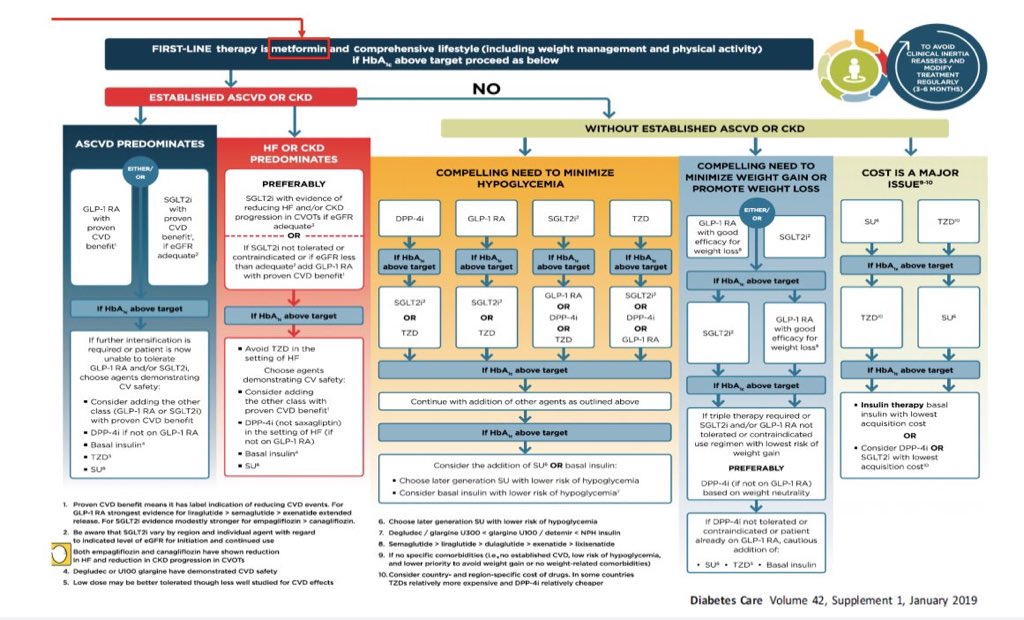
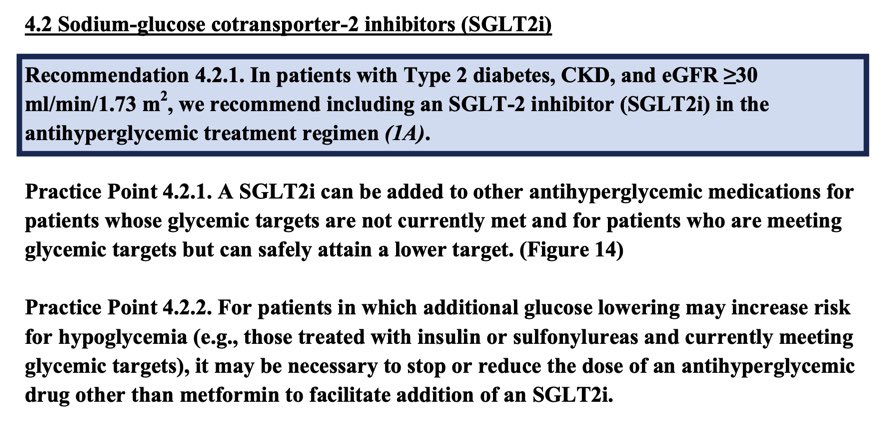
Almost all guidelines recommend SGLT2i as 2nd line in T2DM & CKD/HF if not achieving glucose control on metformin
But should “metformin 1st for all” be revisited given the latest trial evidence?
A thread on metformin, guidelines & our new meta-analysis https://dom-pubs.onlinelibrary.wiley.com/doi/abs/10.1111/dom.14226">https://dom-pubs.onlinelibrary.wiley.com/doi/abs/1...
But should “metformin 1st for all” be revisited given the latest trial evidence?
A thread on metformin, guidelines & our new meta-analysis https://dom-pubs.onlinelibrary.wiley.com/doi/abs/10.1111/dom.14226">https://dom-pubs.onlinelibrary.wiley.com/doi/abs/1...
Metformin is cheap, well tolerated, effective at lowering glucose & has been used for decades.
The main randomised evidence for its CV benefits comes from 1709 obese individuals in the UKPDS trial, where metformin https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> risk of MI and mortality over ~10y follow up
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> risk of MI and mortality over ~10y follow up
The main randomised evidence for its CV benefits comes from 1709 obese individuals in the UKPDS trial, where metformin
UKPDS ( https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(98)07037-8/fulltext)">https://www.thelancet.com/journals/... was published over 2 decades ago, prior to the widespread use of RAS blockade, statins etc, with metformin being compared with early generation glucose lowering drugs/diet, making comparison with Rx effects in contemporary trials challenging
These CV benefits observed in UKPDS have largely not been corroborated in subsequent randomised trials, or meta-analyses of these trials https://link.springer.com/article/10.1007/s00125-017-4337-9">https://link.springer.com/article/1...
Nevertheless, almost all clinical practice guidelines recommend metformin as first line treatment, with the addition of SGLT2i in patients with CKD/heart failure if they are not achieving sufficient glucose control on metformin alone
Recommendations from ADA/EASD & KDIGO:
Recommendations from ADA/EASD & KDIGO:
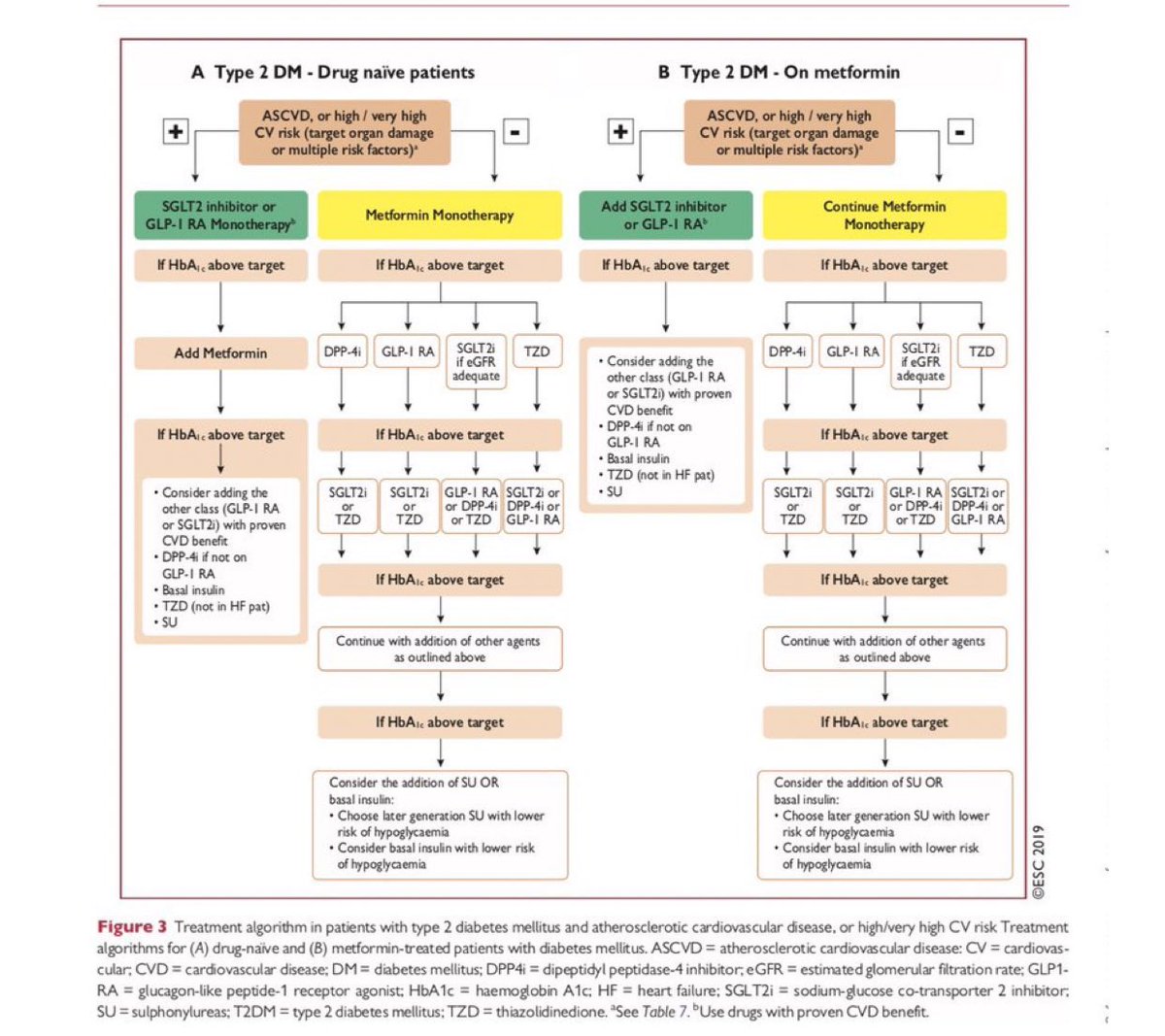
Somewhat controversially in 2019, the ESC broke rank with other guidelines and recommended SGLT2i/GLP-1RA in patients at very high CV risk “regardless of whether the are treatment naive or already receiving metformin” https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Diabetes-Pre-Diabetes-and-Cardiovascular-Diseases-developed-with-the-EASD">https://www.escardio.org/Guideline...
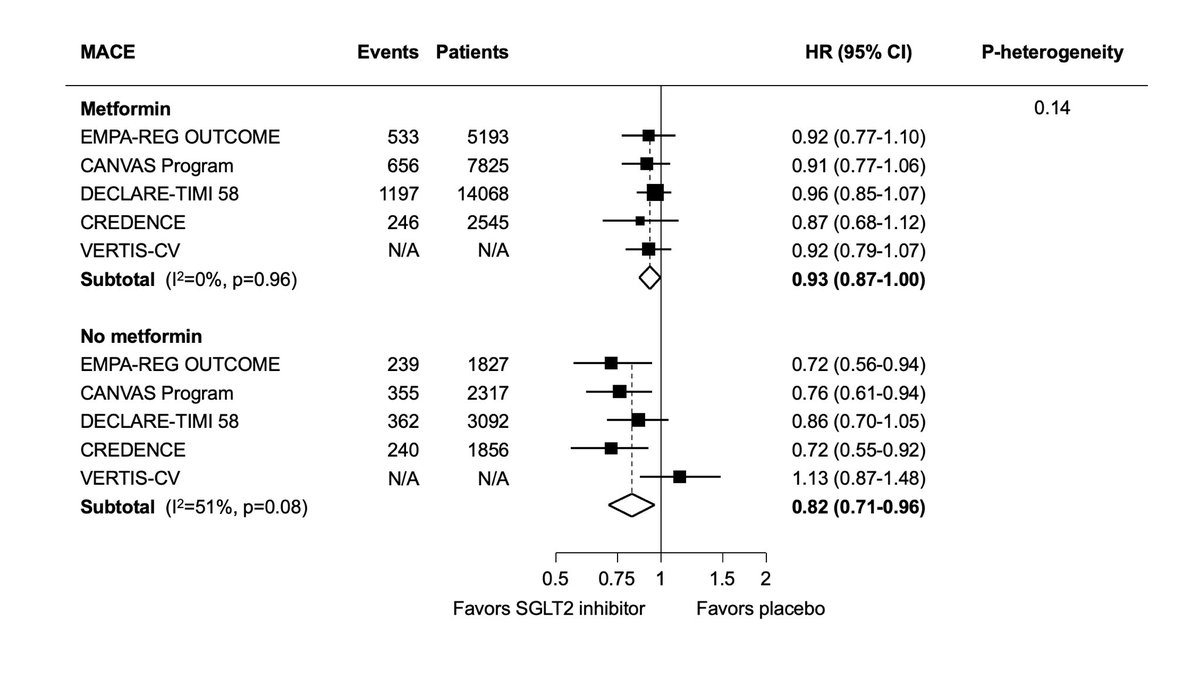
So what is the evidence for the effect of SGLT2 inhibitors, with and without metformin, on CV, renal and mortality outcomes?
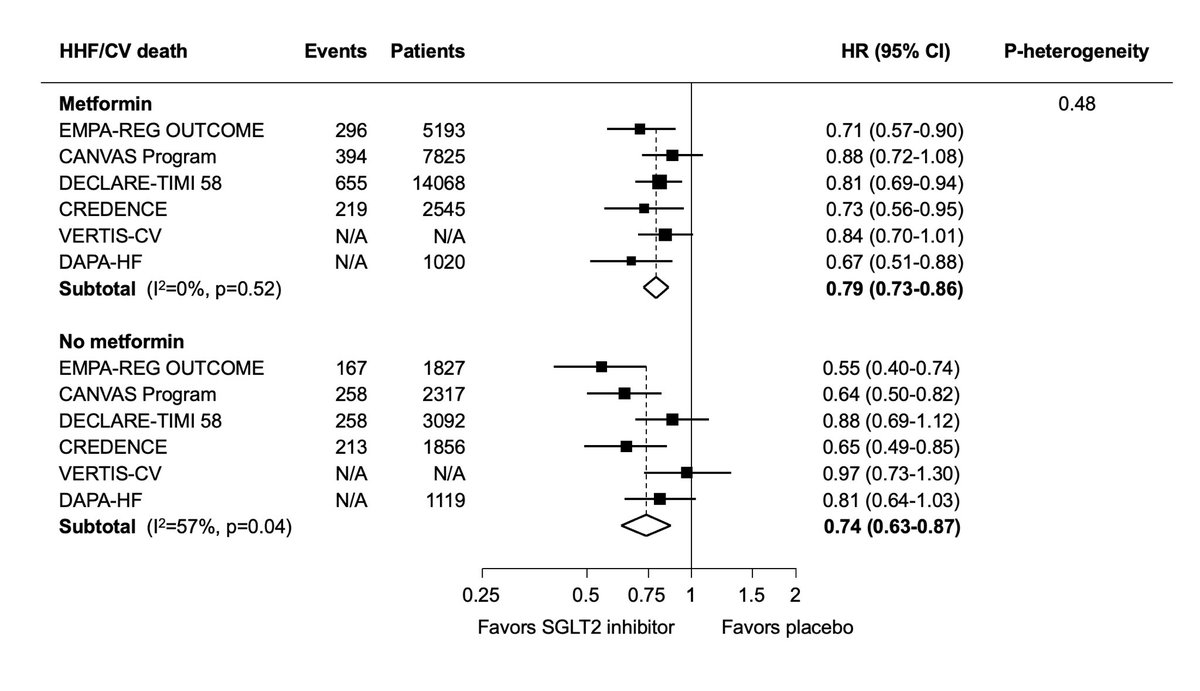
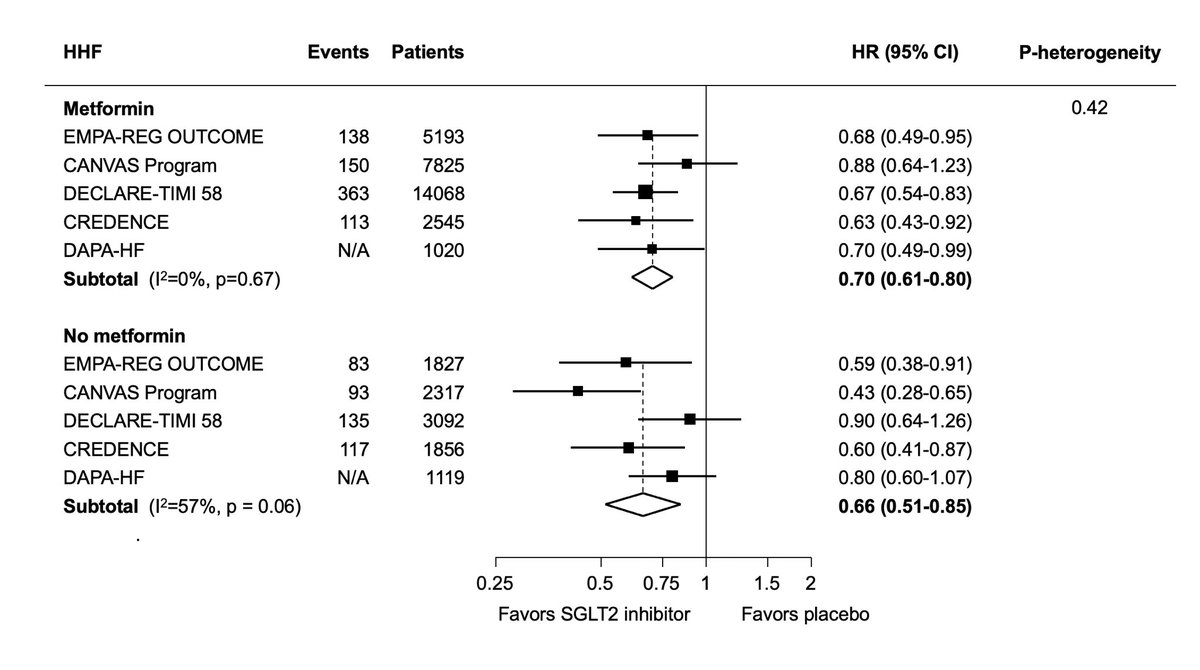
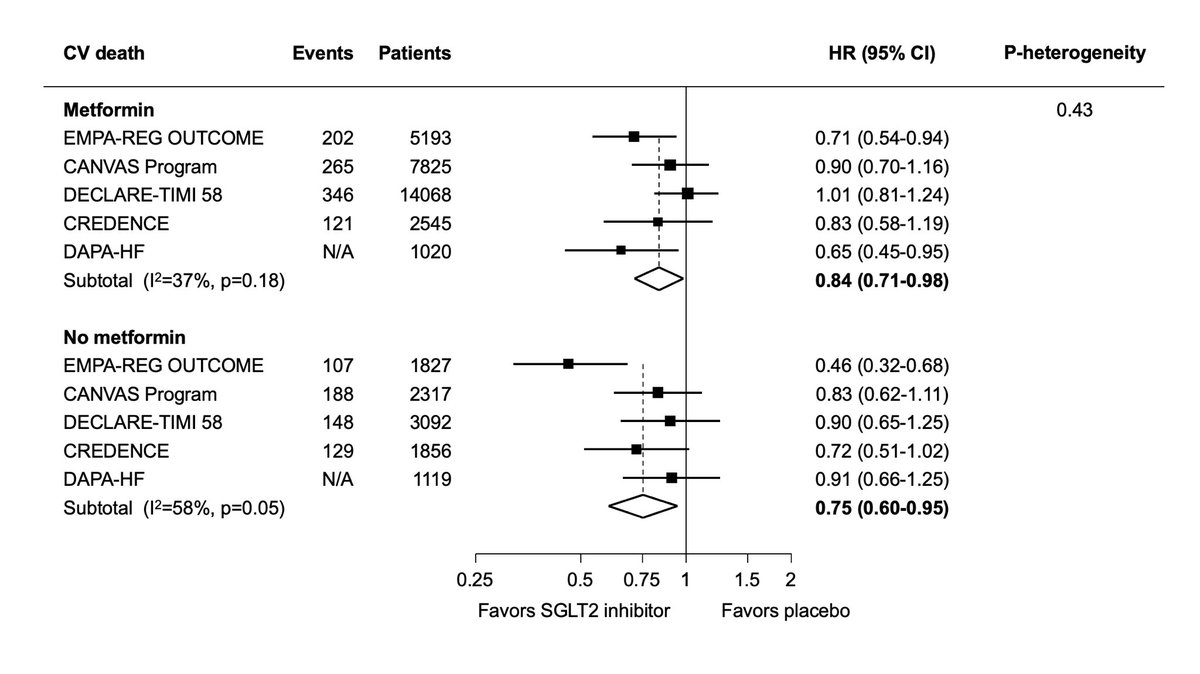
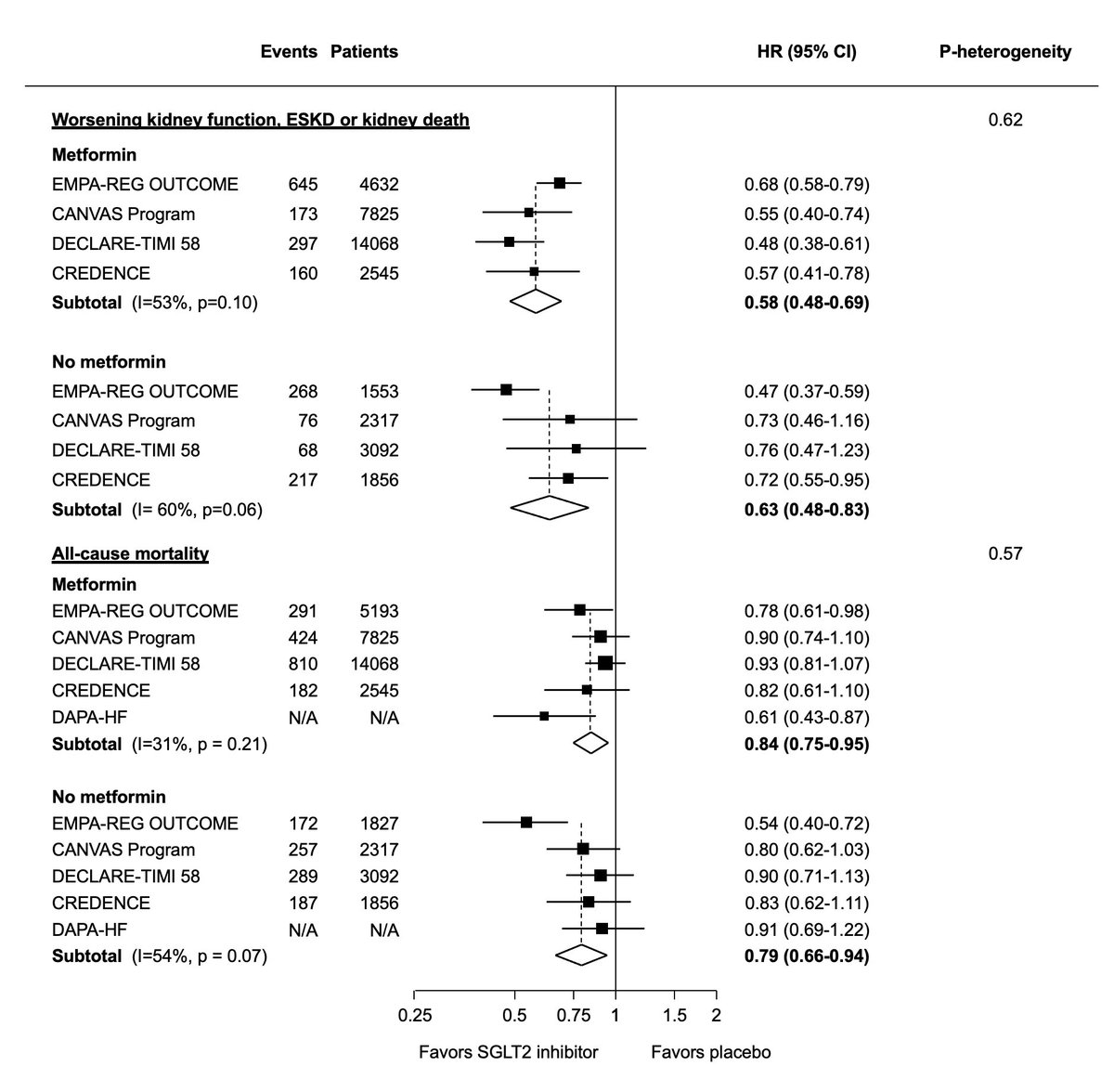
We pooled data from the CVOTs, CREDENCE and DAPA-HF in this meta-analysis https://dom-pubs.onlinelibrary.wiley.com/doi/abs/10.1111/dom.14226">https://dom-pubs.onlinelibrary.wiley.com/doi/abs/1...
We pooled data from the CVOTs, CREDENCE and DAPA-HF in this meta-analysis https://dom-pubs.onlinelibrary.wiley.com/doi/abs/10.1111/dom.14226">https://dom-pubs.onlinelibrary.wiley.com/doi/abs/1...
We found that treatment with SGLT2 inhibitors resulted in clear and consistent reductions in MACE, heart failure or CV death, heart failure alone, and CV death, regardless of metformin use
SGLT2 inhibitors also reduced the risk of worsening kidney function, kidney failure or death due to kidney disease, as well as all-cause death, irrespective of metformin use
These data do not directly address the question of 1st line treatment in ppl with early T2DM - most ppl not on metformin in these trials had a long duration of diabetes with substantial proportion on insulin.
Ongoing trials may provide some guidance https://clinicaltrials.gov/ct2/show/NCT03982381?term=NCT03982381&draw=2&rank=1">https://clinicaltrials.gov/ct2/show/...
Ongoing trials may provide some guidance https://clinicaltrials.gov/ct2/show/NCT03982381?term=NCT03982381&draw=2&rank=1">https://clinicaltrials.gov/ct2/show/...
Accepting these limitations, these data call into question current recommendations that SGLT2i be added only when insufficient glucose control is achieved on metformin and provide empirical support for the ESC guidelines
As Prof Drucker states here - is it time to reconsider the idea of universal 1st line treatment for all patients when we have clear outcome data for preventing specific complications? Are we doing more harm than good with such a rigid approach? https://twitter.com/danieljdrucker/status/1071445827913203712">https://twitter.com/danieljdr...

 Read on Twitter
Read on Twitter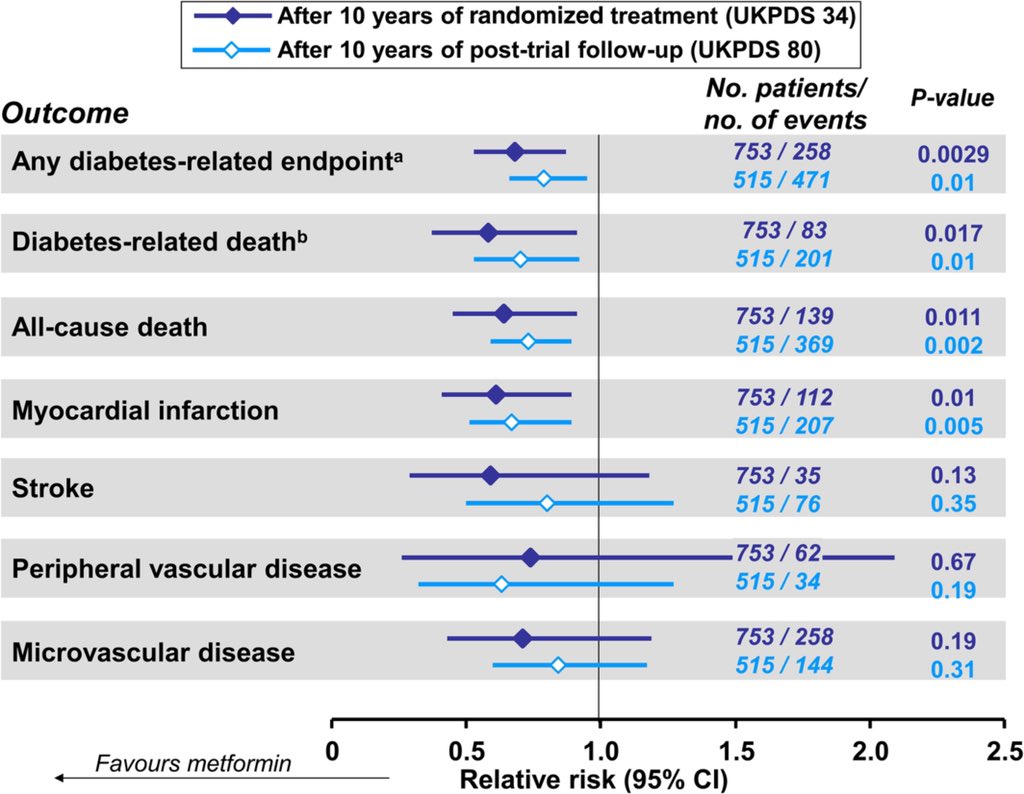 risk of MI and mortality over ~10y follow up" title="Metformin is cheap, well tolerated, effective at lowering glucose & has been used for decades.The main randomised evidence for its CV benefits comes from 1709 obese individuals in the UKPDS trial, where metformin https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> risk of MI and mortality over ~10y follow up" class="img-responsive" style="max-width:100%;"/>
risk of MI and mortality over ~10y follow up" title="Metformin is cheap, well tolerated, effective at lowering glucose & has been used for decades.The main randomised evidence for its CV benefits comes from 1709 obese individuals in the UKPDS trial, where metformin https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> risk of MI and mortality over ~10y follow up" class="img-responsive" style="max-width:100%;"/>