Back to #pulmonology quick hits! Today I& #39;ll present a schema for the  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🗣️" title="Silhouette eines sprechenden Kopfes" aria-label="Emoji: Silhouette eines sprechenden Kopfes"> PULM MANIFESTATIONS OF LUPUS
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🗣️" title="Silhouette eines sprechenden Kopfes" aria-label="Emoji: Silhouette eines sprechenden Kopfes"> PULM MANIFESTATIONS OF LUPUS  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🗣️" title="Silhouette eines sprechenden Kopfes" aria-label="Emoji: Silhouette eines sprechenden Kopfes"> – all info from #H402634822">https://www.uptodate.com/contents/pulmonary-manifestations-of-systemic-lupus-erythematosus-in-adults #H402634822">https://www.uptodate.com/contents/...
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🗣️" title="Silhouette eines sprechenden Kopfes" aria-label="Emoji: Silhouette eines sprechenden Kopfes"> – all info from #H402634822">https://www.uptodate.com/contents/pulmonary-manifestations-of-systemic-lupus-erythematosus-in-adults #H402634822">https://www.uptodate.com/contents/...
First, consider if pulmonary symptoms may be due to INFECTION or CHEST WALL PAIN. Chest wall pain has a high base rate, so don& #39;t forget to palpate that chest wall & think of superficial MSK causes as a quick rule-out.
We must consider infxn in SLE due to disease itself (low complements + lymphopenia) & infxn due to immunosuppressive therapies. Standard w/u may include RPP, atypical pneumonia serologies, & urinary antigens. If immunosuppressed, consider opportunistic infxn testing (eg PJP).
Next, consider the CHRONICITY of symptoms. If ACUTE, think pleuritis, thromboembolism, acute pneumonitis, & DAH.
Pleuritis is common and generally associated with small effusions if present. This may be eventually complicated by fibrothorax w/ Trapped Lung Syndrome. https://www.nejm.org/doi/full/10.1056/nejmicm1404964">https://www.nejm.org/doi/full/...
Thromboembolism may be associated with antiphospholipid antibodies or SLE complicated by nephrotic syndrome. (Think, does the patient have a red leg?)
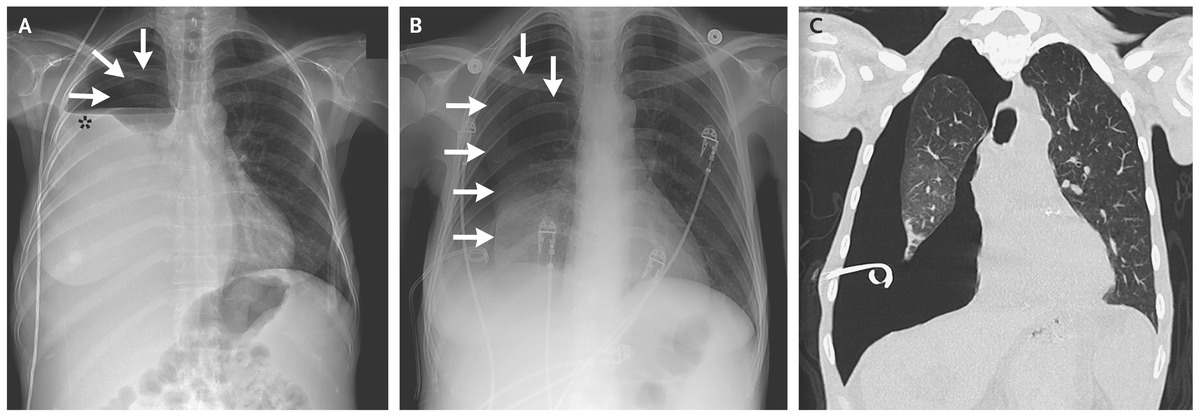
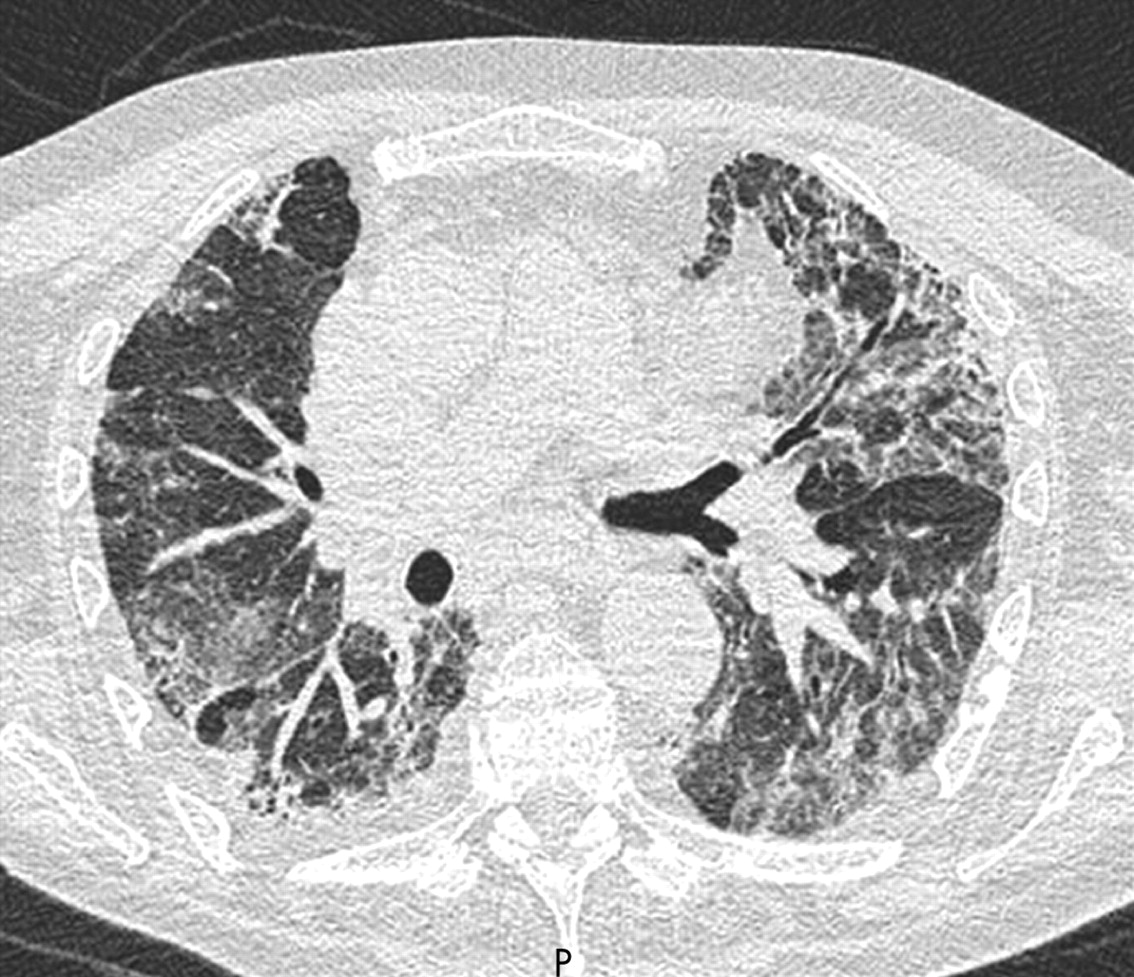
Acute pneumonitis & Diffuse Alveolar Hemorrhage (DAH) are rare. DAH patients appear acutely ill and report dyspnea, cough, & hemoptysis usually developing over 3 days, w/ hemoptysis eventually occurring in a majority.
The hemorrhage of DAH is related to bland hemorrhage & immune complex-mediated capillaritis. However, fever is inconsistent and occurs in only 25%.
Patients w/ Acute Pneumonitis (AP) present w/ rapid-onset fever, cough/hemoptysis, & dyspnea. This is really a diagnosis of exclusion. Since DAH & AP are difficult to distinguish in practice, BAL is helpful for both ruling-out infxn & DAH.
If symptoms are CHRONIC, think pulmonary HTN, ILD, & Shrinking Lung Syndrome.
Pulmonary HTN in lupus can be due to a variety of causes. (Think of the WHO Classification of etiologies.) The PAH-like phenotype in lupus is pathologically similar to ordinary PAH, but w/ complement & immunoglobulin deposition in pulmonary arterial walls.
ILD is rare and actually the least common rheum-associated ILD. (Scleroderma is the most common.) Manifestations on imaging are protean but the most common pattern is NSIP (nonspecific interstitial pneumonia). https://thorax.bmj.com/content/62/11/1008">https://thorax.bmj.com/content/6...
Shrinking Lung Syndrome is very rare (1-6%) but presents w/ episodes of pleuritic chest pain (65%), dyspnea, & progressive decreases in lung volumes & DLCO. Characteristically, no evidence of interstitial/pleural disease on imaging.
For more on Shrinking Lung Syndrome, see this great thread by @nickmmark https://twitter.com/nickmmark/status/1286705496221597696?s=20">https://twitter.com/nickmmark...

 Read on Twitter
Read on Twitter