Time for some tweet-ucation from our morning #CHEST2020 session on “Cystic Fibrosis Pulmonary Exacerbations: What Every Pulmonologist Should Know”!
So what is a pulmonary exacerbation? There is no agreed upon definition.
The American Cystic Fibrosis Foundation gives a simple definition in the family handbook as ‘‘signs and symptoms that show a need for treatment’.”
#CHEST2020
The American Cystic Fibrosis Foundation gives a simple definition in the family handbook as ‘‘signs and symptoms that show a need for treatment’.”
#CHEST2020
Some studies classify exacerbations as a physician-defined requirement to treat with new antibiotic therapy. #CHEST2020
A pulmonary exacerbation is typically characterized by worsening symptoms like increased cough, increased sputum production, shortness of breath, chest pain, loss of appetite, loss of weight, & lung function decline.
#CHEST2020
#CHEST2020
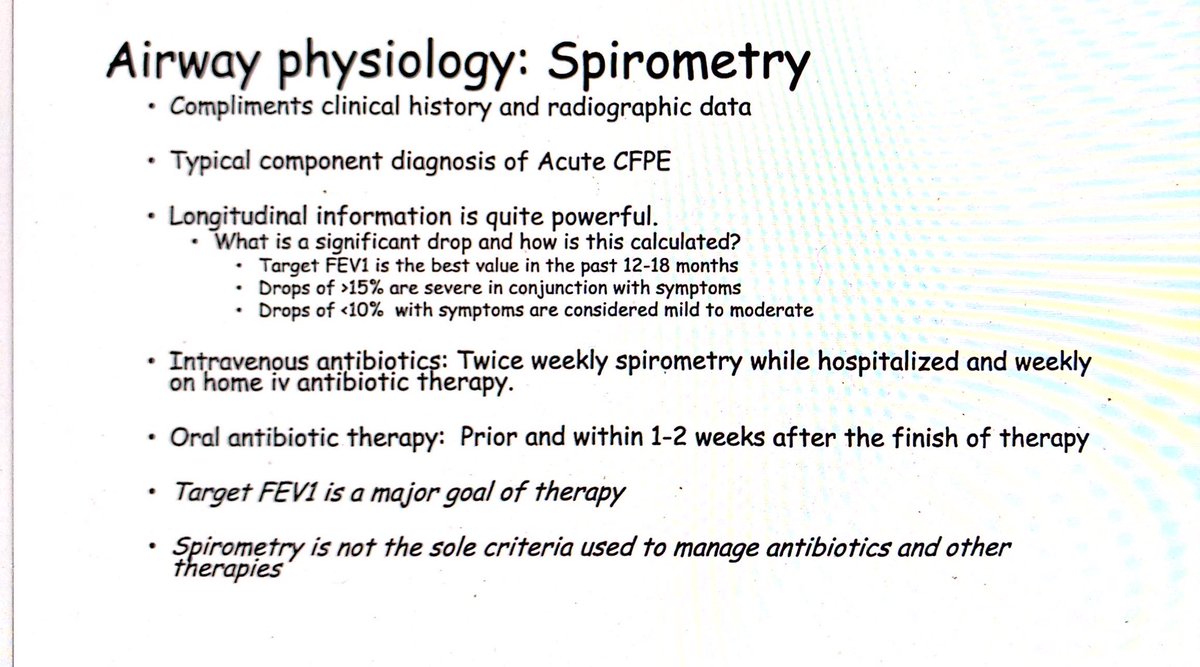
We typically offer treatment in patients with stable symptoms if they have an FEV1 decline of >5-10%. #CHEST2020
We know that pulmonary exacerbations have an adverse impact on patients’ quality of life. They also have an impact on survival in CF, they adversely affect sleep and neurobehavioral performance, and they increase health costs. #CHEST2020
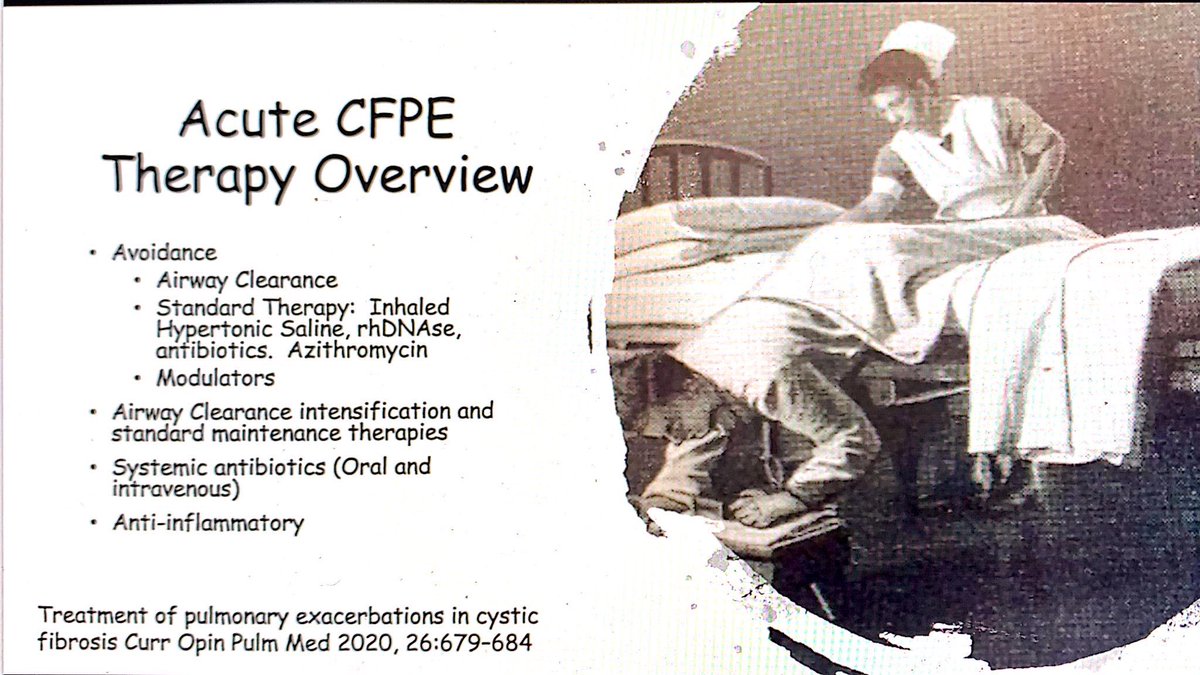
Airway clearance still plays a vital role in the treatment of pulmonary exacerbations.
Airway clearance includes things like nebulized treatments, positive expiratory pressure devices, and VEST therapy. #CHEST2020
Airway clearance includes things like nebulized treatments, positive expiratory pressure devices, and VEST therapy. #CHEST2020
In general airway clearance therapies should be intensified as part of the treatment of an acute exacerbation.
We typically increase the quantity to 4 times a day and if they tolerate it you can do longer sessions of chest physiotherapy. #CHEST2020
We typically increase the quantity to 4 times a day and if they tolerate it you can do longer sessions of chest physiotherapy. #CHEST2020
For patients with a presumed upper respiratory viral infection accompanied by a persistent cough for more than 3–5 days or other lower respiratory symptoms, it is common to start an oral antibiotic. #CHEST2020
Some of it also depends on insurance and patient preference. It’s not uncommon for patients to request to try oral antibiotics first and then to agree to IV treatment if they fail to improve.
#CHEST2020
#CHEST2020
Interestingly a study in the UK found that CF care sites with patients with the best lung function prescribe IV antibiotics more frequently than sites who have a lower average FEV1. #CHEST2020
Home intravenous antibiotic therapy is used in individual cases, but the patient needs to have access to the same therapies and monitoring at home they would be afforded as an inpatient. #CHEST2020
One comparative trial looked at treatment of pulmonary exacerbations at home vs in the hospital. It demonstrated similar results in most outcome measures for home and hospital settings. #CHEST2020
However, there are observational studies that suggest better outcomes for patients treated in a hospital than at home.
If there is any doubt, I recommend hospital admission.
#CHEST2020
If there is any doubt, I recommend hospital admission.
#CHEST2020
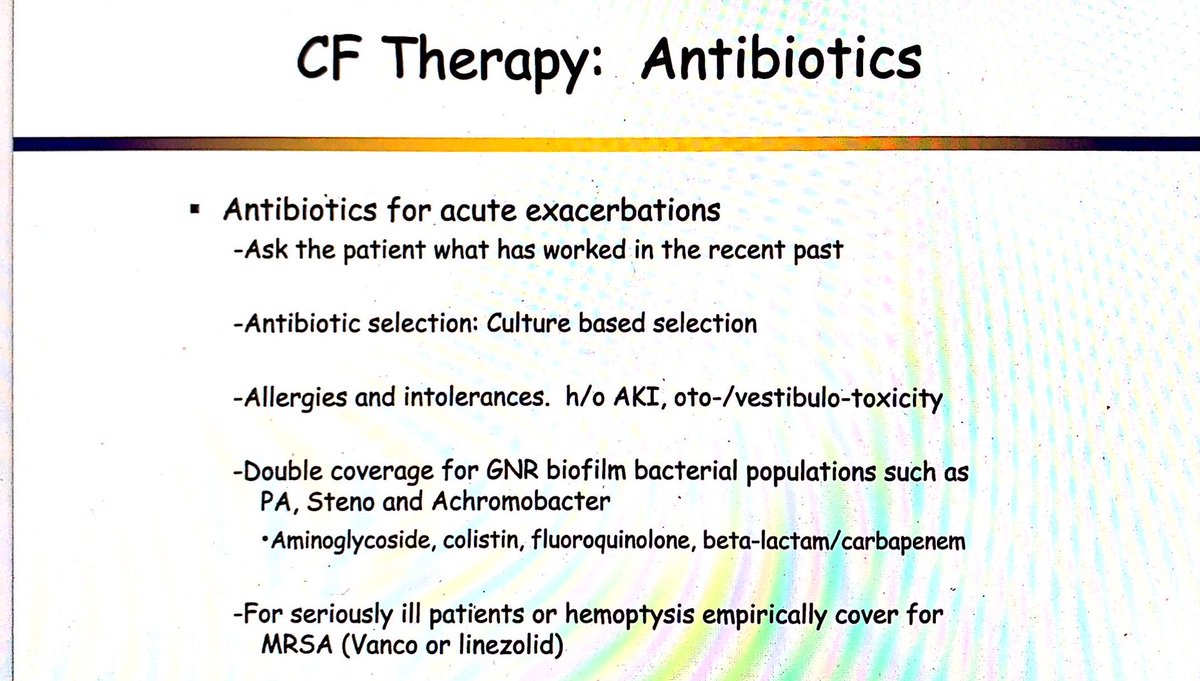
Antibiotic choice should be tailored towards culture results.
We typically treat any bacteria that has grown in the past 12 months. #CHEST2020
We typically treat any bacteria that has grown in the past 12 months. #CHEST2020
The most common pathogen identified in airway cultures of patients with cystic fibrosis is Pseudomonas aeruginosa. Other common pathogens include Haemophilus influenzae, Staphylococcus aureus (including MRSA), and Stenotrophomonas maltophilia. #CHEST2020
For Pseudomonas aeruginosa dual coverage is generally recommended to enhance activity and reduce resistance. However, trials have not sufficiently demonstrated that dual or mono coverage is more beneficial. #CHEST2020
Many patients with CF are on supplements, so it’s important to note that Doxycycline and Ciprofloxacin are chelators of iron, calcium, and magnesium. If patients are on those supplements you should separate them from the antibiotics by 4 hours. #CHEST2020
Make sure you consider safety of antibiotics in pregnant patients. During CHEST 2019 Trikafta was FDA approved, and one of its many effects is thinner cervical mucous so we are seeing a Trikafta baby boom and it’s important to keep this in mind! #CHEST2020
There is evidence that patients with CF benefit from use of long-term inhaled antibiotics and a suggestion that they may also benefit from the use of inhaled antibiotics during an exacerbation. #CHEST2020
There is not sufficient evidence to determine whether it is of additional benefit to have a patient on both IV and inhaled versions of the same antibiotic. #CHEST2020
There is also insufficient evidence regarding whether a patient on chronic inhaled antibiotics should be continued on them during treatment for an acute pulmonary exacerbation, so it’s really physician preference. #CHEST2020
We often add an inhaled antipseudomonal antibiotic to dual IV treatment of Pseudomonas if the patient has grown a particularly resistant strain. #CHEST2020
Remember, if you do give an inhaled antibiotic you should always premedicate with a bronchodilator as they can cause bronchospasm. #CHEST2020
The pharmacokinetics of antibiotics are different in patients with CF than those without CF, thus antibiotics dosages need to be adjusted based on their levels and they often require higher doses. #CHEST2020
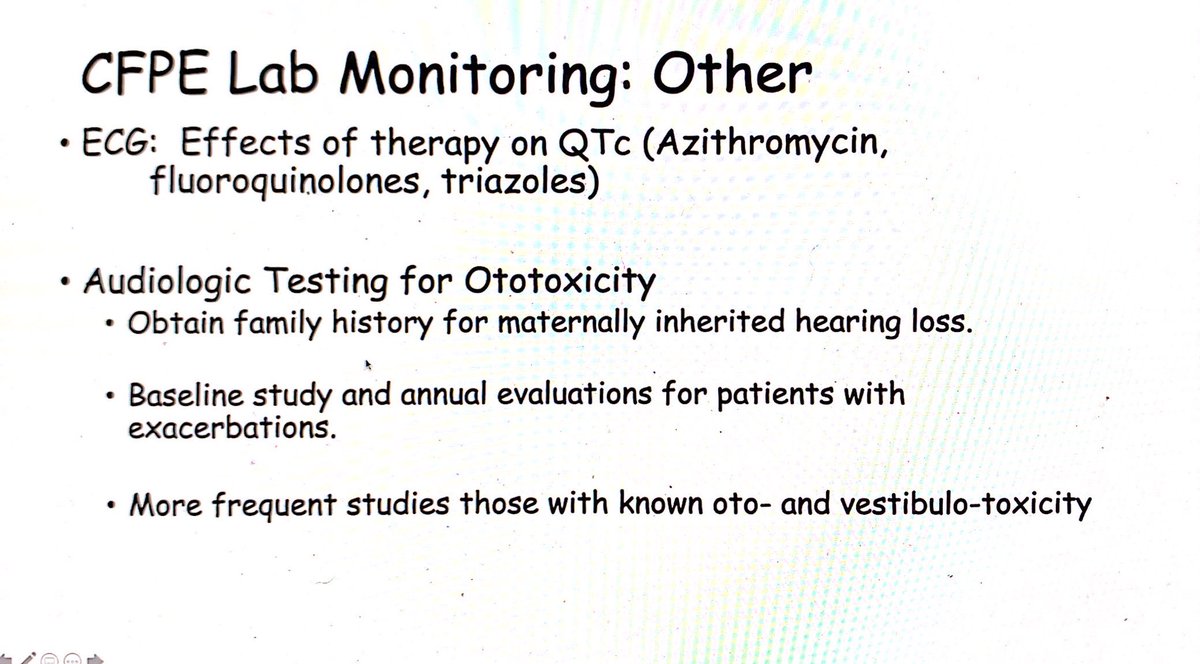
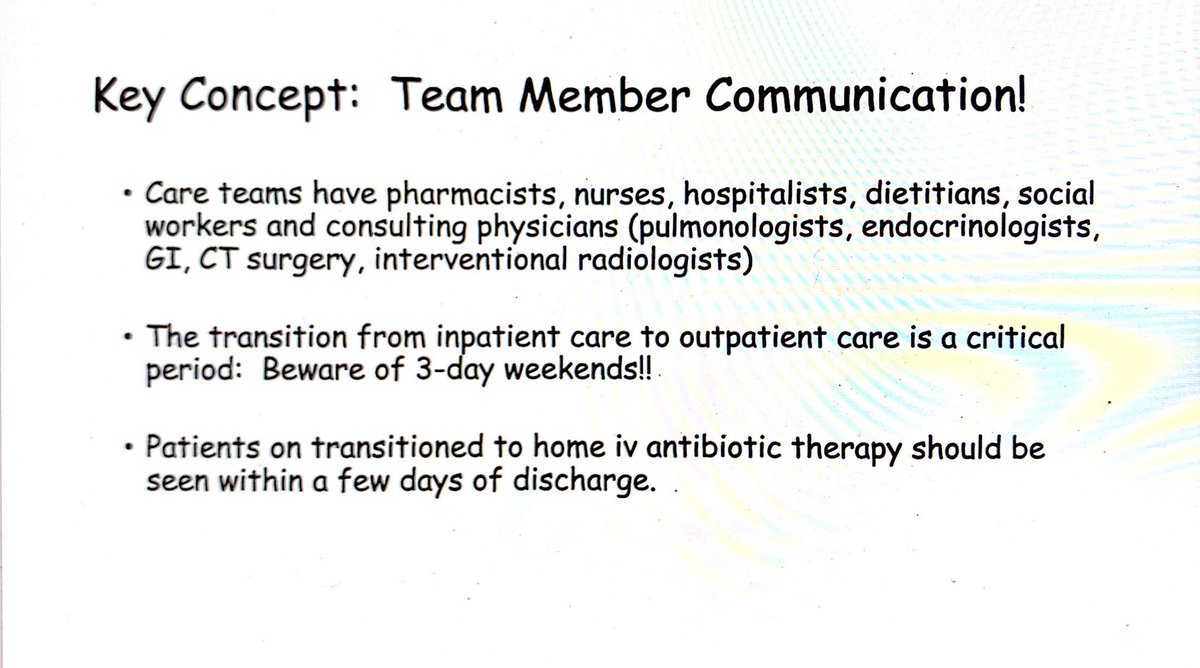
Treatment of cystic fibrosis can lead to its own complications due to medication toxicity and interactions. The inclusion of a specialized pharmacist as part of the CF team is very important. #CHEST2020
The CF Foundation does recommend that once-daily dosing of aminoglycosides is preferable to 3-times daily dosing. #CHEST2020
The CF Foundation also concluded that there is insufficient evidence to recommend the continuous infusion of b-lactam antibiotics. However, anecdotally we sometimes see improvement with continuous over intermittent dosing. #CHEST2020
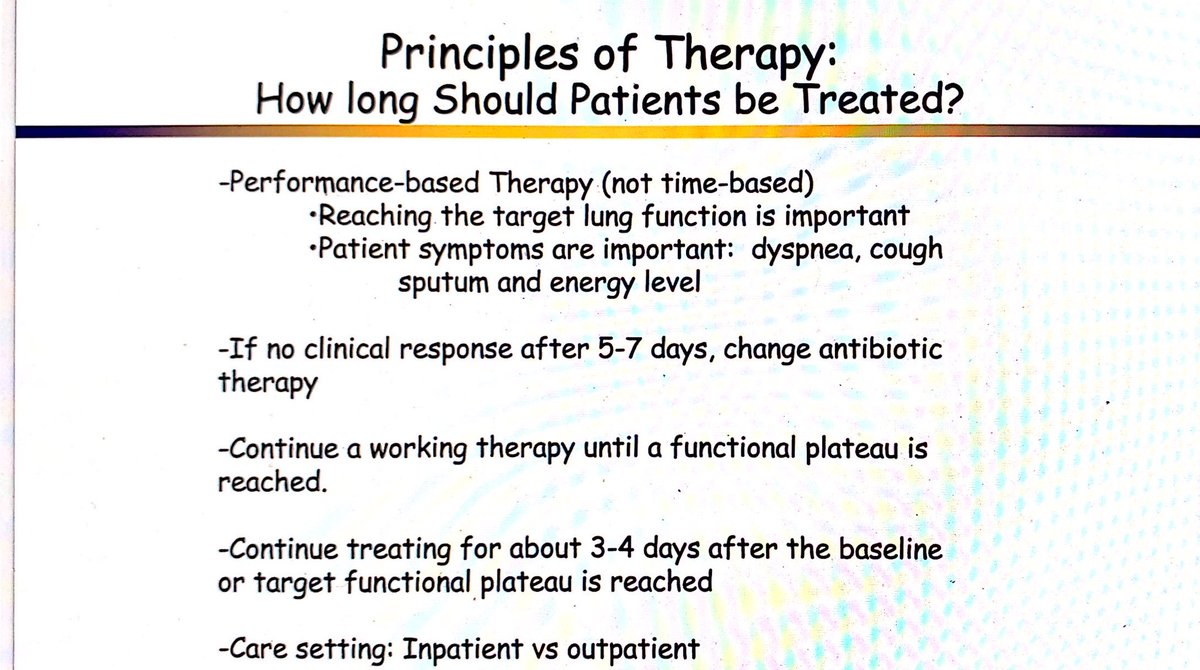
Duration of treatment is generally recommended to be 14 days, but data is lacking, and some suggest a minimum duration of 10 days. #CHEST2020
A large multicenter retrospective study indicated that improvement in FEV1 plateaus after 7–10 days of therapy, but t’s unclear whether treatment for 14 days leads to sustained clinical benefit and lung function may not be the most helpful parameter to follow. #CHEST2020
Some patients may benefit from longer therapy and that decision should be based on medical needs rather than resources and costs. In one study, parents and children felt that a third week was subjectively beneficial. #CHEST2020
The STOP-2 trial just finished and the results will be submitted for publication soon. It looked at the safety and effectiveness of different lengths of IV treatment for pulmonary exacerbations. We are eagerly anticipating these results. #CHEST2020
Consider drug interactions and whether you need to adjust dose.
Fluconazole and other triazoles, Clarithromycin, Erythromycin all increase Trikafta levels so you should decrease Trikafta dose. #CHEST2020
Fluconazole and other triazoles, Clarithromycin, Erythromycin all increase Trikafta levels so you should decrease Trikafta dose. #CHEST2020
Rifampin, Rifabutin, Phenobarbital, Carbamazepine, Phenytoin, and St. John’s Wort decrease Trikafta levels, so it’s contraindicated to use these together. #CHEST2020
I consider bronchoscopy if patients don’t improve with treatment to make sure we’re not missing something on culture. #CHEST2020
Consider treatment of NTM if they don’t improve with typical therapy and cultures and imaging suggest they have an active infection.
Consider ABPA if their IgE is rising and the patient doesn’t improve, especially if they have a lot of mucous and wheezing. #CHEST2020
Consider ABPA if their IgE is rising and the patient doesn’t improve, especially if they have a lot of mucous and wheezing. #CHEST2020
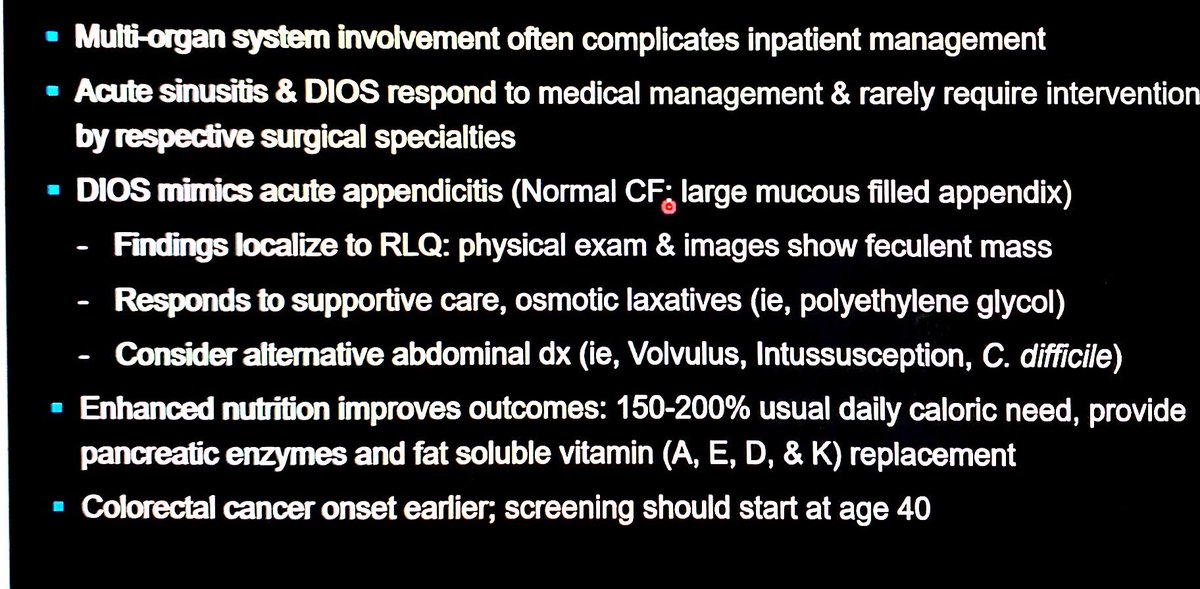
Next up is Dr. Doug Hornick talking in "CF Comorbidities: DIOS, Sinusitis, and Pancreatic Insufficiency”! #CHEST2020
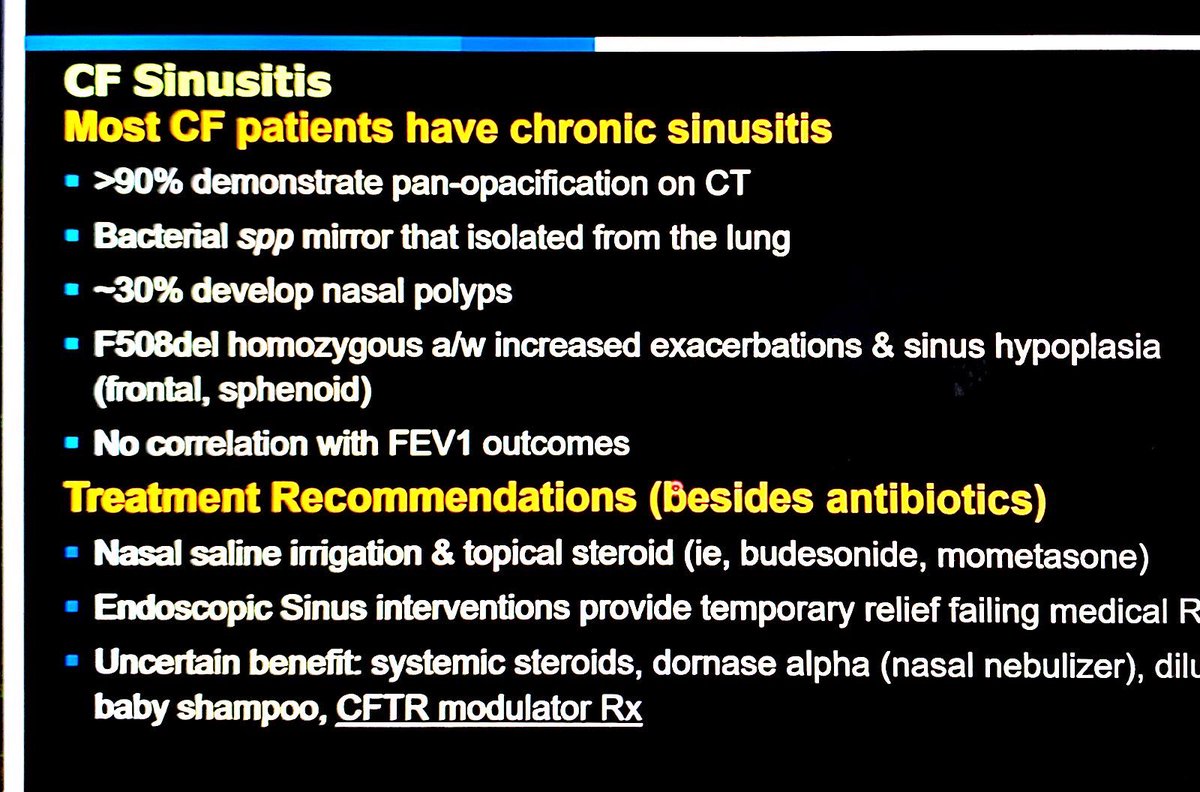
CF sinusitis is very common! Treatment recommendations include nasal saline irrigation and topical steroids. Endoscopic interventions provide temporary relief. #CHEST2020
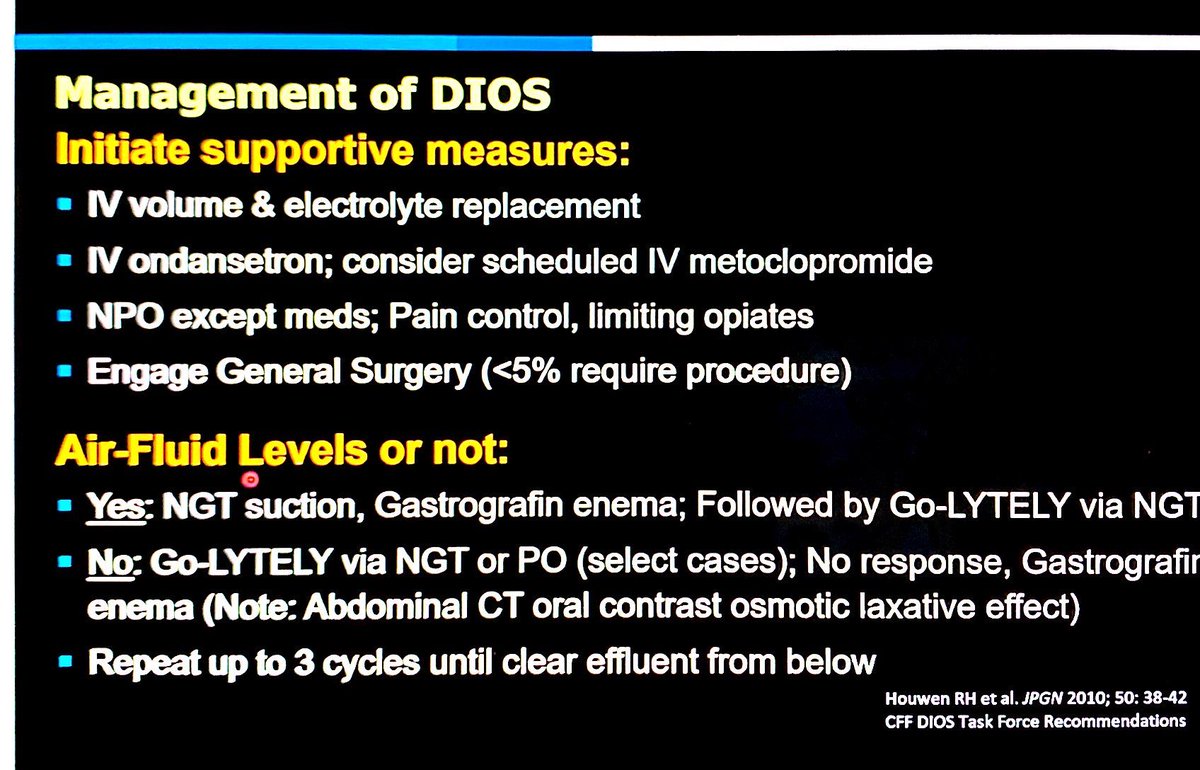
DIOS occurs in 10-47% of patients with CF. The most predictive thing of an episode of DIOS is a prior episode of DIOS. Osmotic laxatives are the first line treatment. #CHEST2020
Clinical features of DIOS include abdominal pain w/wo distension. KUB shows SBO with air-fluid levels and impacted RLQ. Note that a CF appendix is usually enlarged on CT due to mucous impaction. #CHEST2020
When it& #39;s only constipation instead of DIOS the patient will have less intense abdominal discomfort, they will strain to defecate and have more flatulence. Imaging does not have air-fluid levels and has stool throughout colon. #CHEST2020
Management of DIOS. Keep in mind that surgeons who are inexperienced with DIOS may recommend surgery when it is not needed and it can cause more harm. Less than 5% of these patients actually require surgery. #CHEST2020
Once DIOS resolves make sure you emphasize adherence with pancreatic enzymes! #CHEST2020
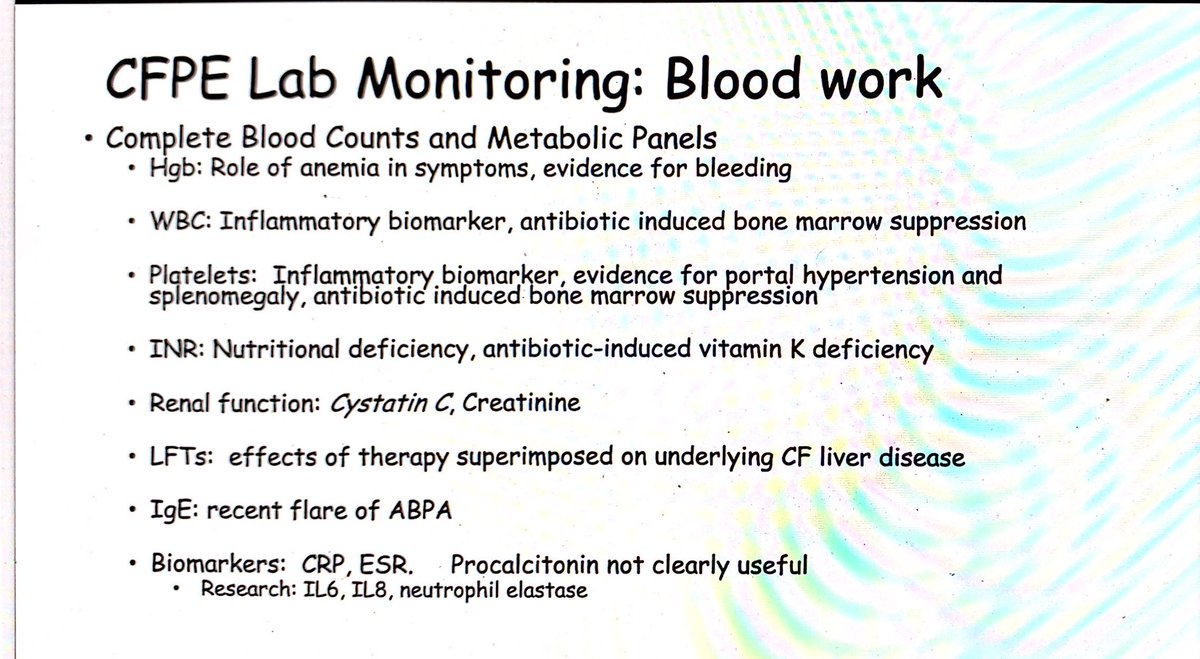
Our final topic is "Laboratory, Radiographic, and Physiologic Monitoring" with Dr. Douglas Conrad! #CHEST2020
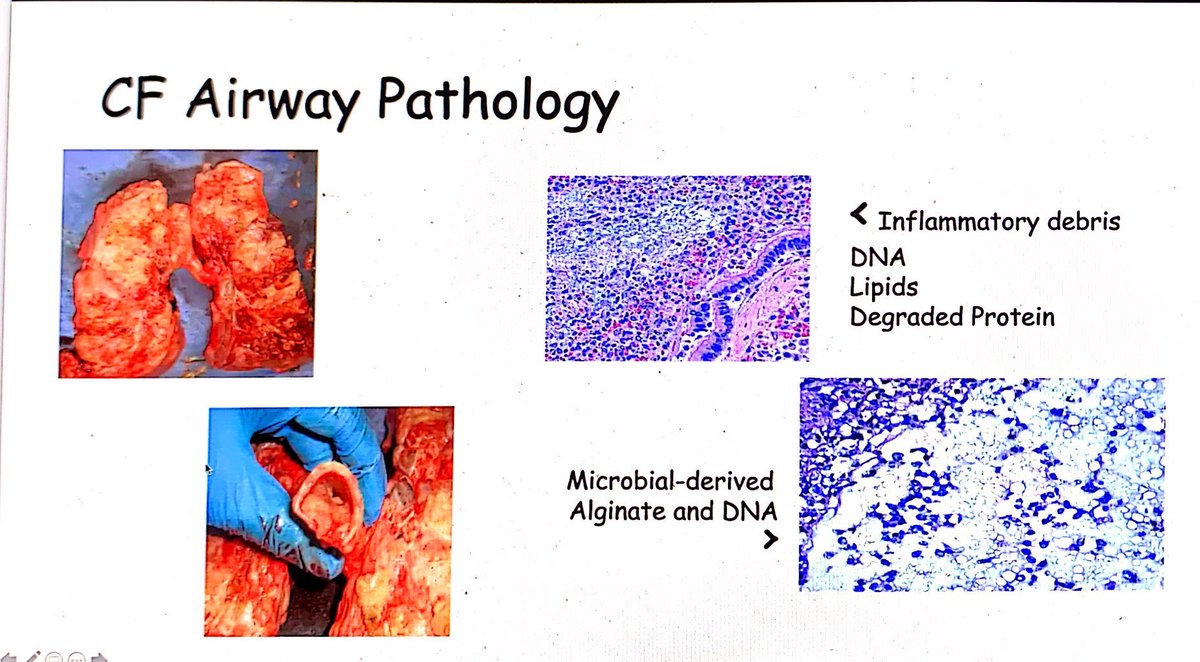
The ecology of the CF lung includes the attack community and the climax community. The attack comunity causes inflammation. The climax community includes bacteria that stay in the CF lung over time as the bronchiectasis progresses, #CHEST2020
CF pulmonary exacerbations are clinical syndromes associated with increased symptoms and changes in airway physiology. #CHEST2020
One of our major clinical goals is to decrease the frequency of exacerbations as they are major events for CF patients that are associated with irreversible loss of lung function. #CHEST2020
Overview of antibiotics for CF pulmonary exacerbations. The patient often knows what has worked well for them in the past. Section based on cultures and history of intolerances. Double cover Pseudomonas/Stenotrophomonas/Achromobacter. Empirically cover MRSA if ill. #CHEST2020
How long to treat? Consider performance-based therapy rather than time-based. Treat with the goal of reaching target lung function and improvement in patient symptoms. #CHEST2020
Monitoring lung function with spirometry. It is so important to monitor FEV1 and treat accordingly, both routinely and during exacerbations. FEV1 is not the only criteria in pulmonary exacerbations - symptoms are important and these patients know their bodies! #CHEST2020
You should monitor cultures in patients with CF to know what is growing (although it is not comprehensive). Note that susceptibility testing is not predictive of clinical outcomes. #CHEST2020
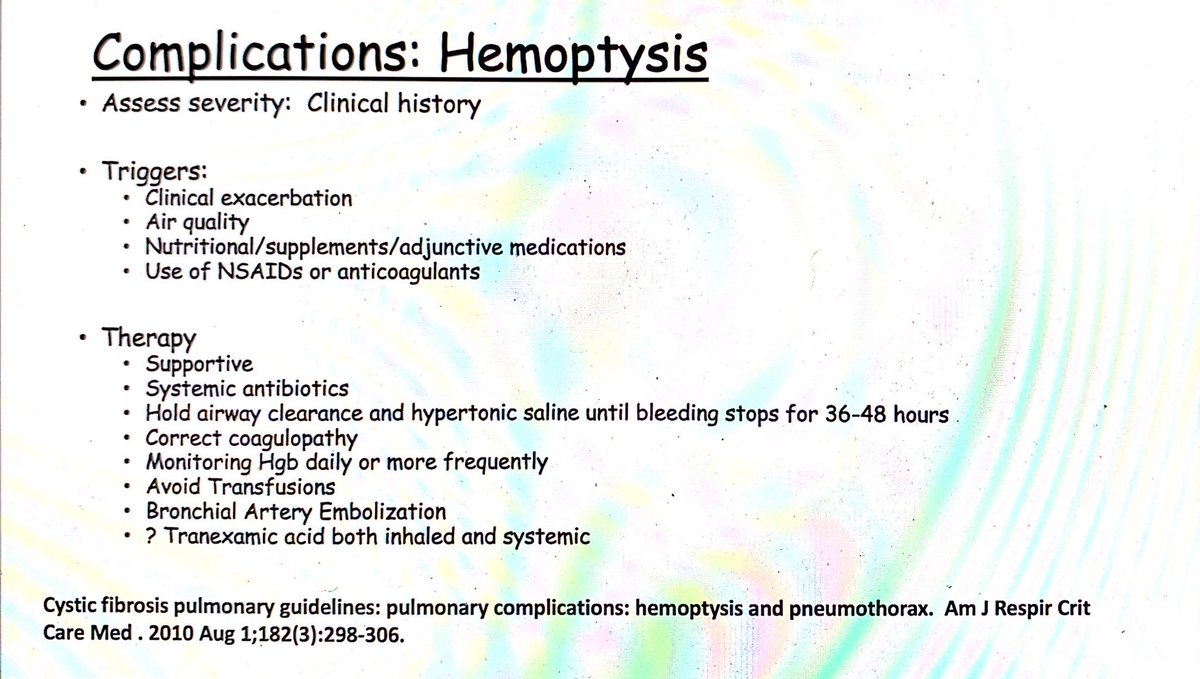
Assess severity of hemoptysis by clinical history. Identify triggers. Therapy is supportive. Consider antibiotics. Hold abrasive airway clearance. May require bronchial artery embolization if severe. #CHEST2020
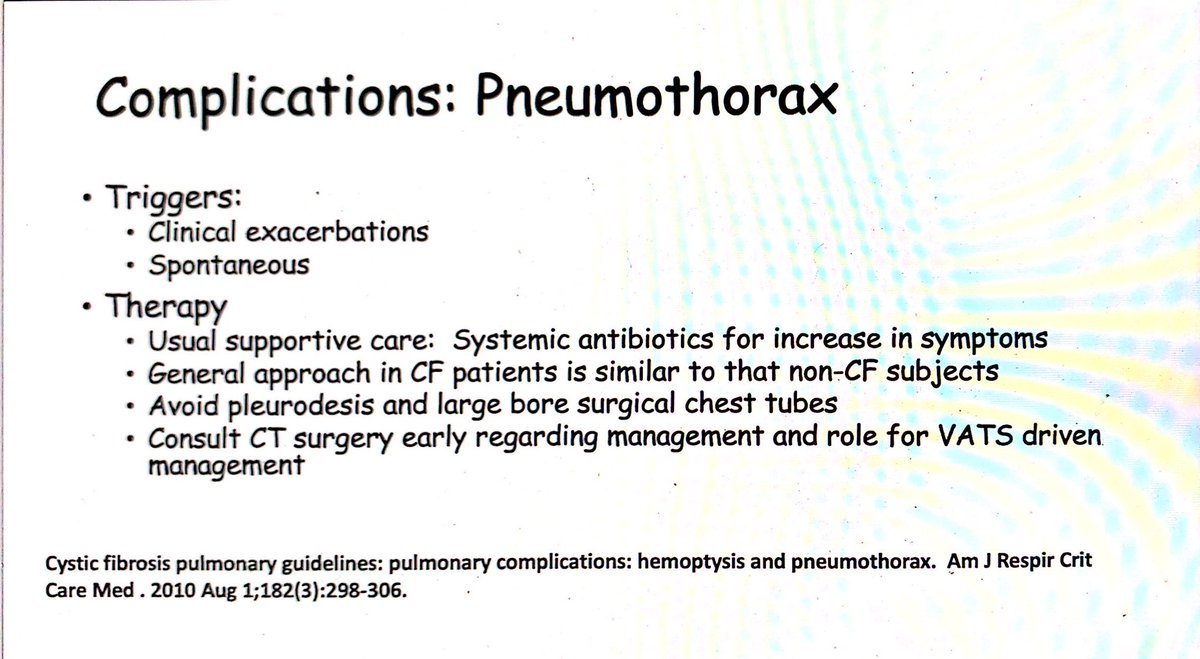
Pneumothoraces are common spontaneously. Usually supportive care. Consider CTS consult early on. Avoid large bore chest tubes and pleurodesis. #CHEST2020

 Read on Twitter
Read on Twitter