonanywhere.com/en/unit/e...
And it achieved this success simply by monitoring back loading and estimating tissue damage. Thus this tool has demonstrated effectiveness even without additional user-specific data like age, height, weight, gender, tissue quality, medical history, etc.
29/
29/
As researchers we love as much data as possible, but this example shows that w/ ability to monitor load on injury-prone areas of body there& #39;s great potential to better understand & manage injury risk. This bodes well for commercial translation & societal impact in near-term.
30/
30/
No Limericks to end this paper, sorry :( But hope you enjoyed this #SciComm thread. Thanks for reading. Let me know what you think. We’ll keep pushing, & continuing to make strides to further this science & to translate this #wearable #biomechanics tech outside the lab.
31/
31/
Thanks to my fantastic & interdisciplinary collaborators:
@EmilyMatijevich - lead author, biomechanist & wearables extraordinaire
@volgy - data scientist & machine learning guru
@leonscottmd - ortho & sports medicine doc
Kendall Derry - engineering undergrad & track star
32/
@EmilyMatijevich - lead author, biomechanist & wearables extraordinaire
@volgy - data scientist & machine learning guru
@leonscottmd - ortho & sports medicine doc
Kendall Derry - engineering undergrad & track star
32/
PS. @EmilyMatijevich is a remarkable #biomechanical engineer w/ expertise in motion capture, #wearables, & biosignal analysis. She defends her PhD in Dec. If your organization is looking to hire a rockstar then look no further. Find her before she’s gone. @WomenSportsTech
33/33
33/33
@threadreaderapp unroll

 Read on Twitter
Read on Twitter