1/ TELEHEALTH: THE IRRESISTIBLE FORCE MEETS THE IMMOVABLE OBJECT
The IRRESISTIBLE FORCE is patients& #39; rapid uptake & high satisfaction with #telehealth & virtual care.
The IMMOVABLE OBJECT is healthcare incumbents& #39; economic interests that align with the pre COVID-19 old normal.
The IRRESISTIBLE FORCE is patients& #39; rapid uptake & high satisfaction with #telehealth & virtual care.
The IMMOVABLE OBJECT is healthcare incumbents& #39; economic interests that align with the pre COVID-19 old normal.
2/ TELEHEALTH: THE IRRESISTIBLE FORCE MEETS THE IMMOVABLE OBJECT
This thread will be of interest to people who follow a range of hashtags:
#telemedicine
#TelemedNow
#telehealth
#DigitalHealth
#HealthIT
#VirtualCare
#VirtualHealth
#SDOH
#mHealth
#IoT
#ConnectedHealth
This thread will be of interest to people who follow a range of hashtags:
#telemedicine
#TelemedNow
#telehealth
#DigitalHealth
#HealthIT
#VirtualCare
#VirtualHealth
#SDOH
#mHealth
#IoT
#ConnectedHealth
3/ PART ONE: Telehealth as the IRRESISTIBLE FORCE:
A. Rapid Uptake
B. High Satisfaction
C. Strong Intentions for Future Use
D. Quality
E. Patient Safety
F. Additional Benefits
G. Glowing Reports
A. Rapid Uptake
B. High Satisfaction
C. Strong Intentions for Future Use
D. Quality
E. Patient Safety
F. Additional Benefits
G. Glowing Reports
4/
A. Rapid Uptake
Providers reported "50x to 175x the number of telehealth visits compared with pre COVID-19 levels"
— @AdvisoryBd https://www.advisory.com/research/health-care-advisory-board/blogs/at-the-helm/2020/06/10-covid-19-takeaways-june-11
Respondents">https://www.advisory.com/research/... who have had a virtual visit
2019--8%
2020--22%
— 2020 @Amwell Survey https://business.amwell.com/resources/from-virtual-care-to-hybrid-care-covid-19-and-the-future-of-healthcare/">https://business.amwell.com/resources...
A. Rapid Uptake
Providers reported "50x to 175x the number of telehealth visits compared with pre COVID-19 levels"
— @AdvisoryBd https://www.advisory.com/research/health-care-advisory-board/blogs/at-the-helm/2020/06/10-covid-19-takeaways-june-11
Respondents">https://www.advisory.com/research/... who have had a virtual visit
2019--8%
2020--22%
— 2020 @Amwell Survey https://business.amwell.com/resources/from-virtual-care-to-hybrid-care-covid-19-and-the-future-of-healthcare/">https://business.amwell.com/resources...
5/
Telehealth visits surged, then settled at 11%
— @StrataDecision, September 2020 https://www.stratadecision.com/wp-content/uploads/2020/09/6-Month-Summary_National-Patient-and-Procedure-Volume-Tracker-and-Report_FINAL.pdf">https://www.stratadecision.com/wp-conten...
Telehealth visits surged, then settled at 11%
— @StrataDecision, September 2020 https://www.stratadecision.com/wp-content/uploads/2020/09/6-Month-Summary_National-Patient-and-Procedure-Volume-Tracker-and-Report_FINAL.pdf">https://www.stratadecision.com/wp-conten...
6/
B. High Satisfaction
92% Satisfied, 62% Very Satisfied
— @POStrategies https://pos.org/wp-content/uploads/2020/05/Coronavirus-Public-Opinion-Data_Special-Provider-Report.pdf
The">https://pos.org/wp-conten... telehealth satisfaction score was 860 (out of 1000), among the highest for healthcare, insurance & financial services
— @JDPower https://www.jdpower.com/business/press-releases/2020-us-telehealth-satisfaction-study">https://www.jdpower.com/business/...
B. High Satisfaction
92% Satisfied, 62% Very Satisfied
— @POStrategies https://pos.org/wp-content/uploads/2020/05/Coronavirus-Public-Opinion-Data_Special-Provider-Report.pdf
The">https://pos.org/wp-conten... telehealth satisfaction score was 860 (out of 1000), among the highest for healthcare, insurance & financial services
— @JDPower https://www.jdpower.com/business/press-releases/2020-us-telehealth-satisfaction-study">https://www.jdpower.com/business/...
7/
@PressGaney analysis--30K patient surveys:
When 3 key drivers were in place
1) Video visit staff worked together to care for you
2) Ease of talking w/ care provider over video
3) Video connection during visit
LIKELIHOOD TO RECOMMEND video visits = 96.3%
NOT a typo — 96.3%
@PressGaney analysis--30K patient surveys:
When 3 key drivers were in place
1) Video visit staff worked together to care for you
2) Ease of talking w/ care provider over video
3) Video connection during visit
LIKELIHOOD TO RECOMMEND video visits = 96.3%
NOT a typo — 96.3%
8/
C. Strong Intentions for Future Use
A Metova study showed dramatically higher preferences for virtual care:
81% would choose telemedicine for their next consultation if given the option https://www.prnewswire.com/news-releases/new-survey-reveals-high-demand-for-telemedicine-301115288.html">https://www.prnewswire.com/news-rele...
C. Strong Intentions for Future Use
A Metova study showed dramatically higher preferences for virtual care:
81% would choose telemedicine for their next consultation if given the option https://www.prnewswire.com/news-releases/new-survey-reveals-high-demand-for-telemedicine-301115288.html">https://www.prnewswire.com/news-rele...
9/
D. Quality
Almost two-thirds of patients feel telemedicine is better than in-person visits for the same type of medical appointments (only 13% think it is worse) https://www.prnewswire.com/news-releases/new-survey-reveals-high-demand-for-telemedicine-301115288.html
In">https://www.prnewswire.com/news-rele... August 2020, @AHRQ reviewed quality & safety of telediagnosis https://www.ahrq.gov/patient-safety/reports/issue-briefs/teledx.html">https://www.ahrq.gov/patient-s...
D. Quality
Almost two-thirds of patients feel telemedicine is better than in-person visits for the same type of medical appointments (only 13% think it is worse) https://www.prnewswire.com/news-releases/new-survey-reveals-high-demand-for-telemedicine-301115288.html
In">https://www.prnewswire.com/news-rele... August 2020, @AHRQ reviewed quality & safety of telediagnosis https://www.ahrq.gov/patient-safety/reports/issue-briefs/teledx.html">https://www.ahrq.gov/patient-s...
10/
AHRQ& #39;s conclusion:
"The evidence-base for telehealth is strong, especially for the remote management of chronic health conditions. Systematic reviews confirm that telehealth improves health outcomes, utilization, and cost of care for a host of chronic diseases..."
AHRQ& #39;s conclusion:
"The evidence-base for telehealth is strong, especially for the remote management of chronic health conditions. Systematic reviews confirm that telehealth improves health outcomes, utilization, and cost of care for a host of chronic diseases..."
11/
E. Patient Safety
Many patients have been hesitant to return to provider locations:
Have you postponed any doctor appointments...?
Yes 68%
No 32%
Preferred method for the rest of the year--
In person 50%
Virtual 38%
Unsure 12%
CaringAdvisor https://caringadvisor.com/the-digital-doctor/">https://caringadvisor.com/the-digit...
E. Patient Safety
Many patients have been hesitant to return to provider locations:
Have you postponed any doctor appointments...?
Yes 68%
No 32%
Preferred method for the rest of the year--
In person 50%
Virtual 38%
Unsure 12%
CaringAdvisor https://caringadvisor.com/the-digital-doctor/">https://caringadvisor.com/the-digit...
12/
F. Additional Benefits
The Taskforce on Telehealth Policy is a joint project of @AmericanTelemed @NCQA & @ConnectwCare https://www.ncqa.org/programs/data-and-information-technology/telehealth/taskforce-on-telehealth-policy/taskforce-on-telehealth-policy-ttp-findings-and-recommendations/
Findings">https://www.ncqa.org/programs/... in the 9/20 report:
"...telehealth largely substituted for in-person care & did not increase the total number of visits.
F. Additional Benefits
The Taskforce on Telehealth Policy is a joint project of @AmericanTelemed @NCQA & @ConnectwCare https://www.ncqa.org/programs/data-and-information-technology/telehealth/taskforce-on-telehealth-policy/taskforce-on-telehealth-policy-ttp-findings-and-recommendations/
Findings">https://www.ncqa.org/programs/... in the 9/20 report:
"...telehealth largely substituted for in-person care & did not increase the total number of visits.
13/
"...telehealth can help reduce more costly urgent & ED care, as well as use of costly & often overused services such as imaging.
"Health systems & clinician practices consistently
report lower no-show rates with telehealth"
Telehealth lowered SNF transfers to hospitals.
"...telehealth can help reduce more costly urgent & ED care, as well as use of costly & often overused services such as imaging.
"Health systems & clinician practices consistently
report lower no-show rates with telehealth"
Telehealth lowered SNF transfers to hospitals.
14/
G. Glowing Reports
"Consumers who have used telehealth LOVE it"
— @POStrategies https://pos.org/wp-content/uploads/2020/07/Provider-Trends-July-2020.pdf
89%">https://pos.org/wp-conten... say COVID-19 made telehealth “an indispensable part of the healthcare system”
—Harris Poll https://www.hfma.org/topics/news/2020/07/consumers-expect-expanded-telehealth-to-remain-post-covid-19--su.html">https://www.hfma.org/topics/ne...
G. Glowing Reports
"Consumers who have used telehealth LOVE it"
— @POStrategies https://pos.org/wp-content/uploads/2020/07/Provider-Trends-July-2020.pdf
89%">https://pos.org/wp-conten... say COVID-19 made telehealth “an indispensable part of the healthcare system”
—Harris Poll https://www.hfma.org/topics/news/2020/07/consumers-expect-expanded-telehealth-to-remain-post-covid-19--su.html">https://www.hfma.org/topics/ne...
15/ THE IMMOVABLE OBJECT—healthcare incumbents& #39; economic interests that better align with the pre COVID-19 old normal:
* Payer fears about utilization & costs
* Provider uncertainty over future reimbursement
* Provider concerns about new competition
* Regulatory quagmire
* Payer fears about utilization & costs
* Provider uncertainty over future reimbursement
* Provider concerns about new competition
* Regulatory quagmire
16/
A. Payer fears that telehealth increases utilization & costs
A central question:
Are telehealth visits SUBSTITUTIVE or ADDITIVE to in-person office visits?
A. Payer fears that telehealth increases utilization & costs
A central question:
Are telehealth visits SUBSTITUTIVE or ADDITIVE to in-person office visits?
17/
“The very advantage of telehealth — the fact that it makes care more convenient — is also its Achilles’ heel, in the sense that it can make care too convenient”
-- @Ateevm, Harvard Medical School
“The very advantage of telehealth — the fact that it makes care more convenient — is also its Achilles’ heel, in the sense that it can make care too convenient”
-- @Ateevm, Harvard Medical School
18/
The Congressional Budget Office rationale for restricting Medicare telehealth is that it increases—rather than decreases—health care costs, mostly through additional utilization. https://leavittpartners.com/future-medicare-telehealth-coverage-cbo-hesitates-congress-inches-forward/">https://leavittpartners.com/future-me...
The Congressional Budget Office rationale for restricting Medicare telehealth is that it increases—rather than decreases—health care costs, mostly through additional utilization. https://leavittpartners.com/future-medicare-telehealth-coverage-cbo-hesitates-congress-inches-forward/">https://leavittpartners.com/future-me...
19/
The evidence is "unclear".
A 2018 @Health_Affairs article examined 20 systematic reviews https://www.ehidc.org/sites/default/files/resources/files/The%20current%20state%20of%20telehealth%20evidence.pdf
"...it">https://www.ehidc.org/sites/def... is unclear whether the use of telehealth services reduces the use of other services, duplicates services, or improves access to beneficial services."
The evidence is "unclear".
A 2018 @Health_Affairs article examined 20 systematic reviews https://www.ehidc.org/sites/default/files/resources/files/The%20current%20state%20of%20telehealth%20evidence.pdf
"...it">https://www.ehidc.org/sites/def... is unclear whether the use of telehealth services reduces the use of other services, duplicates services, or improves access to beneficial services."
20/
Some studies have found increases in utilization, e.g.,:
"We estimated that 12% of direct-to-consumer telehealth visits [for respiratory care] replaced visits to other providers, and 88% represented new utilization."
-- @Health_Affairs https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2016.1130">https://www.healthaffairs.org/doi/full/...
Some studies have found increases in utilization, e.g.,:
"We estimated that 12% of direct-to-consumer telehealth visits [for respiratory care] replaced visits to other providers, and 88% represented new utilization."
-- @Health_Affairs https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2016.1130">https://www.healthaffairs.org/doi/full/...
21/
Some studies have shown substitution, e.g.,:
One study found that that among patients who had contemplated an ER visit, 74% had their concerns resolved with a telemedicine visit. | American Journal of Emergency Medicine https://www.sciencedirect.com/science/article/abs/pii/S0735675718306533">https://www.sciencedirect.com/science/a...
Some studies have shown substitution, e.g.,:
One study found that that among patients who had contemplated an ER visit, 74% had their concerns resolved with a telemedicine visit. | American Journal of Emergency Medicine https://www.sciencedirect.com/science/article/abs/pii/S0735675718306533">https://www.sciencedirect.com/science/a...
22/
B. Provider uncertainty over future reimbursement
When asked about barriers to telehealth adoption, 64% of physicians cited "Uncertainty Around Reimbursement"
2020 Amwell Physician and Consumer Survey https://business.amwell.com/resources/from-virtual-care-to-hybrid-care-covid-19-and-the-future-of-healthcare/">https://business.amwell.com/resources...
B. Provider uncertainty over future reimbursement
When asked about barriers to telehealth adoption, 64% of physicians cited "Uncertainty Around Reimbursement"
2020 Amwell Physician and Consumer Survey https://business.amwell.com/resources/from-virtual-care-to-hybrid-care-covid-19-and-the-future-of-healthcare/">https://business.amwell.com/resources...
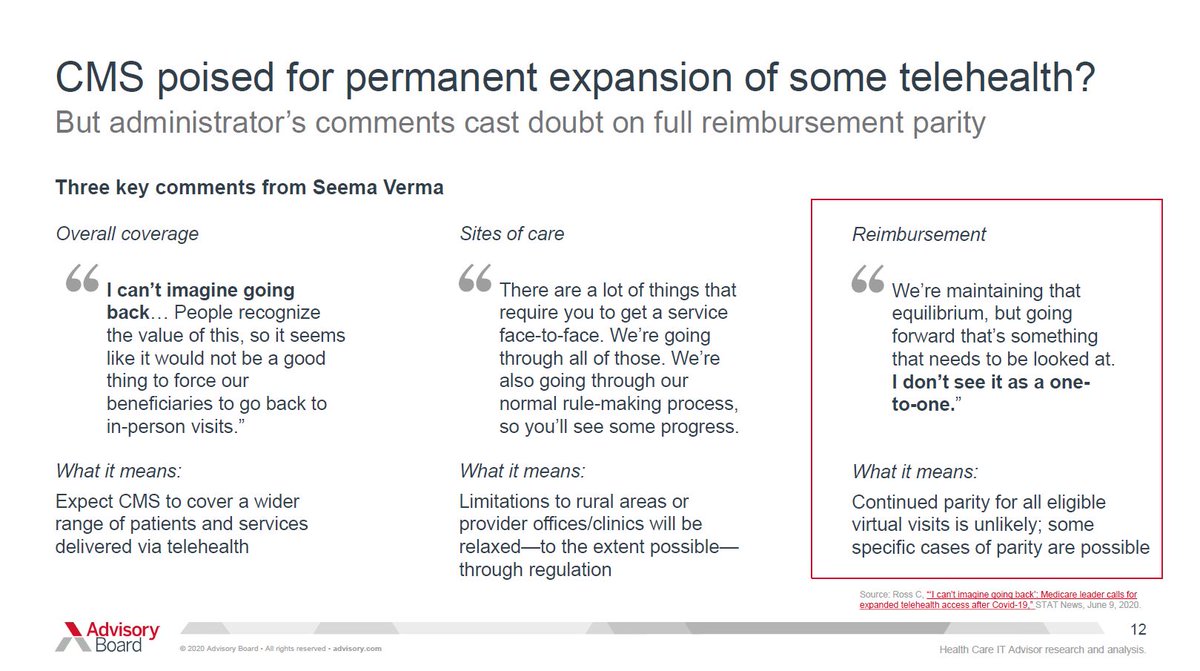
23/
Medicare has been highly supportive of expanded telehealth coverage and reimbursement parity during the COVID-19 Public Health Emergency (PHE).
Will it continue reimbursement parity?
Statements by CMS Administrator @SeemaCMS imply that payments will be lower.
Medicare has been highly supportive of expanded telehealth coverage and reimbursement parity during the COVID-19 Public Health Emergency (PHE).
Will it continue reimbursement parity?
Statements by CMS Administrator @SeemaCMS imply that payments will be lower.
24/
The @AdvisoryBd graphic quotes some of @SeemaCMS& #39; comments on reimbursement parity.
https://bit.ly/372Fx7O
"& #39;I">https://bit.ly/372Fx7O&q... don& #39;t see it as a one-to-one.& #39; What it means: Continued parity for all eligible virtual visits is unlikely; some specific cases of parity are possible."
The @AdvisoryBd graphic quotes some of @SeemaCMS& #39; comments on reimbursement parity.
https://bit.ly/372Fx7O
"& #39;I">https://bit.ly/372Fx7O&q... don& #39;t see it as a one-to-one.& #39; What it means: Continued parity for all eligible virtual visits is unlikely; some specific cases of parity are possible."
25/
Parity in coverage and parity in reimbursement are not the same. Here& #39;s a primer https://visuwell.io/news/parity-explained/">https://visuwell.io/news/pari... HT @RasuShrestha
@SeemaCMS has been more positive about the need for ongoing telehealth coverage: "Telehealth should be a permanent benefit..." https://twitter.com/RasuShrestha/status/1316048678512140288?s=20">https://twitter.com/RasuShres...
Parity in coverage and parity in reimbursement are not the same. Here& #39;s a primer https://visuwell.io/news/parity-explained/">https://visuwell.io/news/pari... HT @RasuShrestha
@SeemaCMS has been more positive about the need for ongoing telehealth coverage: "Telehealth should be a permanent benefit..." https://twitter.com/RasuShrestha/status/1316048678512140288?s=20">https://twitter.com/RasuShres...
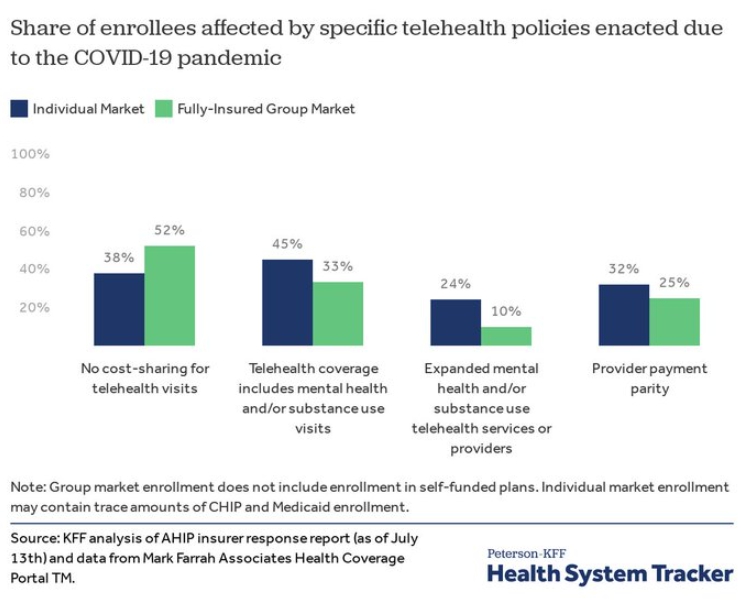
26/
During COVID-19, private payer reimbursement support has been cautious.
@KFF study http://bit.ly/3kXEJ8Z
Among">https://bit.ly/3kXEJ8Z&q... individual market health plans:
32% of enrollees are in plans with $$ parity for telehealth.
27% because of state mandates.
only 5% voluntary.
During COVID-19, private payer reimbursement support has been cautious.
@KFF study http://bit.ly/3kXEJ8Z
Among">https://bit.ly/3kXEJ8Z&q... individual market health plans:
32% of enrollees are in plans with $$ parity for telehealth.
27% because of state mandates.
only 5% voluntary.
27/
Some plans are rolling back enhanced coverage.
@UHC is ending a “virtual visit” benefit that had been expanded to many members... @AnthemBCBS will stop waiving the cost of copays, coinsurance, & deductibles for virtual visits not related to COVID-19. https://bit.ly/2SiV4YJ ">https://bit.ly/2SiV4YJ&q...
Some plans are rolling back enhanced coverage.
@UHC is ending a “virtual visit” benefit that had been expanded to many members... @AnthemBCBS will stop waiving the cost of copays, coinsurance, & deductibles for virtual visits not related to COVID-19. https://bit.ly/2SiV4YJ ">https://bit.ly/2SiV4YJ&q...
28/
C. Many providers will have concerns about new competition.
A @McKinsey report noted that "up to $250 billion of current US healthcare spend could potentially be virtualized"
https://mck.co/2XPje0i
There">https://mck.co/2XPje0i&q... will be winners. There will be losers.
C. Many providers will have concerns about new competition.
A @McKinsey report noted that "up to $250 billion of current US healthcare spend could potentially be virtualized"
https://mck.co/2XPje0i
There">https://mck.co/2XPje0i&q... will be winners. There will be losers.
29/
Potential new competitors (and/or partners!):
Local providers (MDs/hospitals/etc.) vs. local providers.
Local providers vs. national virtual visit providers.
Local providers vs. local/national payers.
Local providers vs. big tech companies
Potential new competitors (and/or partners!):
Local providers (MDs/hospitals/etc.) vs. local providers.
Local providers vs. national virtual visit providers.
Local providers vs. local/national payers.
Local providers vs. big tech companies
30/
D. Regulatory Quagmire
The regulatory DEFAULT after PHE waivers and rule relaxations expire is a return to the Pre COVID-19 old normal.
The regulatory Pre COVID-19 old normal for telehealth regulations was a mess.
D. Regulatory Quagmire
The regulatory DEFAULT after PHE waivers and rule relaxations expire is a return to the Pre COVID-19 old normal.
The regulatory Pre COVID-19 old normal for telehealth regulations was a mess.
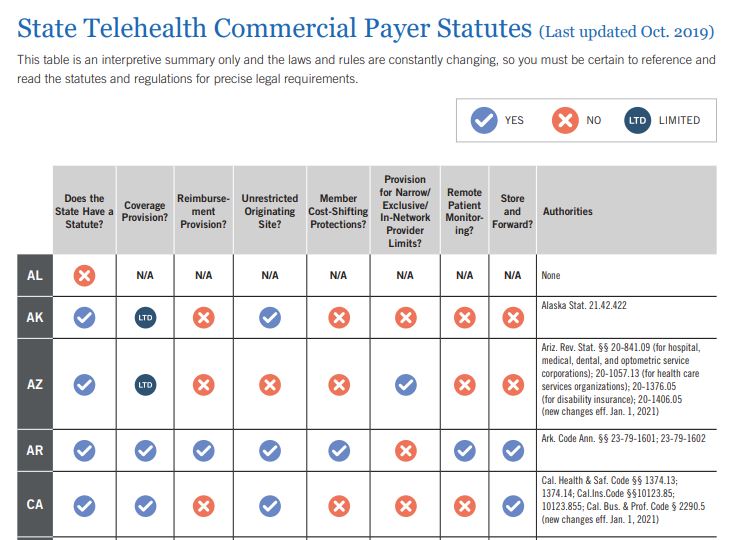
31/
Prior to COVID-19, 42 states and DC maintained a commercial telehealth payer statute.
"Unfortunately, the quality and efficacy of these laws varies significantly from state to state."
-- @FoleyandLardner https://bit.ly/3m5Yx9L ">https://bit.ly/3m5Yx9L&q...
Prior to COVID-19, 42 states and DC maintained a commercial telehealth payer statute.
"Unfortunately, the quality and efficacy of these laws varies significantly from state to state."
-- @FoleyandLardner https://bit.ly/3m5Yx9L ">https://bit.ly/3m5Yx9L&q...
32/
@FoleyandLardner describe differences:
Does the state have a statute?
Coverage provision?
Reimbursement provision?
Unrestricted originating site?
Member cost-shifting provision?
Narrow/exclusive in-network provider limits?
Remote patient monitoring?
Store and forward?
@FoleyandLardner describe differences:
Does the state have a statute?
Coverage provision?
Reimbursement provision?
Unrestricted originating site?
Member cost-shifting provision?
Narrow/exclusive in-network provider limits?
Remote patient monitoring?
Store and forward?
33/
State licensure relaxations are not permanent.
Governors& #39; temporary waivers of professional licensure for out-of-state telehealth "state licensure waivers are temporary, and, unless made permanent, will expire" https://bit.ly/37pLID3 ">https://bit.ly/37pLID3&q...
State licensure relaxations are not permanent.
Governors& #39; temporary waivers of professional licensure for out-of-state telehealth "state licensure waivers are temporary, and, unless made permanent, will expire" https://bit.ly/37pLID3 ">https://bit.ly/37pLID3&q...
34/
Physician groups are already attempting to limit competition.
Led by the American Medical Association, more than 100 medical groups called on the CMS to sunset waivers related to scope of practice and licensure once the pandemic has subsided. https://bit.ly/2XlExWY ">https://bit.ly/2XlExWY&q...
Physician groups are already attempting to limit competition.
Led by the American Medical Association, more than 100 medical groups called on the CMS to sunset waivers related to scope of practice and licensure once the pandemic has subsided. https://bit.ly/2XlExWY ">https://bit.ly/2XlExWY&q...
35/
Dr. Ronald Hirsch @signaturedoc https://bit.ly/3ma0hz1 ">https://bit.ly/3ma0hz1&q... :
"While the declaration of a public health emergency allowed CMS to issue emergency waivers for many regulations, once the waivers expire, things will go back to standard operating procedures.
Dr. Ronald Hirsch @signaturedoc https://bit.ly/3ma0hz1 ">https://bit.ly/3ma0hz1&q... :
"While the declaration of a public health emergency allowed CMS to issue emergency waivers for many regulations, once the waivers expire, things will go back to standard operating procedures.
36/
"any substantive change will have to go through the formal rulemaking process, w/ drafting by CMS staff, review by the OMB, publication..., a mandated comment period, & then a second review & finally publication of a final rule, w/ an effective date at least 60 days later."
"any substantive change will have to go through the formal rulemaking process, w/ drafting by CMS staff, review by the OMB, publication..., a mandated comment period, & then a second review & finally publication of a final rule, w/ an effective date at least 60 days later."
37/ IMPLICATIONS.
So what happens when the IRRESISTIBLE FORCE meets the IMMOVABLE OBJECT?
TBD.
There are MANY implications (but that& #39;s another thread).
A key takeaway: Telehealth successes to-date should not be taken for granted.
So what happens when the IRRESISTIBLE FORCE meets the IMMOVABLE OBJECT?
TBD.
There are MANY implications (but that& #39;s another thread).
A key takeaway: Telehealth successes to-date should not be taken for granted.

 Read on Twitter
Read on Twitter