Okay, I said I& #39;d try my hand at a #tweetorial for #meded so, here goes:
Let& #39;s talk about Lewy Body Dementia (LBD) diagnosis. Management would be another thread. I& #39;ll provide refs as we go and link to some really great tools, and try to tag relevant folks for their work. 1/21 https://twitter.com/RenegadeSynapse/status/1308548679175938048">https://twitter.com/RenegadeS...
Let& #39;s talk about Lewy Body Dementia (LBD) diagnosis. Management would be another thread. I& #39;ll provide refs as we go and link to some really great tools, and try to tag relevant folks for their work. 1/21 https://twitter.com/RenegadeSynapse/status/1308548679175938048">https://twitter.com/RenegadeS...
First, please read Susan Schneider Williams editorial in Neurology about Robin Williams, and strongly encourage you to watch Robin& #39;s Wish on @netflix https://n.neurology.org/content/87/13/1308">https://n.neurology.org/content/8... 2/21
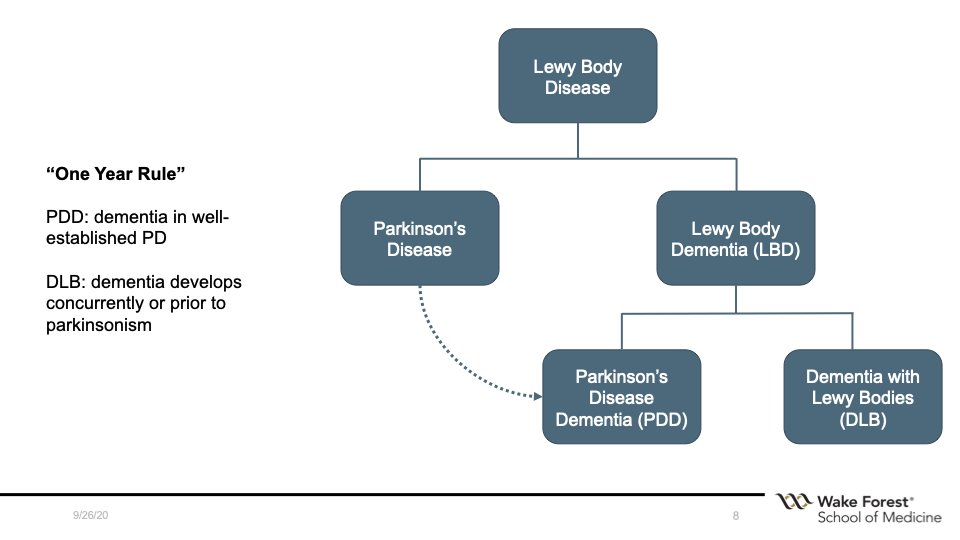
Terminology is confusing: Lewy Body Dementia is best thought of as the supraordinate category made up of PDD and DLB.
If movement problems develop concurrently with dementia or after the dementia (and fits otherwise) then = DLB. In & #39;well-established PD& #39; = PDD. 3/21
If movement problems develop concurrently with dementia or after the dementia (and fits otherwise) then = DLB. In & #39;well-established PD& #39; = PDD. 3/21
@rimonaweil, @a_schrag, @jmschott and colleagues wrote a great review of the PDD/DLB spectrum in 2017, highly recommended reading. https://f1000research.com/articles/6-1604/v1">https://f1000research.com/articles/... 4/21
What increases risk for dementia in PD?
Older, smoking, HTN, male sex, presence of REM behavior disorder, postural instability gait disturbance (PIGD) phenotype. Tremor predominant less likely. 5/21
Older, smoking, HTN, male sex, presence of REM behavior disorder, postural instability gait disturbance (PIGD) phenotype. Tremor predominant less likely. 5/21
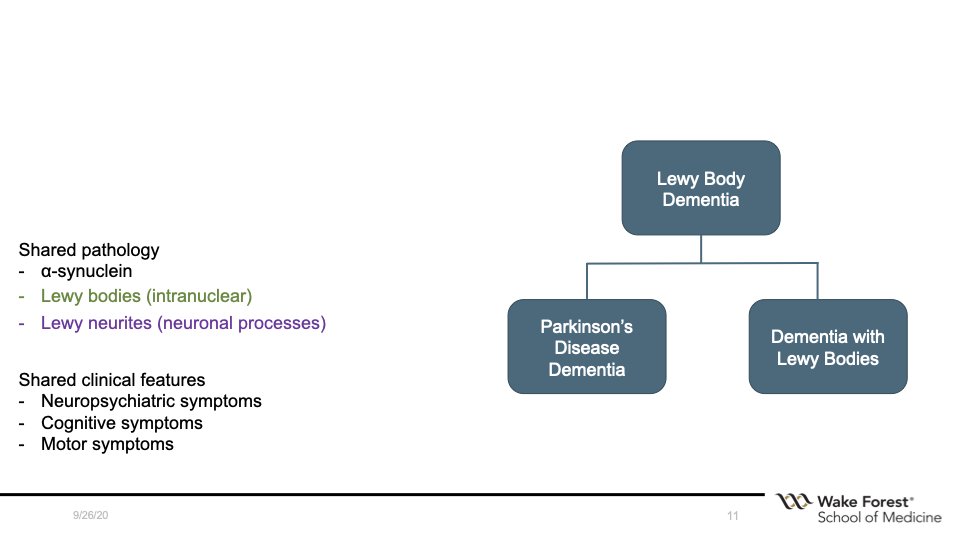
The dementia due to PDD shares a lot of features with DLB, including shared pathology and phenomenology (cognitive, neuropsychiatric, and motor...although the movement usually much more of a problem in PDD). 6/21
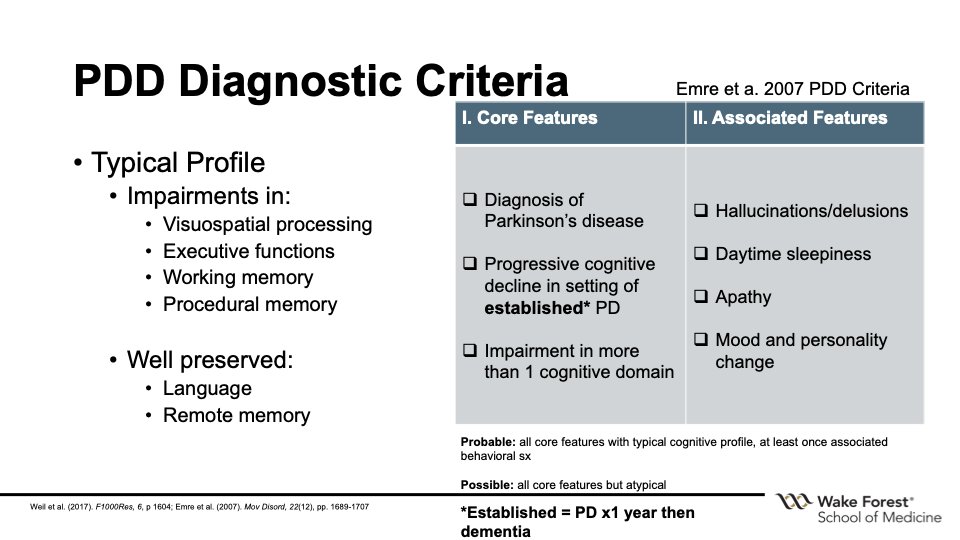
Diagnostic criteria for PDD were published in 2007. Probable if it& #39;s typical and at least one associated feature, possible if atypical. 7/21
Now I& #39;m going to focus on what I more often see, and what I find to be a more challenging diagnostic entity: DLB.
First described by clinically by Kenji Kosaka, MD (小阪 憲司), a psychiatrist in Japan. 8/21
First described by clinically by Kenji Kosaka, MD (小阪 憲司), a psychiatrist in Japan. 8/21
This is a great article written by Dr. Kosaka that discusses the history of the early clinical science behind DLB. He also described a & #39;cerebral& #39; subtype with no parkinsonism at all (important, we& #39;ll come back to that) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4275567/">https://www.ncbi.nlm.nih.gov/pmc/artic... 9/21
It& #39;s a tough diagnosis: 78% dx with something else first, 24% with a psychiatric diagnosis, and up to 18 months and 3 doctors to arrive at the correct diagnosis.
https://pubmed.ncbi.nlm.nih.gov/20434939/
10/21">https://pubmed.ncbi.nlm.nih.gov/20434939/...
https://pubmed.ncbi.nlm.nih.gov/20434939/
10/21">https://pubmed.ncbi.nlm.nih.gov/20434939/...
Why is it so difficult? I think the answer is that it& #39;s a really heterogeneous disease, with diverse symptoms, and easy to misapply the dx criteria.
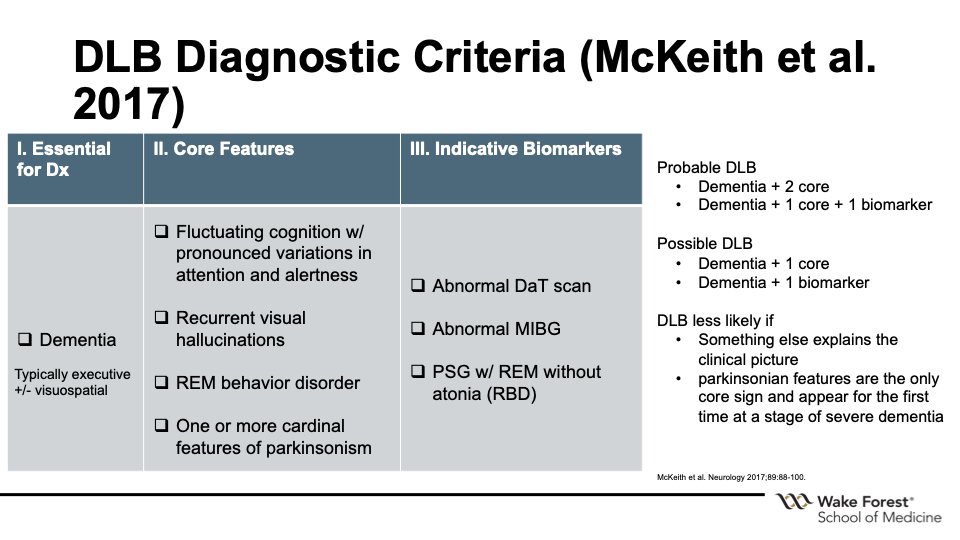
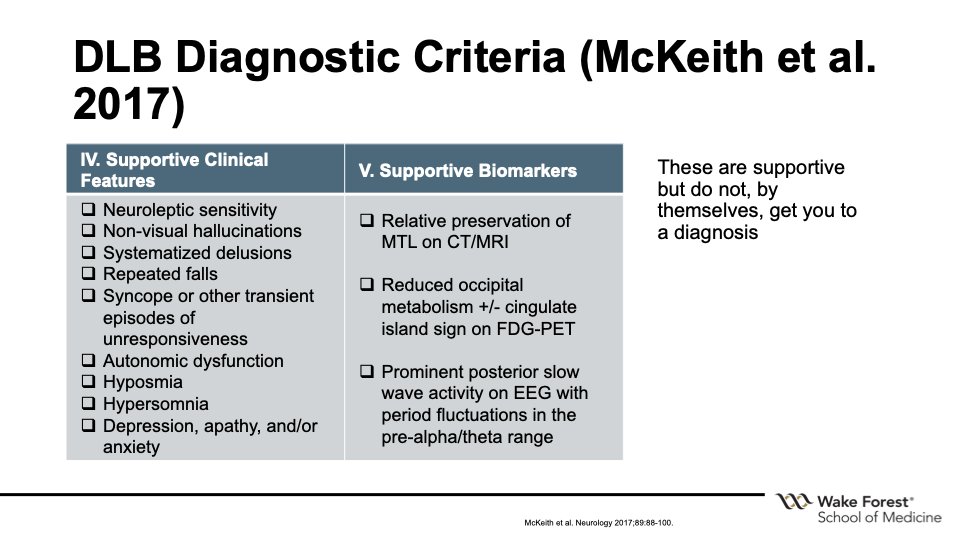
The latest diagnostic criteria were from McKeith et al. (2017) https://pubmed.ncbi.nlm.nih.gov/28592453/ .">https://pubmed.ncbi.nlm.nih.gov/28592453/... 11/21
The latest diagnostic criteria were from McKeith et al. (2017) https://pubmed.ncbi.nlm.nih.gov/28592453/ .">https://pubmed.ncbi.nlm.nih.gov/28592453/... 11/21
Of the 4 core criteria, no single one HAS to be present, but 2 (or 1 + biomarker) need be for probable. I see a lot of referrals where "well it looks like LBD but no parkinsonism" and that& #39;s because there does not have to be!
Let& #39;s take a closer look at the core sx...12/21
Let& #39;s take a closer look at the core sx...12/21
FLUCTUATIONS
In attention and arousal, phenomenologically ~ delirium.
"But everyone fluctuates!" Not like this. Great article describes qualitative differences, fluctuations can be profound in DLB
https://jnnp.bmj.com/content/75/3/382.info">https://jnnp.bmj.com/content/7... 13/21
In attention and arousal, phenomenologically ~ delirium.
"But everyone fluctuates!" Not like this. Great article describes qualitative differences, fluctuations can be profound in DLB
https://jnnp.bmj.com/content/75/3/382.info">https://jnnp.bmj.com/content/7... 13/21
VISUAL HALLUCINATIONS
Can be simple (shadows, peripheral) but usually well-formed, complex (children, animals). Other modalities supportive but not diagnostic. Can have auditory component.
Illusions (mispercep. of a stimulus common, thinking a towel is a snake, etc). 14/21
Can be simple (shadows, peripheral) but usually well-formed, complex (children, animals). Other modalities supportive but not diagnostic. Can have auditory component.
Illusions (mispercep. of a stimulus common, thinking a towel is a snake, etc). 14/21
REM BEHAVIOR DISORDER
Not specific to DLB; can be seen any in alpha-synucleinopathy, which includes DLB.
PTSD also associated with RBD, and SSRIs can unmask (but might still be a risk). 15/21
Not specific to DLB; can be seen any in alpha-synucleinopathy, which includes DLB.
PTSD also associated with RBD, and SSRIs can unmask (but might still be a risk). 15/21
PARKINSONISM
One or more cardinal signs. Often mild, not usually tremor-predominant. PD requires bradykinesia + one other sign, DLB often falls short of this! 16/21
One or more cardinal signs. Often mild, not usually tremor-predominant. PD requires bradykinesia + one other sign, DLB often falls short of this! 16/21
Biomarkers
DAT scan most common one in practice, MIBG cardiac scintigraphy and PSG-confirmed RBD also count.
Abnormal DAT scan points towards a pre-synaptic cause of parkinsonism. It& #39;s specific in this context, not sensitive enough to rule out. 17/21
DAT scan most common one in practice, MIBG cardiac scintigraphy and PSG-confirmed RBD also count.
Abnormal DAT scan points towards a pre-synaptic cause of parkinsonism. It& #39;s specific in this context, not sensitive enough to rule out. 17/21
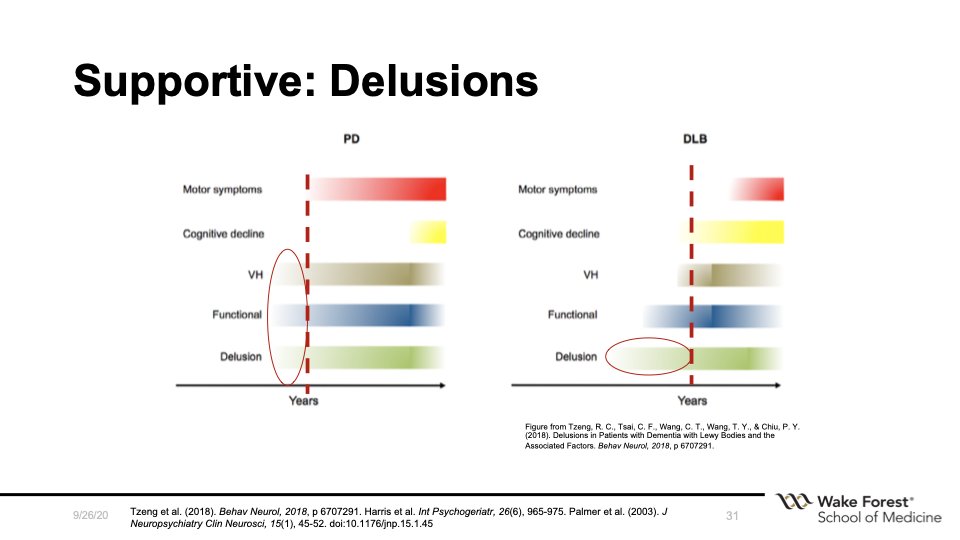
Supportive features and biomarkers. Delusions, neuropsychiatric sx of depression, apathy, anxiety are common. 18/21
These neuropsychiatric symptoms can occur *before* movement or cognitive sx. Be incredibly wary of diagnoses like "new onset delusional disorder" in older adults with no history. 19/21
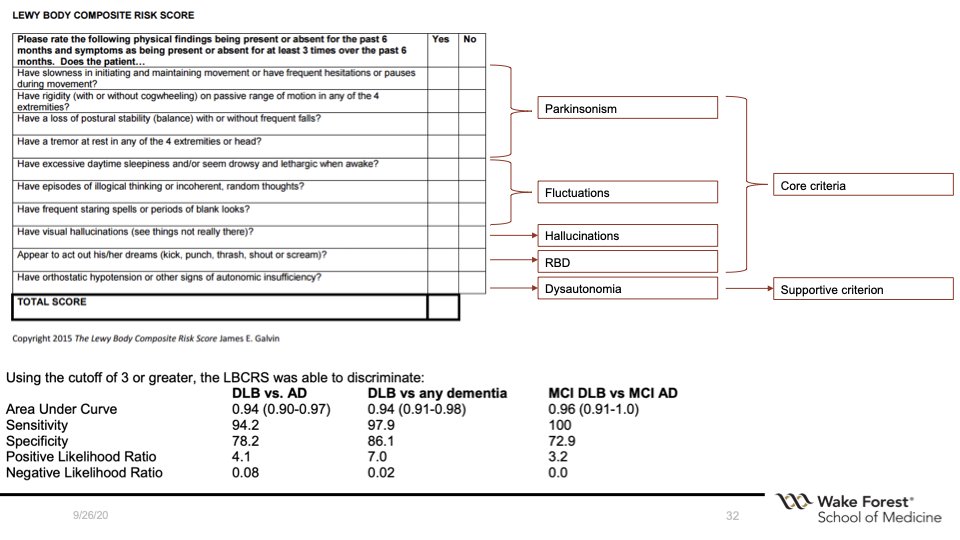
Okay, so, the diagnostic criteria can be complex. How can we simply it for folks who don& #39;t see this frequently?
Jim Galvin& #39;s Lewy Body Composite Risk Score to the rescue! It& #39;s an excellent tool to help with diagnosis. http://med.fau.edu/research/Lewy%20Body%20Composite%20Risk%20Score%20Form%20and%20Instructions.pdf">https://med.fau.edu/research/... 20/21
Jim Galvin& #39;s Lewy Body Composite Risk Score to the rescue! It& #39;s an excellent tool to help with diagnosis. http://med.fau.edu/research/Lewy%20Body%20Composite%20Risk%20Score%20Form%20and%20Instructions.pdf">https://med.fau.edu/research/... 20/21
That& #39;s it. Trying to be semi-brief and keep it as simple as possible since purpose is #meded.
I also want to highlight work from @John_PaulTaylor and colleagues. Invaluable assessment and management toolkits. https://research.ncl.ac.uk/diamondlewy/ ">https://research.ncl.ac.uk/diamondle... check them out and use them! 21/21
I also want to highlight work from @John_PaulTaylor and colleagues. Invaluable assessment and management toolkits. https://research.ncl.ac.uk/diamondlewy/ ">https://research.ncl.ac.uk/diamondle... check them out and use them! 21/21
And if I forgot something, let me know! Tried to tag relevant people and reference work either on slide or linked. Let me know if I missed someone who should be noted. This is a synthesis of the great work of others, so want to give credit where it& #39;s due.
Forgot to talk about what the cog testing should look like! Absolutely agree here. Early attention/ executive deficits +/- visual deficits. Noise pareidolia task (part of LBD module in NACC) can be helpful. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0154713">https://journals.plos.org/plosone/a... https://twitter.com/geropsychlife/status/1309966454800908296">https://twitter.com/geropsych...

 Read on Twitter
Read on Twitter