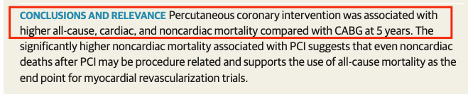
1/ Cherry-picking by Meta-analysis: In a meta-analysis of 23 randomized trials comparing PCI vs. CABG, “Percutaneous coronary intervention was associated with higher all-cause, cardiac, and noncardiac mortality compared with CABG at 5 years”. https://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2771668">https://jamanetwork.com/journals/...
@mmamas1973 @GreggWStone @JAMAInternalMed @DFCapodanno @MaartenvSmeden @vlgmrc @Drroxmehran @SVRaoMD @DrMarthaGulati @mikejohansenmd @drjohnm @ProfDFrancis #cardiotwitter #RadialFirst @boback @SABOURETCardio @djc795 @ShelleyWood2 @mirvatalasnag @Radial_ICG @CardioIAN
@PCRonline @TCTMD @TCTConference @AHAMeetings @escardio @ESC_Journals @SCAI @sbrugaletta @thiele_holger @evandrofilhobr @lamelaspablo @GoranEBC @HadyLichaaMD @Costa_F_8 @g_giustinoMD @CMichaelGibson @chadialraies @fischman_david @rajivxgulati @drandrewsharp @GGStefanini @espogiov
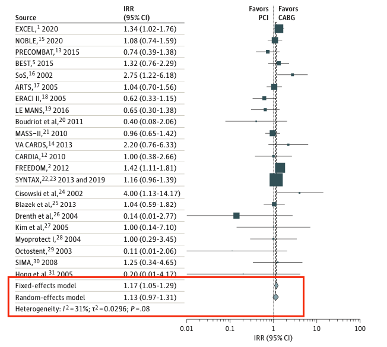
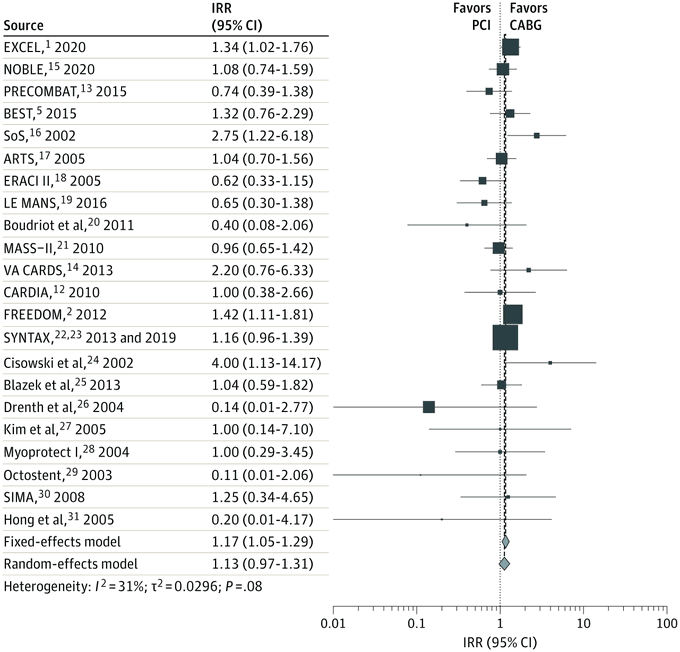
2/ There was a higher risk of all-cause death with the fixed-effect meta-analysis among patients randomized to PCI vs. CABG (IRR 1.17, 95%CI 1.05-1.29). However, random effects meta-analysis showed no evidence for increased risk of mortality with PCI (IRR 1.13, 95%CI 0.97-1.31).
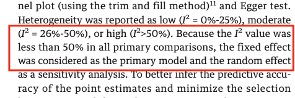
3/ How did the authors decide to use a fixed-effect model (which incidentally favored CABG over PCI)? Apparently, they used the fixed-effect model because heterogeneity was low.
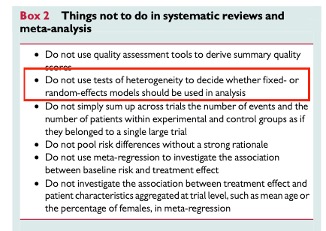
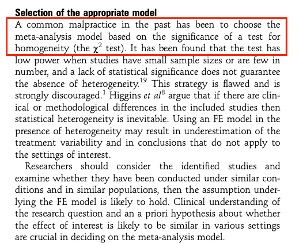
4/ However, the practice of using tests of heterogeneity to decide whether a fixed-effect or random effects model should be used is strongly discouraged in meta-analyses ( https://academic.oup.com/eurheartj/article/35/47/3336/2293217)">https://academic.oup.com/eurheartj...
5/ This is just another article discouraging the use the fixed-effect vs. random effects based on a significance of a test for homogeneity by @Geointheworld and @dimi_mavridis ( https://ebmh.bmj.com/content/17/2/53 )">https://ebmh.bmj.com/content/1...
6/ “Rather, reviewers should decide a priori which model to use […], with the understanding that random-effects models will only be truly more conservative than fixed-effect models if statistical heterogeneity is present and small-study effects absent”. ( https://academic.oup.com/eurheartj/article/35/47/3336/2293217)">https://academic.oup.com/eurheartj...
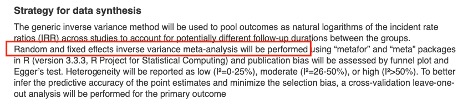
7/ However, what did the authors specify in their protocol registered on PROSPERO? (available at: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=165349)">https://www.crd.york.ac.uk/PROSPERO/... They did not specify at all which model would have been used. If anything, random effects model was reported as first model to be used.
8/ As the included trials were conducted over 20 years and included different populations with different conditions (see for example FREEDOM only in patients with diabetes, trials performed only in patients with LMD), a random effects model should have been used.
9/ Readers should carefully interpret the conclusions of this meta-analysis and should rather consider the results from the random effects model to guide their decision-making in clinical practice. @JAMAInternalMed https://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2771668">https://jamanetwork.com/journals/...

 Read on Twitter
Read on Twitter