PALS now recommends 1 ventilation every 2-3 sec, a drastic change from prior guidelines. This was based on a single paper of 47 pts. where 74% of cases had an initial presenting rhythm of Bradycardia w/poor perfusion. The 8 asystolic pts all died.  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤔" title="Denkendes Gesicht" aria-label="Emoji: Denkendes Gesicht"> https://www.dropbox.com/s/691nebgeu3w72pf/PIHCA%20and%20Ventilation%20Rates%202019.pdf?dl=0">https://www.dropbox.com/s/691nebg...
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤔" title="Denkendes Gesicht" aria-label="Emoji: Denkendes Gesicht"> https://www.dropbox.com/s/691nebgeu3w72pf/PIHCA%20and%20Ventilation%20Rates%202019.pdf?dl=0">https://www.dropbox.com/s/691nebg...
Furthermore, 60% of the patients in the cohort had congenital heart disease as a pre-existing condition.
Compare this to the Banerjee paper in Resuscitation which showed dramatic improvement in POHCA outcomes with a strategy of 1 breath every 10 seconds (6 bpm). This landmark study must be considered in this critical discussion. Lives depend on it. https://www.dropbox.com/s/sspze82jk6mbff5/Banerjee%20Pepe%20Resuscitation%202019.pdf?dl=0">https://www.dropbox.com/s/sspze82...
If you can’t tell, I’m losing sleep over this.
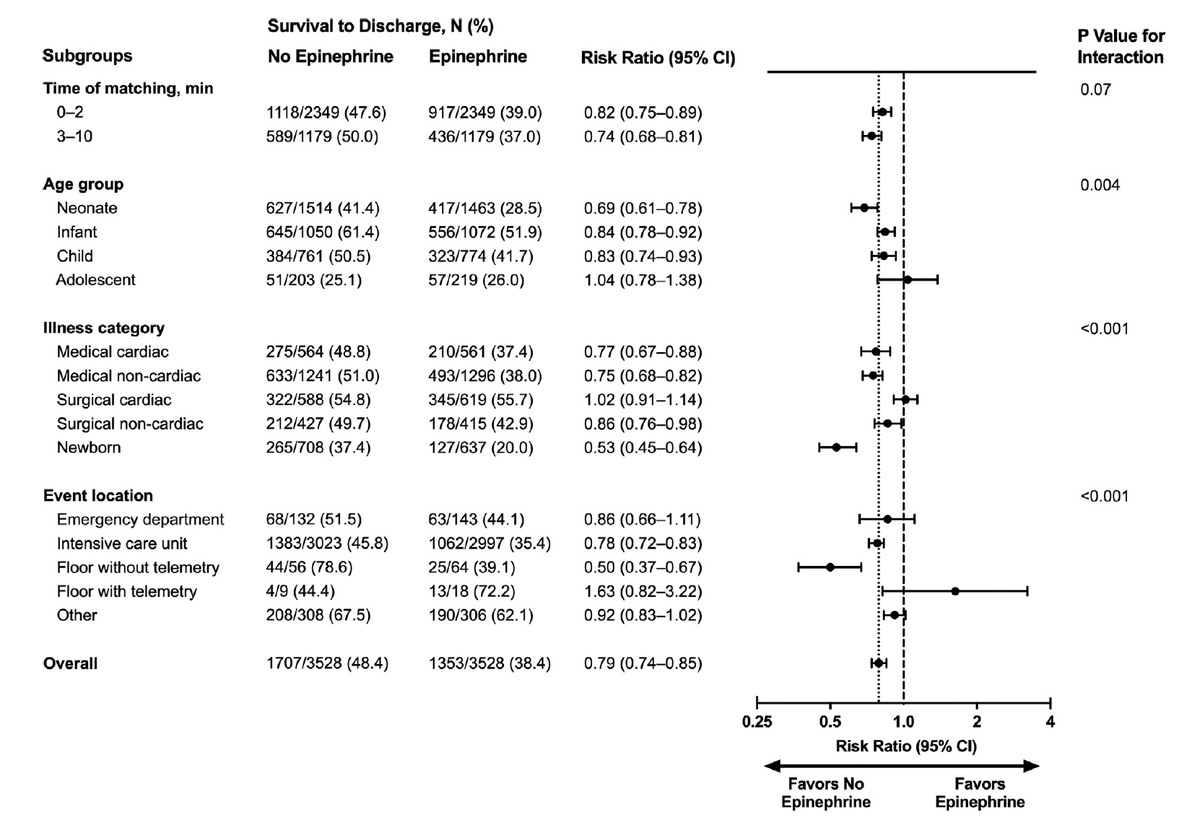
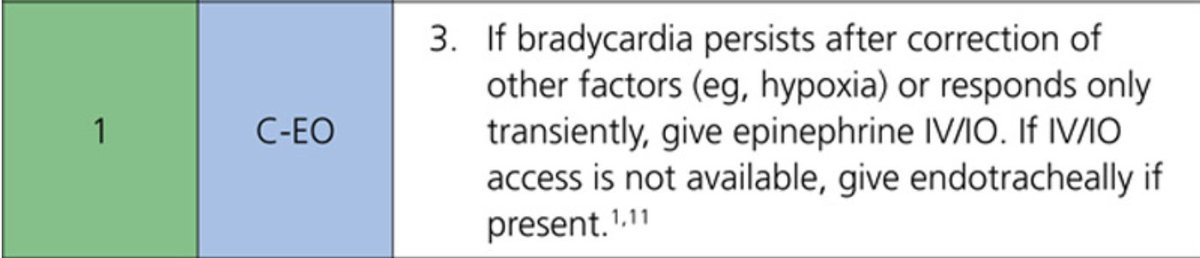
The 2020 PALS Guidlelines also maintained its stance regarding the use of Epinephrine (0.1 mg/mL) for symptomatic bradycardia. This in the face of a convincing paper in Resuscitation (March 2020) that came to the opposite conclusion.
Follow the thread https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">
Follow the thread
Reference #11 above is a paper by Holmberg et. al ( https://bit.ly/3orQiqI )">https://bit.ly/3orQiqI&q... which came to the following conclusion: "..We found that epinephrine was associated with worse outcomes in children receiving cardiopulmonary resuscitation for bradycardia with poor perfusion.."
Last year I modified my protocols, removing cardiac arrest epinephrine from the symptomatic bradycardia procotol and replaced it with push pressor epinephrine. I am a firm believer that epinephrine at a dose of 0.01 mg/kg should not be given to anyone with a perfusing rhythm.
This data is not applicable to the majority of patients we resuscitate in the field (a majority of which are asystolic), and therefore my protocols will not adjust to this new recommendation. More to come.

 Read on Twitter
Read on Twitter https://www.dropbox.com/s/691nebg..." title="PALS now recommends 1 ventilation every 2-3 sec, a drastic change from prior guidelines. This was based on a single paper of 47 pts. where 74% of cases had an initial presenting rhythm of Bradycardia w/poor perfusion. The 8 asystolic pts all died. https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤔" title="Denkendes Gesicht" aria-label="Emoji: Denkendes Gesicht"> https://www.dropbox.com/s/691nebg..." class="img-responsive" style="max-width:100%;"/>
https://www.dropbox.com/s/691nebg..." title="PALS now recommends 1 ventilation every 2-3 sec, a drastic change from prior guidelines. This was based on a single paper of 47 pts. where 74% of cases had an initial presenting rhythm of Bradycardia w/poor perfusion. The 8 asystolic pts all died. https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤔" title="Denkendes Gesicht" aria-label="Emoji: Denkendes Gesicht"> https://www.dropbox.com/s/691nebg..." class="img-responsive" style="max-width:100%;"/>

 " title="The 2020 PALS Guidlelines also maintained its stance regarding the use of Epinephrine (0.1 mg/mL) for symptomatic bradycardia. This in the face of a convincing paper in Resuscitation (March 2020) that came to the opposite conclusion.Follow the thread https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">" class="img-responsive" style="max-width:100%;"/>
" title="The 2020 PALS Guidlelines also maintained its stance regarding the use of Epinephrine (0.1 mg/mL) for symptomatic bradycardia. This in the face of a convincing paper in Resuscitation (March 2020) that came to the opposite conclusion.Follow the thread https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">" class="img-responsive" style="max-width:100%;"/>