Don& #39;t miss cardiogenic shock in the ED!
High mortality that increases when diagnosis is delayed
Use careful exam, labs, ECG and POCUS to dx
A few tips from our recent paper Madison Daly @long_brit @EMHighAK @UVMEmergencyMed
#foamcc #FOAMed
https://www.ajemjournal.com/article/S0735-6757(20)30839-1/pdf">https://www.ajemjournal.com/article/S...
High mortality that increases when diagnosis is delayed
Use careful exam, labs, ECG and POCUS to dx
A few tips from our recent paper Madison Daly @long_brit @EMHighAK @UVMEmergencyMed
#foamcc #FOAMed
https://www.ajemjournal.com/article/S0735-6757(20)30839-1/pdf">https://www.ajemjournal.com/article/S...
Avoid the "everything is Sepsis" trap!
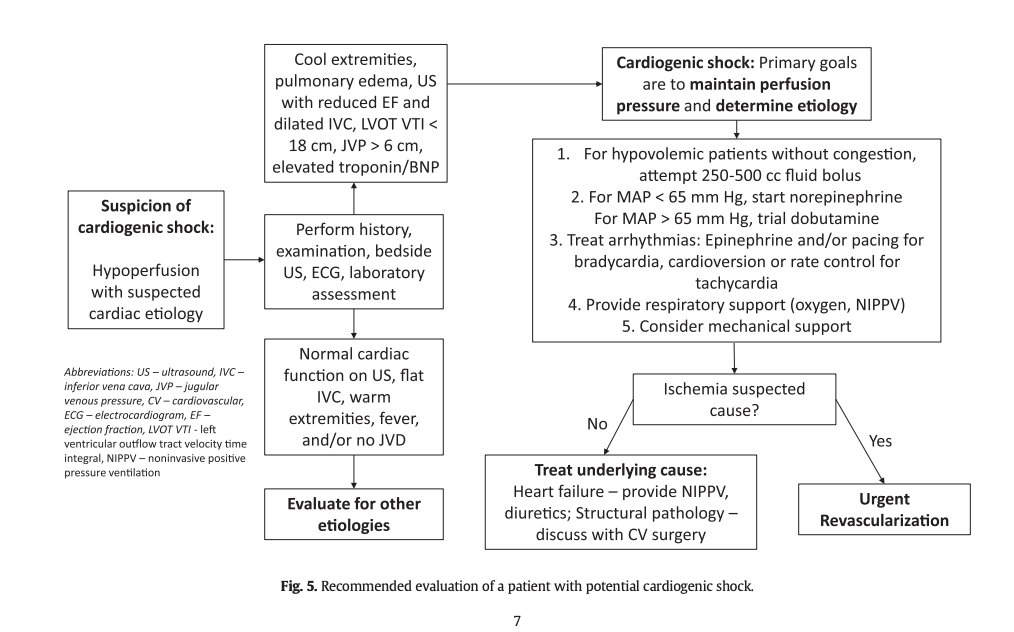
Examine for signs of Cardiogenic Cause:
1. Hypoperfusion: cool extremities, AMS, oliguria, etc.
2. Congestion: elevated JVP or JVD, pulmonary edema, etc
3. Vitals: narrow pulse pressure, > 5% may not have hypotension
4. New murmur? S3?
Examine for signs of Cardiogenic Cause:
1. Hypoperfusion: cool extremities, AMS, oliguria, etc.
2. Congestion: elevated JVP or JVD, pulmonary edema, etc
3. Vitals: narrow pulse pressure, > 5% may not have hypotension
4. New murmur? S3?
Get an ECG! (MI most common cause)
Labs: Lactate elevation, AKI, troponin, SCVO2 low
POCUS for LVEF (mean 30% EF in CS), IVC, RV function, estimate CO (LVOT VTI), pulm edema (better than CXR)
Labs: Lactate elevation, AKI, troponin, SCVO2 low
POCUS for LVEF (mean 30% EF in CS), IVC, RV function, estimate CO (LVOT VTI), pulm edema (better than CXR)
Stabilize:
Avoid med iatrogenesis (BB, CCB, excess fluids)
No congestion on exam? Consider small (250-500 ml) fluid boluses
Start norepinephrine to MAP ~ >65 (18% have inappropriately low SVR)
Add dobutamine if hypoperfusion still exists
Treat underlying causes MI?-> cath lab
Avoid med iatrogenesis (BB, CCB, excess fluids)
No congestion on exam? Consider small (250-500 ml) fluid boluses
Start norepinephrine to MAP ~ >65 (18% have inappropriately low SVR)
Add dobutamine if hypoperfusion still exists
Treat underlying causes MI?-> cath lab
Nice skin mottling images from a very relevant case report of cardiogenic shock in @NEJM
If you see this check the heart!
Skin Mottling | NEJM https://www.nejm.org/doi/full/10.1056/NEJMicm1602055#.X4dXXW8Xncg.twitter">https://www.nejm.org/doi/full/...
If you see this check the heart!
Skin Mottling | NEJM https://www.nejm.org/doi/full/10.1056/NEJMicm1602055#.X4dXXW8Xncg.twitter">https://www.nejm.org/doi/full/...

 Read on Twitter
Read on Twitter