I was reading through
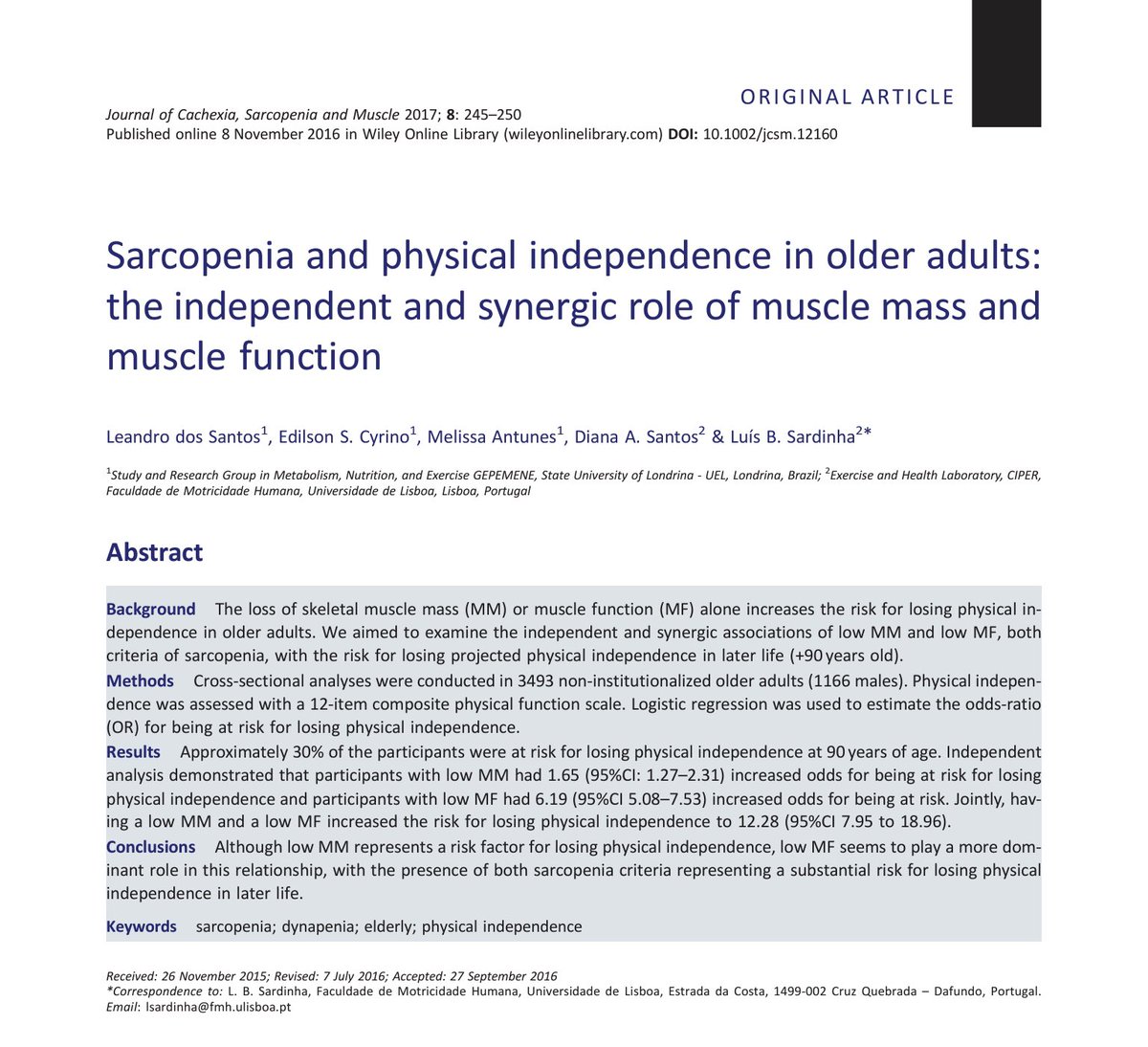
“Sarcopenia prevalence and associations with mortality and hospitalisation by various sarcopenia definitions in 85–89 year old community-dwelling men: a report from the ULSAM study”
because it’s good Friday evening fun.
I saw this figure https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">
“Sarcopenia prevalence and associations with mortality and hospitalisation by various sarcopenia definitions in 85–89 year old community-dwelling men: a report from the ULSAM study”
because it’s good Friday evening fun.
I saw this figure
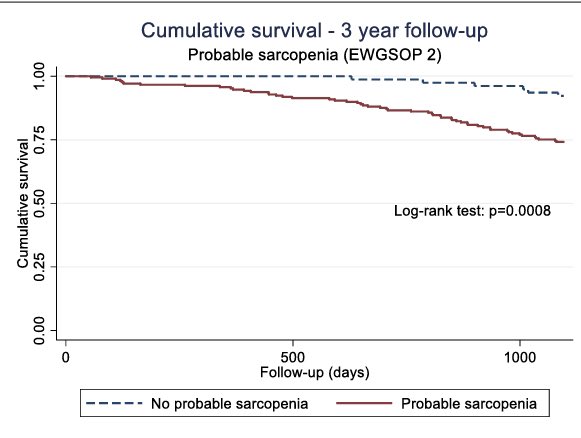
Average age was 86 and there was little mortality difference over the 1000 day follow-up.
Recall, the EWGSOP 2 diagnosis of sarcopenia includes:
-reduced handgrip strength <27kg and/or 5-times chair stand test > 15s
-SMI < 7kg/m^2
(Values above for males bc that was cohort)
Recall, the EWGSOP 2 diagnosis of sarcopenia includes:
-reduced handgrip strength <27kg and/or 5-times chair stand test > 15s
-SMI < 7kg/m^2
(Values above for males bc that was cohort)
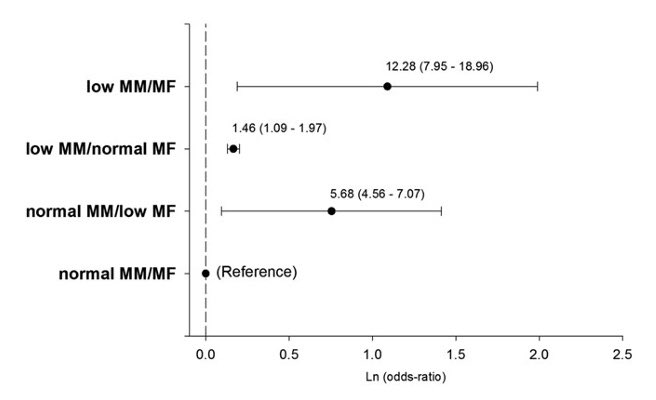
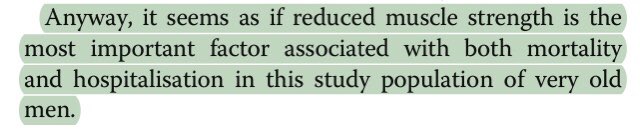
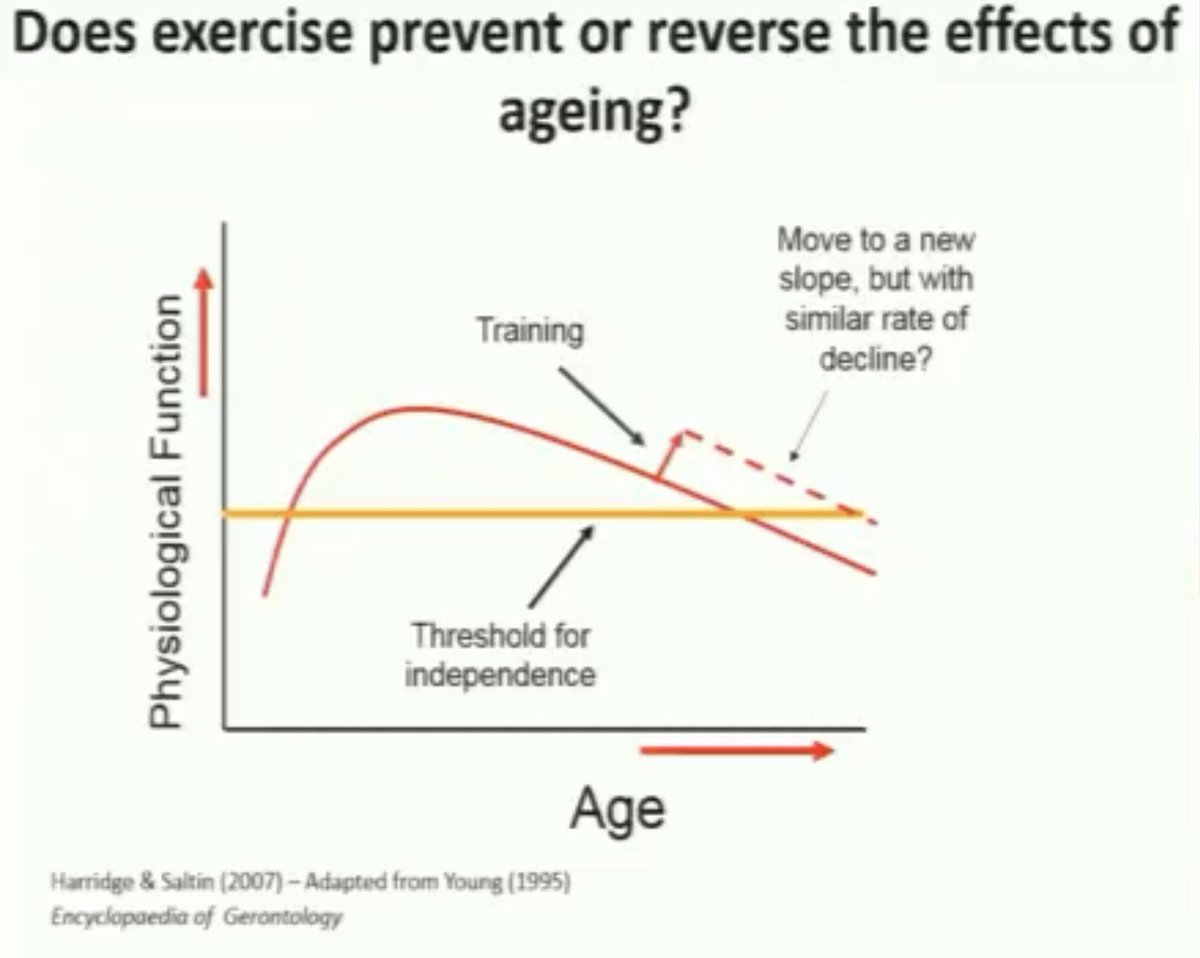
Initially, sarcopenia was based on muscle mass but over time, muscle function has emerged as perhaps the more important determinant of long-term outcomes.
So, when “probable sarcopenia” (strength only) was used, there is a difference in survival.
26% of those with probable sarcopenia died during the follow-up period vs 8% of those without.
26% of those with probable sarcopenia died during the follow-up period vs 8% of those without.
There was also a strong association between probable sarcopenia and hospitalization with no such relationship in those with sarcopenia.
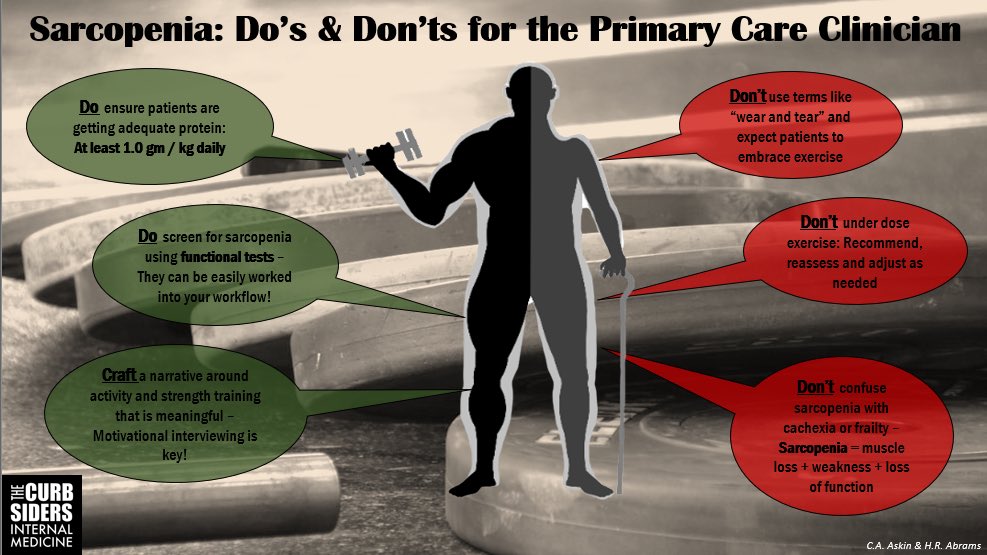
So, we know prevention of sarcopenia is key followed by identifying those with it and then implementing proper treatment.
In primary care, adding one more thing to accomplish during the visit is not going to be easy.
I think that a formal sarcopenia diagnosis is impractical and will be difficult until all scans (DEXA, CT, etc) that have some measure of muscle automatically report findings.
I think that a formal sarcopenia diagnosis is impractical and will be difficult until all scans (DEXA, CT, etc) that have some measure of muscle automatically report findings.
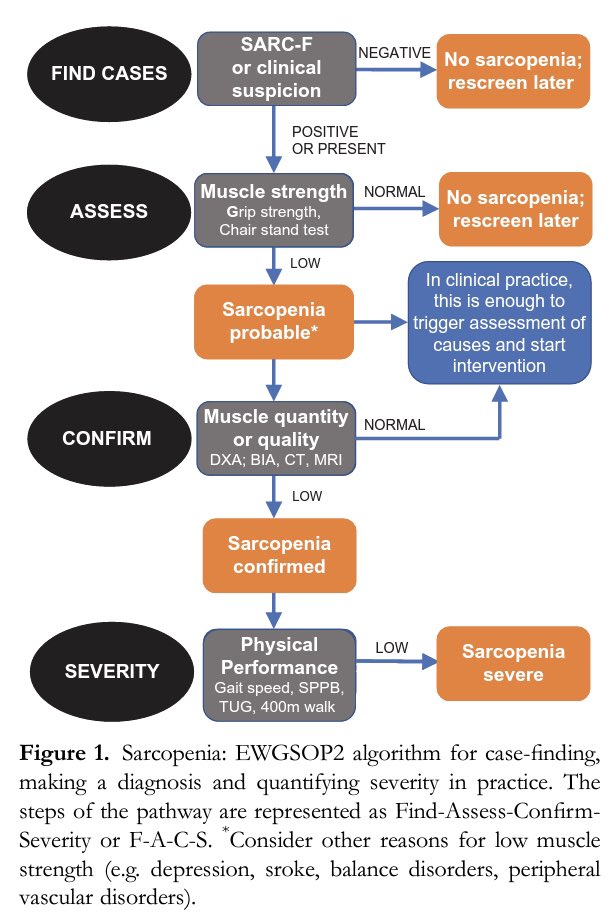
Thankfully the EWGSOP2 has made this easier for me.
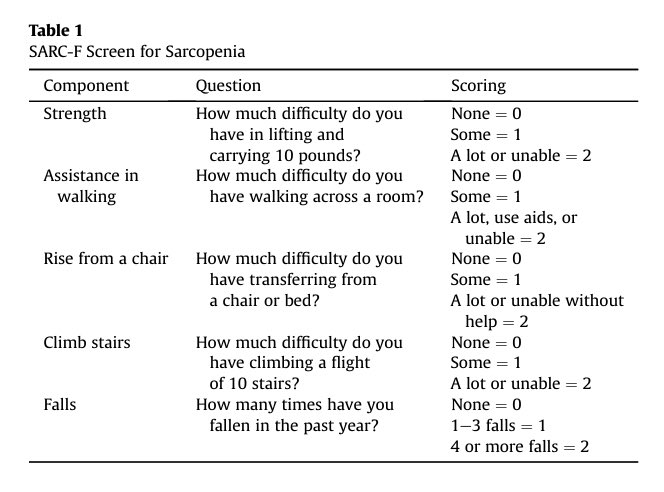
1. Use the SARC-F or clinical suspicion.
2. If pos, test muscle strength (I’ll come back to this).
3. If sarcopenia possible, investigate causes and begin intervention.
1. Use the SARC-F or clinical suspicion.
2. If pos, test muscle strength (I’ll come back to this).
3. If sarcopenia possible, investigate causes and begin intervention.
Muscle testing still takes time. Grip strength requires equipment, adjustments, teaching the patient, testing, etc.
I was happy to hear @AustinBaraki @Jordan_theCoach on @thecurbsiders discussing this. If I’m not mistaken, they felt a chair stand test was sufficient.
I was happy to hear @AustinBaraki @Jordan_theCoach on @thecurbsiders discussing this. If I’m not mistaken, they felt a chair stand test was sufficient.
A patient can either stand without assistance or they can’t. They can either do 5 in <15 seconds or they can’t. This can lead to a quick discussion and exercise recommendations.
Btw, great podcast notes by @thecurbsiders
Btw, great podcast notes by @thecurbsiders
So, how can I implement sarcopenia screening in a busy primary care practice?
1. Identify possible sarcopenia by suspicion or a score of 4 or greater on the SARC-F
2. Do a chair stand test.
Then, I can discuss what this means and exercise or refer.
1. Identify possible sarcopenia by suspicion or a score of 4 or greater on the SARC-F
2. Do a chair stand test.
Then, I can discuss what this means and exercise or refer.
Thankfully, we have an ACSM certified exercise physiologist on staff and great physio referrals in our area.
Our EP has the extended time to work with our patients who need more than simple instructions.
Our EP has the extended time to work with our patients who need more than simple instructions.
References: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6864927/">https://www.ncbi.nlm.nih.gov/pmc/artic...
https://pubmed.ncbi.nlm.nih.gov/27897417/ ">https://pubmed.ncbi.nlm.nih.gov/27897417/...
https://pubmed.ncbi.nlm.nih.gov/30312372/ ">https://pubmed.ncbi.nlm.nih.gov/30312372/...
https://thecurbsiders.com/podcast/186-sarcopenia">https://thecurbsiders.com/podcast/1...
https://youtu.be/q1FlDIErlmA ">https://youtu.be/q1FlDIErl...

 Read on Twitter
Read on Twitter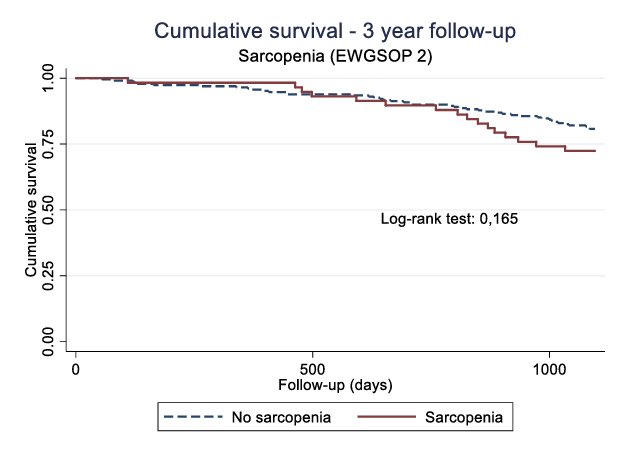 " title="I was reading through “Sarcopenia prevalence and associations with mortality and hospitalisation by various sarcopenia definitions in 85–89 year old community-dwelling men: a report from the ULSAM study”because it’s good Friday evening fun.I saw this figure https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">" class="img-responsive" style="max-width:100%;"/>
" title="I was reading through “Sarcopenia prevalence and associations with mortality and hospitalisation by various sarcopenia definitions in 85–89 year old community-dwelling men: a report from the ULSAM study”because it’s good Friday evening fun.I saw this figure https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">" class="img-responsive" style="max-width:100%;"/>