PSA: We (STILL) have no data to know the pattern of viral loads over time from infection to recovery. So we don& #39;t know how test sensitivity & infectiousness correlate.
Tons of stories w/ quotes from top people are not making this clear & it matters.
Clarifying thread
Tons of stories w/ quotes from top people are not making this clear & it matters.
Clarifying thread
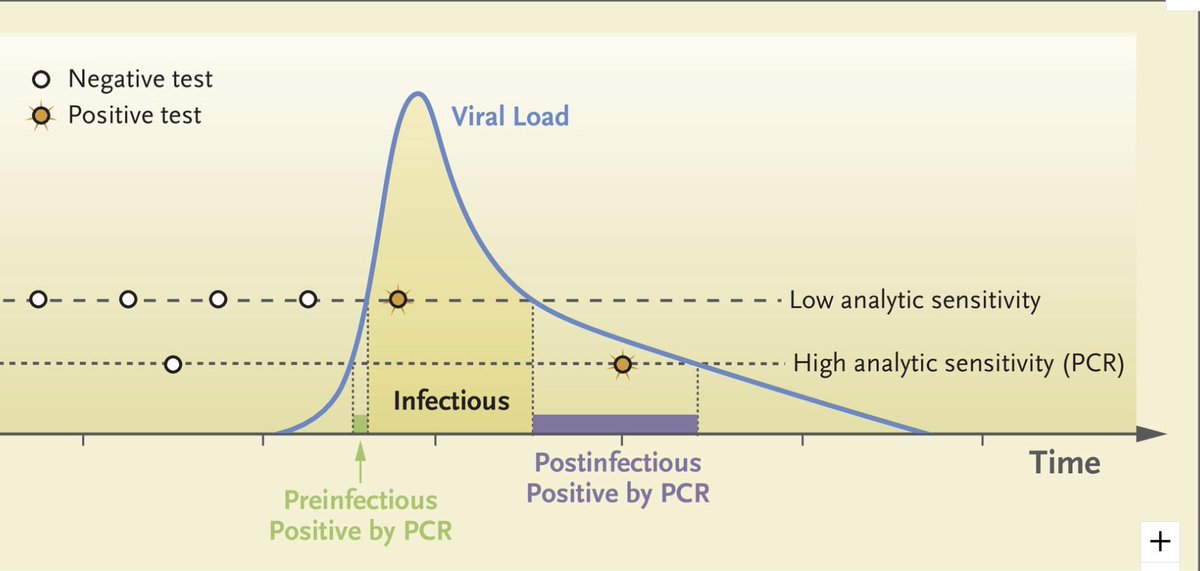
You may have seen this figures showing viral load over time, with thresholds for testing +.
(This one from @michaelmina_lab @DanLarremore paper). Simple & straightforward, right?
Conceptually yes, but what is this figure based on? Is it SARS-CoV-2/COVID-19 data in people? Nope!
(This one from @michaelmina_lab @DanLarremore paper). Simple & straightforward, right?
Conceptually yes, but what is this figure based on? Is it SARS-CoV-2/COVID-19 data in people? Nope!
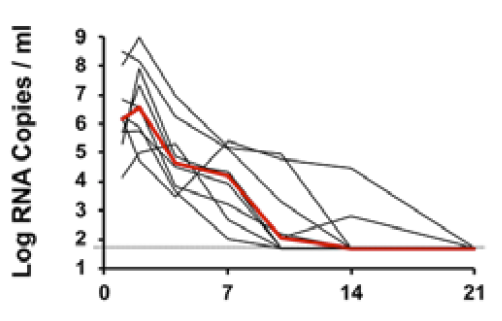
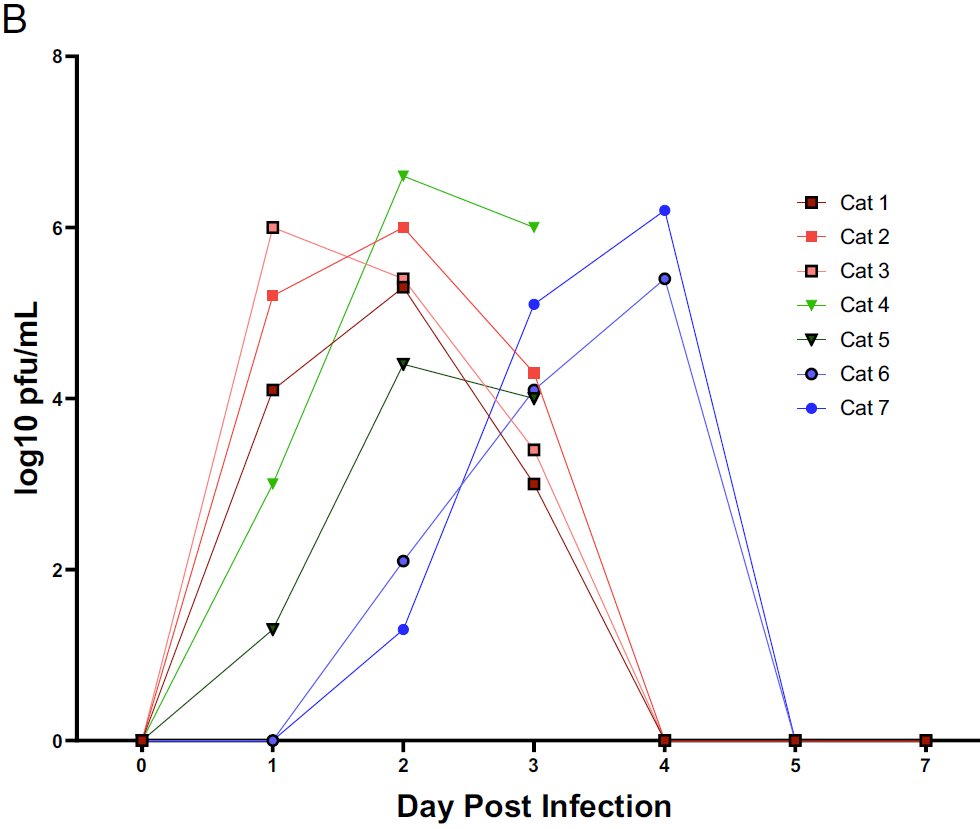
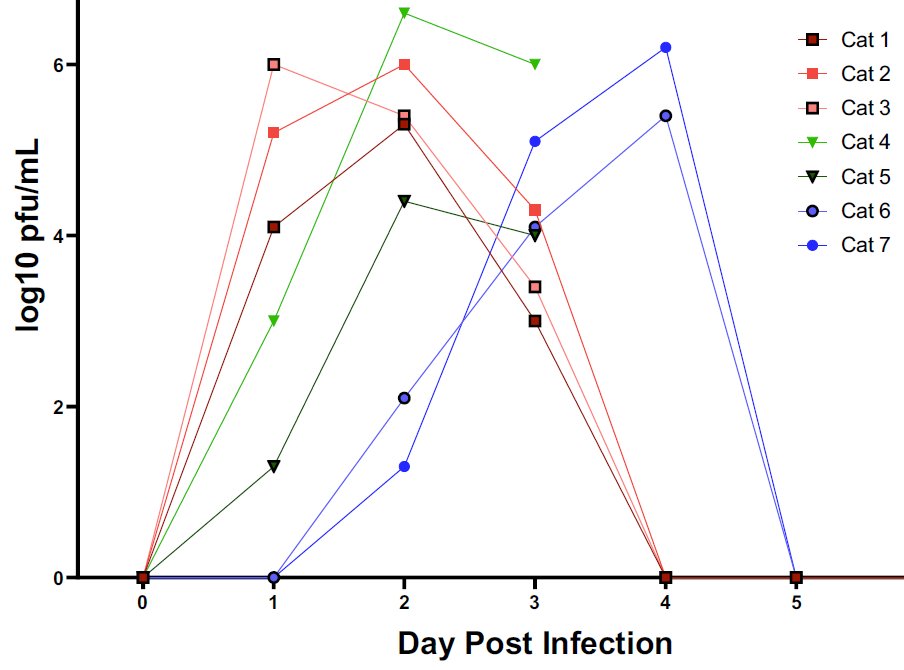
This figure is (loosely) based on data from other viruses in people & SARS-CoV-2 in animals. Here& #39;s data from macaques (10.1126/science.abc4776) & cats ( http://www.pnas.org/cgi/doi/10.1073/pnas.2013102117).">https://www.pnas.org/cgi/doi/1... Looks similar to schematic but not quite identical. Where is the virus-negative period pre-peak?
It& #39;s often NOT present in animals b/c dose we give animals is often very high & probably much higher than most humans get exposed to. In transmission studies (sometimes still w/ very high exposure) we *sometimes* see short period w/out detectable virus...
It& #39;s present on days 0&1 for 2 cats infected by contact (6&7) http://www.pnas.org/cgi/doi/10.1073/pnas.2013102117">https://www.pnas.org/cgi/doi/1...
But it was not present in this study in contact-infected golden hamsters ( https://www.nature.com/articles/s41586-020-2342-5).">https://www.nature.com/articles/... Virus was detectable on day 1 post contact.
So what? Why am I making a big deal out of this?
Because the efficacy of testing to identify people that are infected & infectious depends critically on when a person becomes infectious relative to when they test positive.
Because the efficacy of testing to identify people that are infected & infectious depends critically on when a person becomes infectious relative to when they test positive.
Here& #39;s what we assume vs what we know:
- We assume that if you are infectious you would test positive. Sounds reasonable, right? But where is the data to back that up? It doesn& #39;t exist. Hard (but not impossible) to collect especially if we measure transmission Y/N to animal.
- We assume that if you are infectious you would test positive. Sounds reasonable, right? But where is the data to back that up? It doesn& #39;t exist. Hard (but not impossible) to collect especially if we measure transmission Y/N to animal.
I believe @javid_lab proposed experiment for another purpose (aerosol?) but it would work great for this Q too: take recent contacts of a case & swab each day and put animal (golden hamster?) in room w/ patient. See when swab vs hamster is +. Not trivial but possible.
- We assume that if you have higher viral loads you& #39;re more likely to transmit. Again, likely, but no data to support this. Why? Again, hard experiment w/ people (but this study in HCW could have done it, but didn& #39;t: https://twitter.com/DiseaseEcology/status/1283894370869981185).">https://twitter.com/DiseaseEc... But w/ animals (see above).
So where does this put us & were WH, Trump family & attendees of ACB confirmation, presidential debate dumb to think they were safe w/out masks if everyone had been tested & was negative?
It depends on probability of test correctly identifying people when they are infectious at time of test & time b/w test and contact. If swab&test correctly ID ALL infectious people & are done at time of (short) contact then WH, Trump, rose garden attendees were NOT dumb.
But we don& #39;t actually know this probability, at all, & that& #39;s a major problem. We think we do, but we don& #39;t. Here& #39;s why.
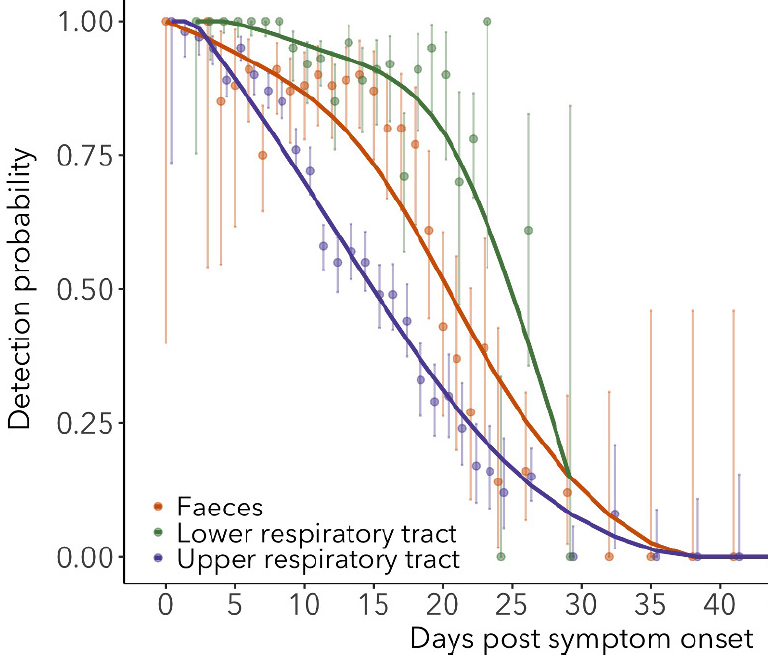
We now have lots of data on the chance of testing + AFTER symptom onset. But on day of onset data v limited (see big day 0 error bar).
https://doi.org/10.7554/eLife.60122">https://doi.org/10.7554/e...
We now have lots of data on the chance of testing + AFTER symptom onset. But on day of onset data v limited (see big day 0 error bar).
https://doi.org/10.7554/eLife.60122">https://doi.org/10.7554/e...
Recent paper by Zhen Zhang @QifangB @JustinLessler @andrewazman very cleverly use antibody testing of PCR - contacts of cases to see how often tests miss infection ( https://doi.org/10.1101/2020.09.01.20182469).">https://doi.org/10.1101/2... Unfortunately, again, almost no data pre-symptom onset (N=7 swabs from ? patients).
Also, prob of detecting RNA on early days post-infection very different between 2 papers (that& #39;s a subject for a whole different thread).
@bennyborremans @jlloydsmith @JustinLessler
@bennyborremans @jlloydsmith @JustinLessler
Key point: we still have almost 0 data on what a neg test means pre-symptom onset for finding infection. I& #39;ve been writing about this June & begging people to collect data (which isn& #39;t hard-just repeated swabs from recent contacts of cases) https://twitter.com/DiseaseEcology/status/1270093309126438912">https://twitter.com/DiseaseEc...
I contributed to an article @sarahzhang wrote about it in Atlantic: https://www.theatlantic.com/science/archive/2020/06/how-negative-covid-19-test-can-mislead/613246/">https://www.theatlantic.com/science/a...
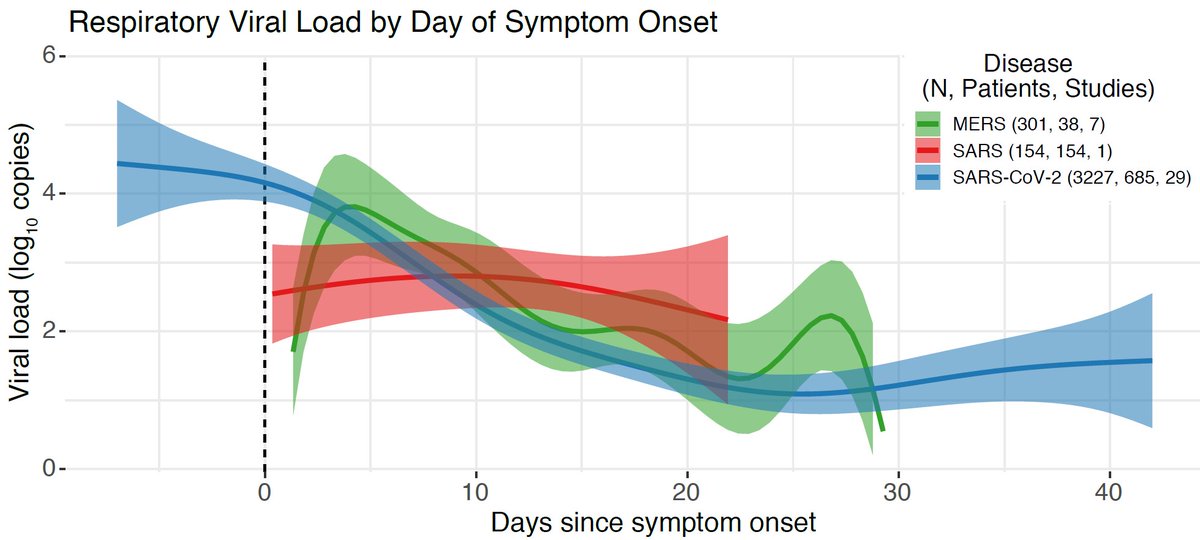
What do we know about infectiousness & viral loads vs time since infection? Recent preprint by Amy Bennefield @BMAlthouse suggests loads higher pre-symptom onset ( https://doi.org/10.1101/2020.09.28.20202028).">https://doi.org/10.1101/2... Paper has issues (need whole new thread) but general trend likely correct.
But where is period of 0 viral load & rise like in early tweet in this thread & in 2 cats? It& #39;s not there b/c no data early enough!
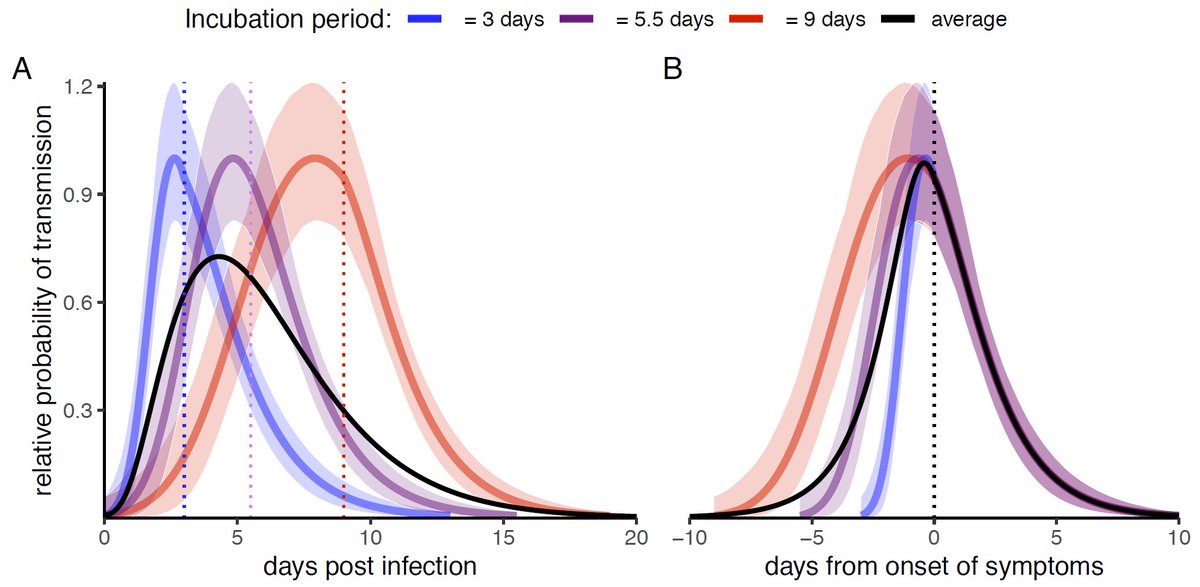
What about infectiousness? Our recent paper w/ @LucaFerrettiEvo @ChristoPhraser @JoannaMasel @ChrisWymant using infector-infectee pairs w/ known exposure time suggests infectious period starts earlier relative to symptoms if incubation period is longer.
https://www.medrxiv.org/content/10.1101/2020.09.04.20188516v2">https://www.medrxiv.org/content/1...
https://www.medrxiv.org/content/10.1101/2020.09.04.20188516v2">https://www.medrxiv.org/content/1...
Put another way, infectiousness rises quickly if short incubation period & slower if incub period is longer, but unfortunately, data aren& #39;t rich enough to carefully describe infectiousness on each day post-infection.
For more details on how long you are infectious & translating RNA into infectious virus see: https://twitter.com/DiseaseEcology/status/1271281847754846211">https://twitter.com/DiseaseEc...
Thus, we currently CANNOT know whether you will test + if you are infectious (more accurately, what is sensitivity vs prob of transmitting given contact). All we can say is that you are more likely to test + if viral load is higher (simple molecular diagnostics)
And, if viral load is higher you *probably* are more infectious (but flu @Don_Milton @bencowling88 study showed very poor correlation (R2<8.5%) b/w NP swab & aerosol load doi:10.1371/journal.ppat.1003205).
What this means is that we do NOT have data to know whether a negative test means you are aren& #39;t infectious. One should NOT assume a negative test means your are not infected or infectious.
(cont)
(cont)
It sounds like attendees of rose garden ACB nomination (WH, Trump family, etc.) were told it was ok to take off masks b/c everyone present had tested negative.
I don’t know who made the decision to tell people this falsehood, but they are partly at fault for any transmission that occurred at the event. It is the people that made this claim that are dumb.
One would think that the white house (& senators) could ask one of the world’s experts (or me!) what they can conclude from a test & if it’s safe to not wear masks if everyone is being tested. They clearly didn’t & it’s not.
In case anyone is wondering what utility testing is if it can’t always correctly identify people as infectious or not, @michaelmina has a thread about it. https://twitter.com/michaelmina_lab/status/1312490467657838593">https://twitter.com/michaelmi...
tl;dr tests can ID a large fraction (but probably not 100%) of infectious people so they can isolate (as Trump, FLOTUS, etc. are doing now) & reduce onward spread. https://twitter.com/michaelmina_lab/status/1312490467657838593">https://twitter.com/michaelmi...
So, if whole US pop had access to cheap rapid tests (w/ high specificity or rapid confirmation test) then it would NOT mean we could immediately return to mask-less social interactions safely.
It would mean we could use testing to greatly reduce levels of infection so that probability of each person being infected was low. In best case, we get to New Zealand/Vietnam status where there is almost zero infection & we can have bars, parties, big sports events, etc.
But we’d need to bring infection to low levels 1st, not restart those activities just because everyone could test themselves. If we did that we’d get the white-house debacle we have now on a massive scale.
Which is the same reason why Hawaii and other places’ decisions to replace quarantine w/ a single negative test is a poor idea:
https://twitter.com/DiseaseEcology/status/1276023991870709761
https://twitter.com/DiseaseEc... href=" https://www.cnn.com/travel/article/hawaii-reopening-october-15-covid-19/index.html">https://www.cnn.com/travel/ar...
https://twitter.com/DiseaseEcology/status/1276023991870709761

 Read on Twitter
Read on Twitter