In case you want to scroll instead of listen to my voice... a thread of our findings! "Invasive aureus infections in persons with and without drug use:
one-year comparative outcomes" #IDWeek2020 https://twitter.com/ABeieler/status/1319280919111294982">https://twitter.com/ABeieler/...
one-year comparative outcomes" #IDWeek2020 https://twitter.com/ABeieler/status/1319280919111294982">https://twitter.com/ABeieler/...
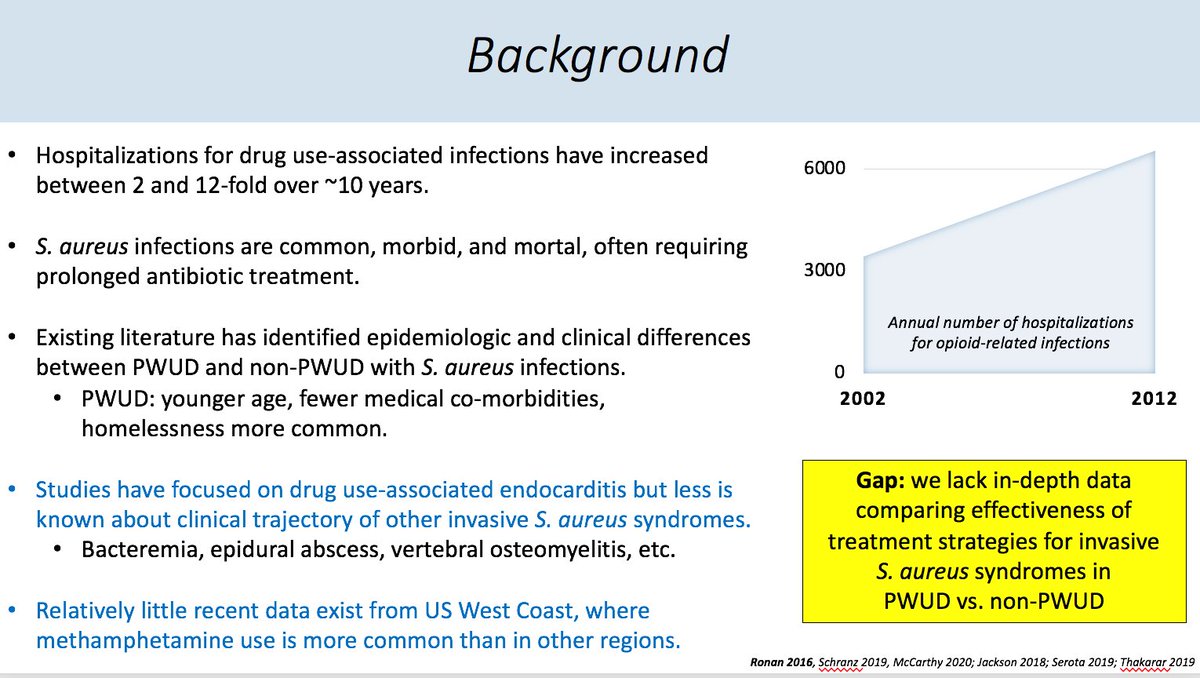
Why do this study? Many have described skyrocketing # of bacterial infxns related to drug use. ID recs for S. aureus tend to be protocol-driven with quality focus… but with #SIRIs representing more of the infxns we see, just how high quality/effective IS our treatment of #PWUD?
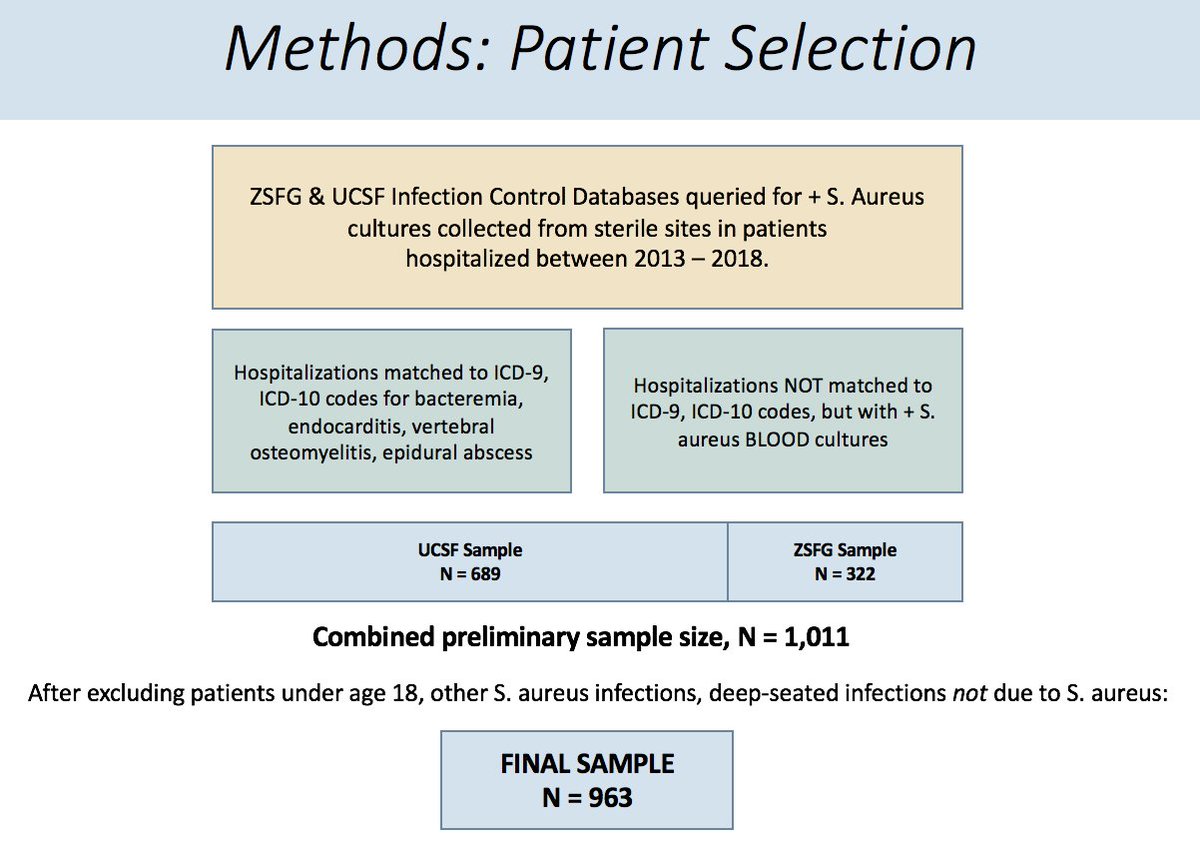
This was a retrospective cohort study of all pts hospitalized with S. aureus bacteremia, endocarditis, vertebral osteomyelitis, or epidural abscess at UCSF and SFGH between 2013 – 2018, comparing outcomes in PWUD vs. non-PWUD.
*Sidenote: why PWUD instead of focus on injection drug use? Opioids and meth affect immune system + not all infections are related to injection (e.g. skin picking)! We need to understand pathophys of drug-related infxn better… ahem, @lauramarks are you studying this?
PWUD with S. aureus infections were younger, generally healthier (though higher proportion w/HIV), and many more experiencing homelessness – as others studying endocarditis have found.
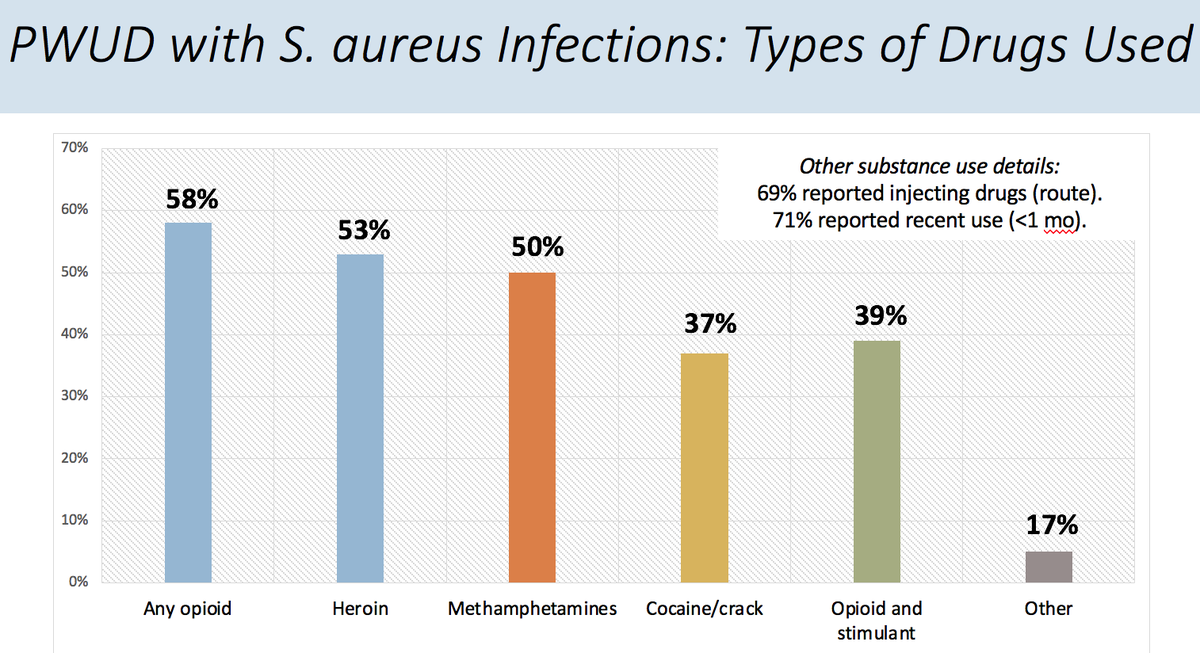
In our sample of people with S. aureus infections in San Francisco, opioid use was most common (58%), but closely followed by methamphetamine use (50%!!) Both opioid and stimulant use was also very common (39%).
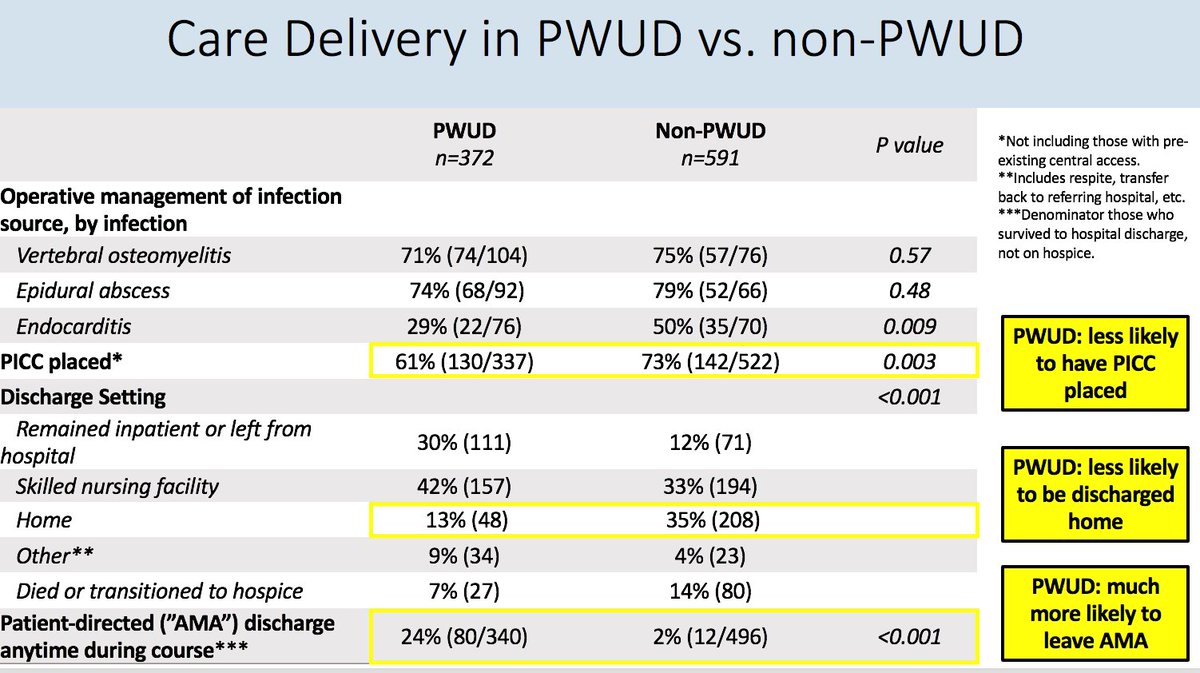
There was no difference in planned duration of antibiotic treatment, but care delivery differed in a number of different ways: fewer surgeries in PWUD w/endocarditis, fewer PICC lines and fewer discharges home, and many more pt-directed discharges in PWUD.
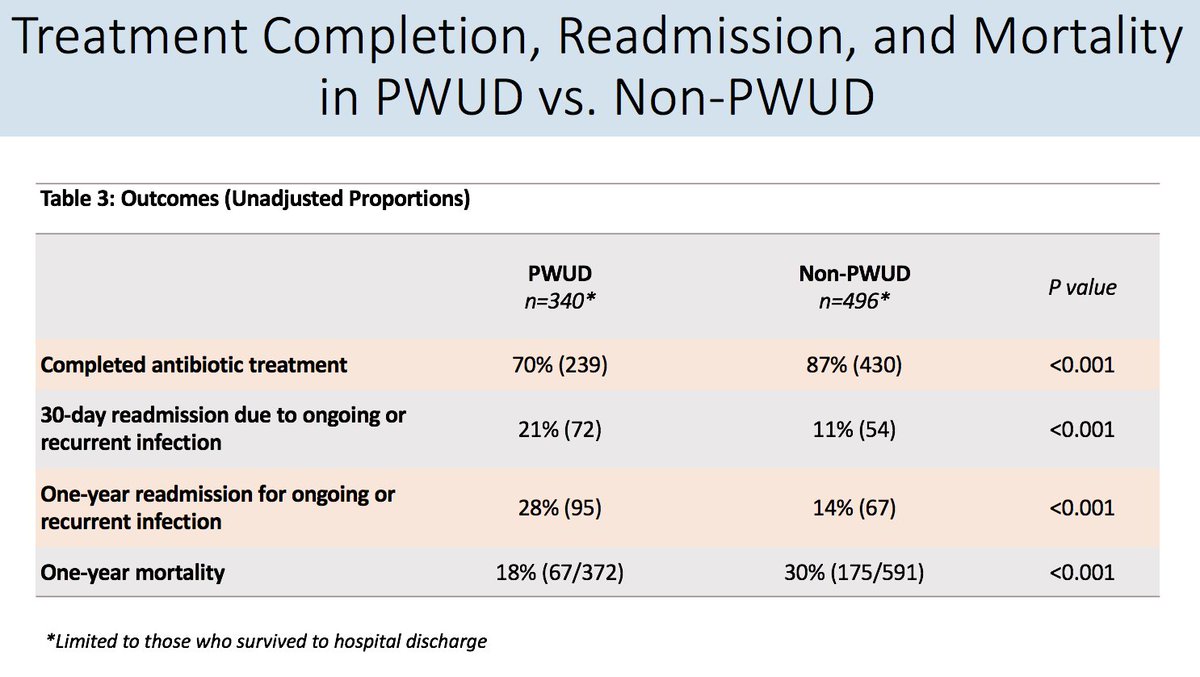
Unadjusted outcomes! 70% of antibiotic treatment courses were not completed among PWUD compared to ~90% among non-PWUD, and one-year readmission rates were 28% vs. 14% -- though with mortality much higher among our sample of non-PWUD (30%) vs. PWUD (18%).
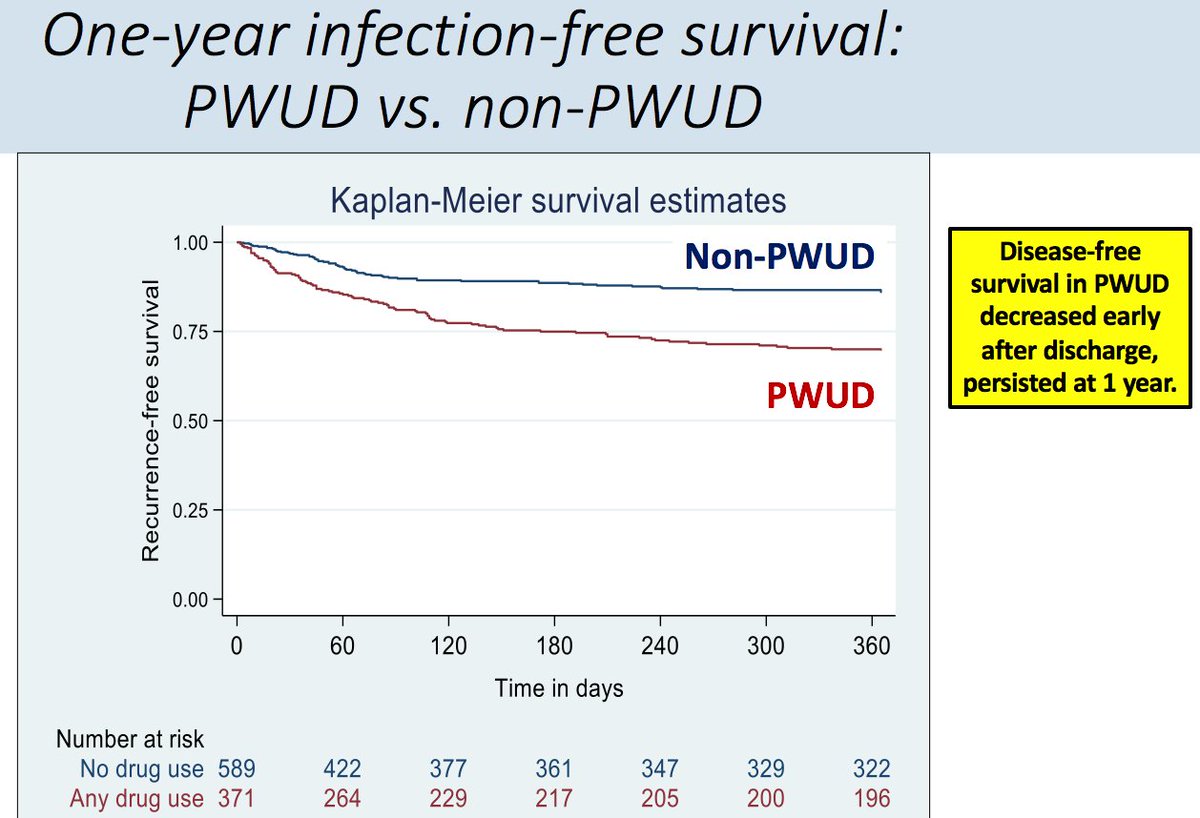
Kaplan Meier time! Better way to look at this outcome is time-to-event analysis, and as you can see, disease-free survival decreased early post-discharge and persisted x 1 year.
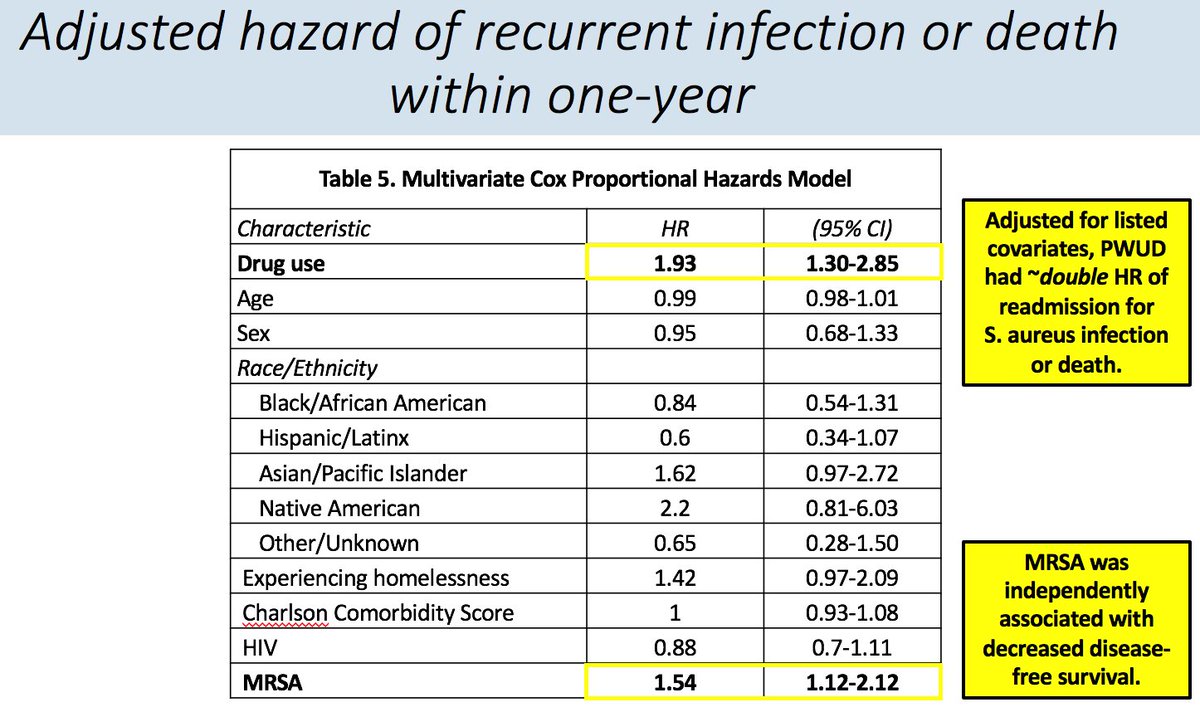
Are you still with me? Last piece data: in adjusted Cox model, drug use was associated with 2x hazard of readmit for infection or death, while we didn’t find age, race-ethnicity, comorbid illness independently associated. #MRSA WAS independently associated with readmit/death.
We are typically offering similar IV abx recs for PWUD and non-PWUD with S. aureus infxns, but there is not parity in care delivery nor outcomes, with diminished disease-free survival! We need more pt-centered antibiotic options + SUD tx models, esp for stimulants! The end.
Good thing there are so many smarties arnd the country doing this work, including folks on our team involved in this work: @VivekJainMD @pcoffin @StephenieLe11 @MarleneMartinMD @UCSF_HIVIDGM @UCSF_ID

 Read on Twitter
Read on Twitter