1/ Today is Yom Kippur. Many Jewish people are fasting. I am not
But I still want to talk about fasting…
But I still want to talk about fasting…
2/ Today we are finally publishing the results of a study on Time Restricted Eating (TRE), which is a form of intermittent fasting. The study is called the TREAT Study. More on that later…
3/ It is the culmination of 7+ years of interest in this topic that started with the publication of some fascinating papers from @SatchinPanda describing the benefits of time restricted feeding (TRF) in mice
4/ This work caught my attention then https://twitter.com/ethanjweiss/status/407730451353059328?s=20
And">https://twitter.com/ethanjwei... again https://twitter.com/ethanjweiss/status/539875628045328384?s=20
By">https://twitter.com/ethanjwei... then, I had started doing 16:8 TRE. What did that mean?
Simple: eat whatever you want between 12PM & 8PM (8 hours) & then fast from 8PM-12PM the next day (16 hours). Repeat...
And">https://twitter.com/ethanjwei... again https://twitter.com/ethanjweiss/status/539875628045328384?s=20
By">https://twitter.com/ethanjwei... then, I had started doing 16:8 TRE. What did that mean?
Simple: eat whatever you want between 12PM & 8PM (8 hours) & then fast from 8PM-12PM the next day (16 hours). Repeat...
5/ And by this time, TRE/TRF had hit the mainstream https://twitter.com/ethanjweiss/status/555742574581792768?s=20
But">https://twitter.com/ethanjwei... there had as yet not been a trial in people, and we all know how similar mouse metabolism is to human metabolism
But">https://twitter.com/ethanjwei... there had as yet not been a trial in people, and we all know how similar mouse metabolism is to human metabolism
6/ So while I was doing this myself, and while I was even recommending it to some of my patients, I remained uneasy given the lack of data in humans
Ultimately, we decided to do something we did not do a lot. We decided to do a human clinical trial (on time restricted eating)
Ultimately, we decided to do something we did not do a lot. We decided to do a human clinical trial (on time restricted eating)
7/ It was at this point that @Dy1anLowe entered the story. Dylan was a Ph.D. candidate in the @UCSF BMS Graduate Program. Dylan came to UCSF to work on metabolism – in mice. He had done a rotation in my lab back when he got here but ultimately ended up in a different lab
8/ A few years into his Ph.D., Dylan came to me to tell me he was leaving graduate school. I asked him why. He said because he wanted to work more directly on clinical projects. I encouraged him to take his time making that decision
9/ Eventually, when I was convinced he was serious about leaving, I told him about the fasting project (idea) and asked him if he would consider coming to my lab to run it and finish his Ph.D. Dylan had zero experience with clinical research
10/ Long story short, Dylan joined the group to lead the TREAT Study. To say he was fundamental in the design, implementation and completion of the study would be a dramatic understatement. He was the study. Also...
11/ We designed it with a tremendous amount of help from @eureka_platform and with generous support from @UCSFCardiology and the CVRI among others
12/ From the beginning, we wanted to test a real world and simple prescription. One of the most attractive things about TRE was that it was easy to do. Anyone can do it. There is nothing complicated about it
13/ TRE had tremendous promise to offer a simple and effective method to lose weight and improve metabolic health. We chose to do it this way since this is how diets work in the real-world
14/ What about the eating window? We chose the 12P-8P because that is what seemed to fit best with how we live our lives. I.e. dinner is a much more social meal than breakfast. We assumed that people would have a harder time fasting through dinner
15/ In the end, we were aligned in the mission to do a rigorous and randomized clinical trial. By the time we started, there had been hints of benefit in small and uncontrolled trials of TRE in people
16/ We also wanted the people randomized to the “control” arm to feel like they were getting an intervention too, so we used some creative language and landed on TRE versus continuous meal timing (CMT)
17/ We enrolled adults with overweight/obesity who were not already fasting and had been relatively weight-stable. The primary endpoint for the study was weight loss as measured by an at home wireless scale at 12 wks. 50% of the participants were entirely virtual
18/ We also incorporated a detailed in-person metabolic phenotyping protocol for half the participants, all of whom were local. This would permit us to explore some secondary outcomes and begin to think about mechanism
19/ We enrolled/compeletd this trial quickly (about a year) with the incredibly hard work of Dylan and the study team
This morning the paper is finally published! https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/10.1001/jamainternmed.2020.4153?guestAccessKey=444bbcb2-7e13-4dc6-998f-5de5e27aa19e&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=092820">https://jamanetwork.com/journals/...
This morning the paper is finally published! https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/10.1001/jamainternmed.2020.4153?guestAccessKey=444bbcb2-7e13-4dc6-998f-5de5e27aa19e&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=092820">https://jamanetwork.com/journals/...
20/ What did we find? Well, let’s start with the bottom line.
This was a negative study. TRE did not lead to a statistically significant difference in weight loss at 12 weeks.
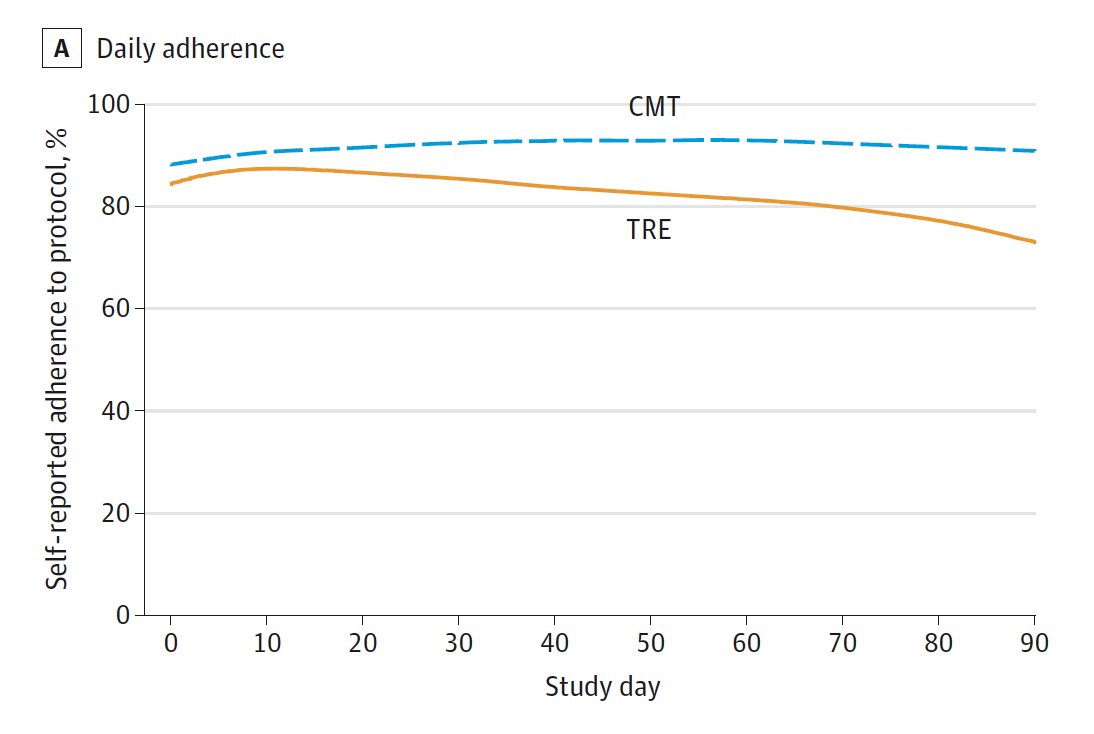
First, the good news. It was relatively easy to comply at least by self-report. So it’s doable
This was a negative study. TRE did not lead to a statistically significant difference in weight loss at 12 weeks.
First, the good news. It was relatively easy to comply at least by self-report. So it’s doable
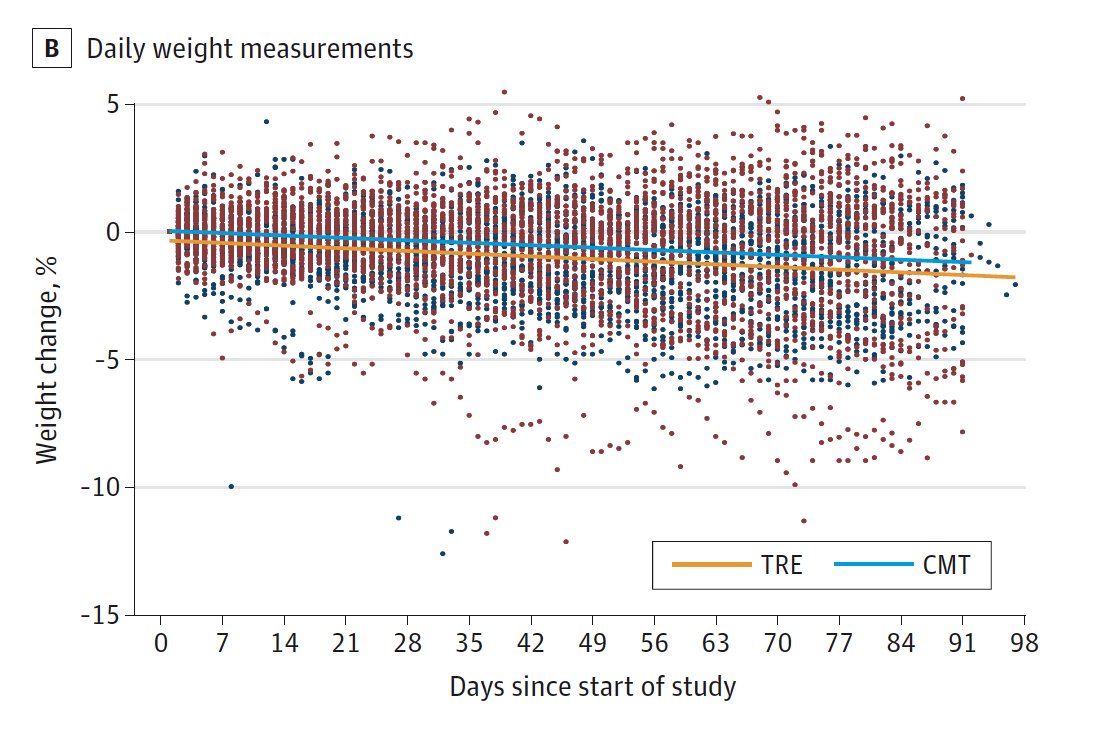
21/ The mean starting weight in both groups was about 100 kg. People in the TRE group lost .94 kg and that was lower than baseline (p = .01). But the CMT group (control) also lost weight (.68 kg). So the between groups differences was not statistically different (p = .63)
22/ This is important. If this had been an uncontrolled study, we& #39;d be saying there was a significant decrease in weight. But there was that pesky control arm. We know that people in clinical trials to lose weight no matter what you do. Including the control arm was important
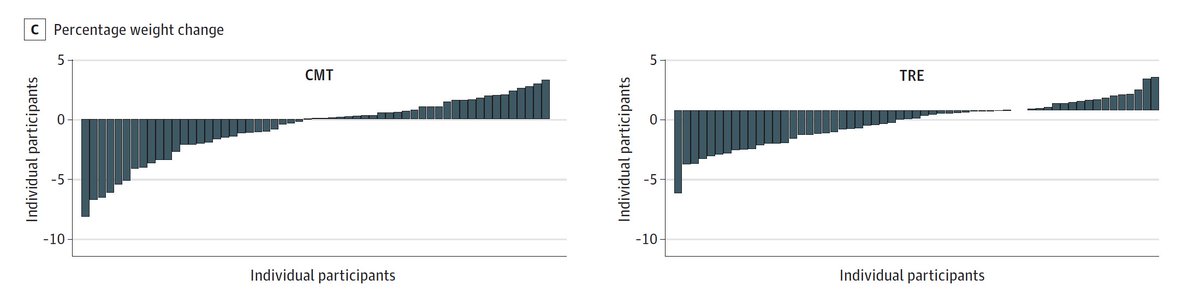
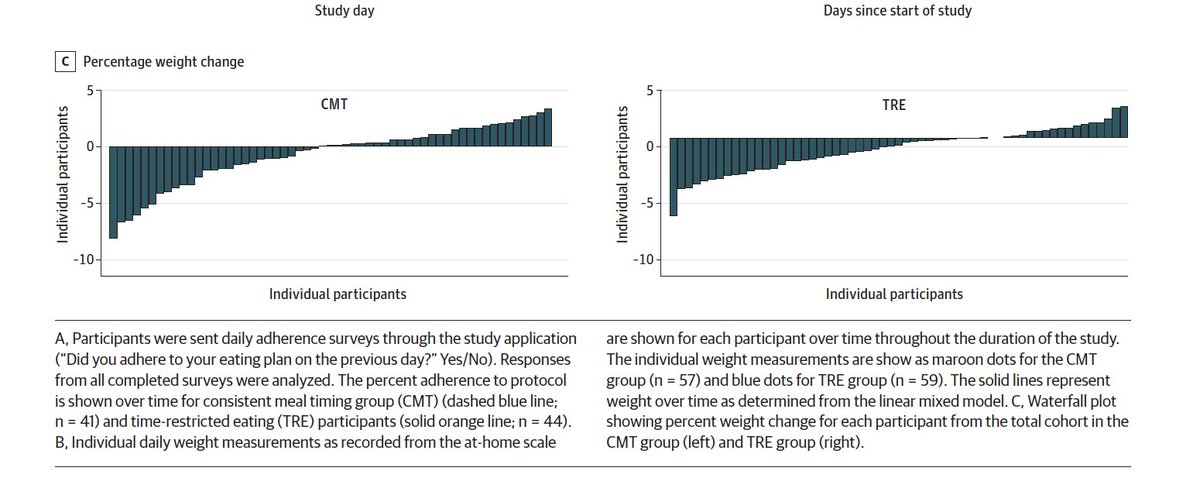
23/ The waterfall plots show the individual weight changes in all the participants from baseline to completion. Here are those plots. There was a balance of people who lost weight & some who gained. The person who lost the most weight was in the CMT group!
24/ If you squint, maybe you can convince yourself more people lost weight in the TRE group, but having squint is never a good thing in science
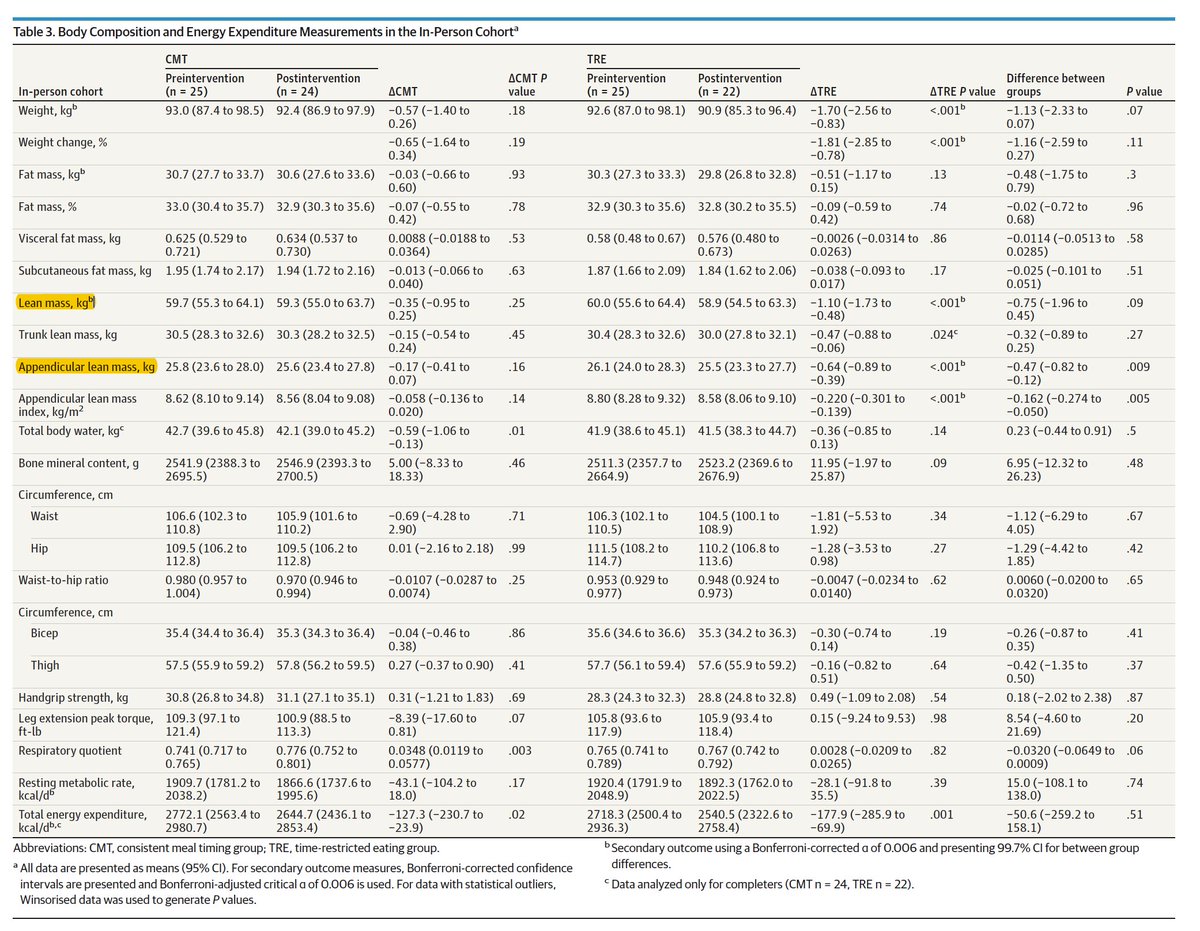
25/ What about the in person stuff. Well, there was basically no difference in any of the things we looked at with one exception (more on that soon). There was no difference in insulin or glucose, lipids, sleep, activity, resting or total energy expenditure, or fat mass
26/ There was one thing that seemed different. This is a secondary endpoint so take it with a grain of salt, but people in the TRE group lost more lean mass (and especially appendicular lean mass) than those in CMT
27/ In the in-person cohort, the average weight loss in the TRE group was 1.70 kg. Of this, 1.10 kg (~ 65% wt lost) was lean mass; only 0.51 kg of weight lost was fat mass. Loss of lean mass during weight loss is normal but typically accounts for 20% to 30% of total weight loss
28/ So in summary: 1) no matter how you slice it, prescription of TRE is not a very effective weight loss strategy; 2) There was no advantage to TRE when compared to a proper control group; 3) What weight was lost looked to come more from muscle mass than fat mass
29/ We were surprised by these results. At that time, I had been doing 16:8 TRE for ~7 years. I stopped. This study taught me a lot. More later but the take home lessons for me are: 1) it is possible to do RCTs in nutrition; 2) ignore all nutrition studies without a control group
30/ 3) focusing just on weight loss may lead one to assume benefit when there could be harm. The lean mass example is a good one. Losing 1 kg of mass =/= a kg of fat. Indeed, if one loses .65 kg of lean mass and only .35 kg fat mass, that is an intervention I’d probably pass on
31/ Lastly, there is so much left to learn here. We are going to stay at it and try to answer some of the obvious next questions. Really this is just the beginning. But again, massive thank you to Dylan who is a star clinical researcher in the making
Postscript. Someone pointed out that there is an issue with one of the figures. The reference line should be zero and it is one on the right side with TRE. I did not notice it in the proofs. We will work with @JAMAInternalMed to get it corrected

 Read on Twitter
Read on Twitter