Yesterday @EricMeyerowitz and I presented insights from new COVID19 papers published over the last month at the HOPE conference. Posting slides and video if interested
Video: http://www.hopeconference.net/conferences/files/2020-09-22/2020-09-22.mp4
Slide">https://www.hopeconference.net/conferenc... deck at end of thread
https://twitter.com/HarvardCFAR/status/1306958585075826688?s=20
https://twitter.com/HarvardCF... href="https://twitter.com/HarvardCFAR">@HarvardCFAR @RMKGandhi
Video: http://www.hopeconference.net/conferences/files/2020-09-22/2020-09-22.mp4
Slide">https://www.hopeconference.net/conferenc... deck at end of thread
https://twitter.com/HarvardCFAR/status/1306958585075826688?s=20
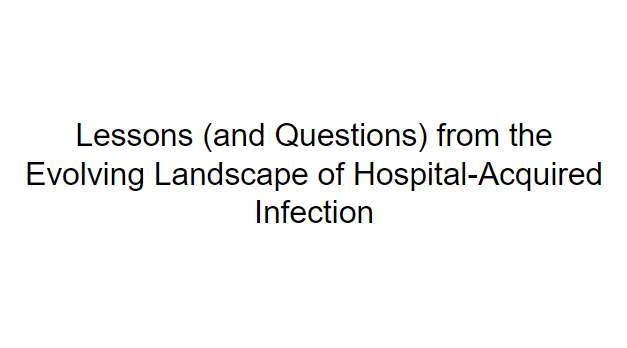
It became apparent during early Chinese epidemic that hospitals were important sites of transmission, >40% infections hospital acquired in Chinese case series
Illustrative example of major outbreak in S Africa stemming from single introduction:
https://www.krisp.org.za/manuscripts/StAugustinesHospitalOutbreakInvestigation_FinalReport_15may2020_comp.pdf">https://www.krisp.org.za/manuscrip...
Illustrative example of major outbreak in S Africa stemming from single introduction:
https://www.krisp.org.za/manuscripts/StAugustinesHospitalOutbreakInvestigation_FinalReport_15may2020_comp.pdf">https://www.krisp.org.za/manuscrip...
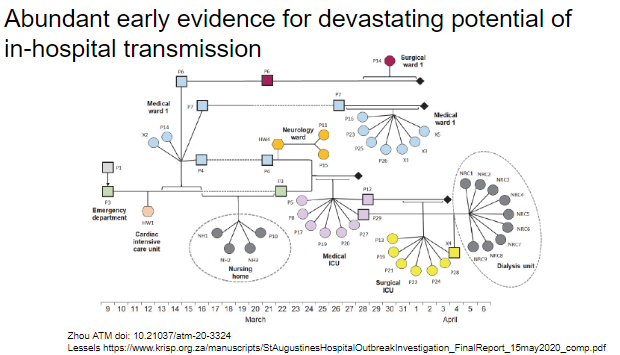
Patients/HCW rightly became scared, and we saw major and concerning decreases in healthcare utilization for urgent/emergent medical issues. E.g. new report showing marked decrease in patients with TB ( #1 infectious killer worldwide) presenting for care
https://doi.org/10.3201/eid2611.203163">https://doi.org/10.3201/e...
https://doi.org/10.3201/eid2611.203163">https://doi.org/10.3201/e...
However, at the same time, we began to see indirect evidence for high efficacy of relatively simple intervention => universal masking. Population-level study from Duke:
https://www.cambridge.org/core/journals/infection-control-and-hospital-epidemiology/article/universal-masking-is-an-effective-strategy-to-flatten-the-sarscov2-healthcare-worker-epidemiologic-curve/9301E77612122039190A29CB7223F9C4">https://www.cambridge.org/core/jour...
https://www.cambridge.org/core/journals/infection-control-and-hospital-epidemiology/article/universal-masking-is-an-effective-strategy-to-flatten-the-sarscov2-healthcare-worker-epidemiologic-curve/9301E77612122039190A29CB7223F9C4">https://www.cambridge.org/core/jour...
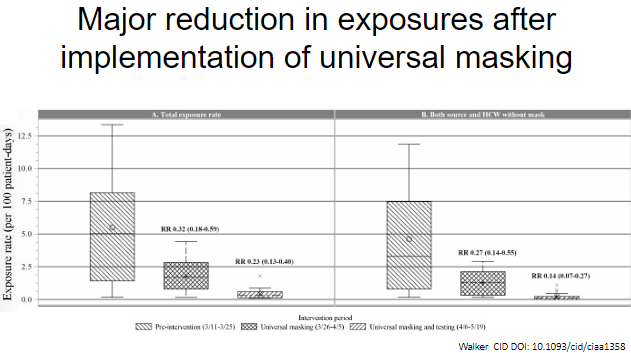
This nice new study from UAB illustrates the massive reduction in exposures with implementation of universal masking
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa1358/5903054">https://academic.oup.com/cid/advan...
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa1358/5903054">https://academic.oup.com/cid/advan...
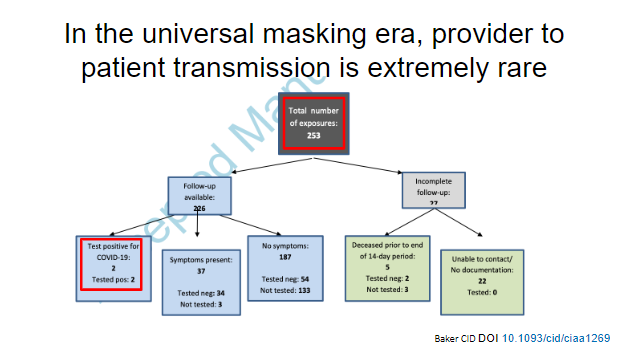
Contact tracing study of patients exposed to HCW with infection show very low rates of infection in universal masking. Only 1 definitive infection out of 253 exposures during a 30 minute unmasked outpatient appointment.
https://pubmed.ncbi.nlm.nih.gov/32856692/ ">https://pubmed.ncbi.nlm.nih.gov/32856692/...
https://pubmed.ncbi.nlm.nih.gov/32856692/ ">https://pubmed.ncbi.nlm.nih.gov/32856692/...
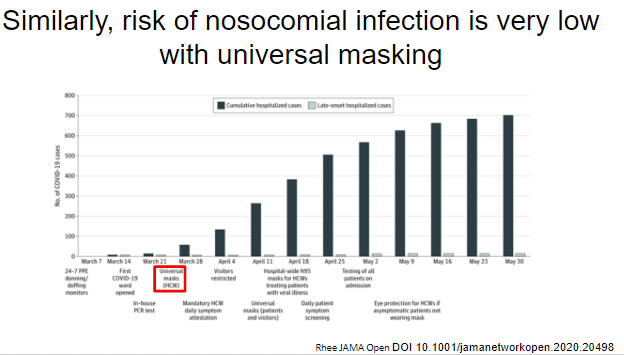
Complementary study showing nosocomial infection was extremely rare during the surge in Boston in universal masking era
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2770287">https://jamanetwork.com/journals/...
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2770287">https://jamanetwork.com/journals/...
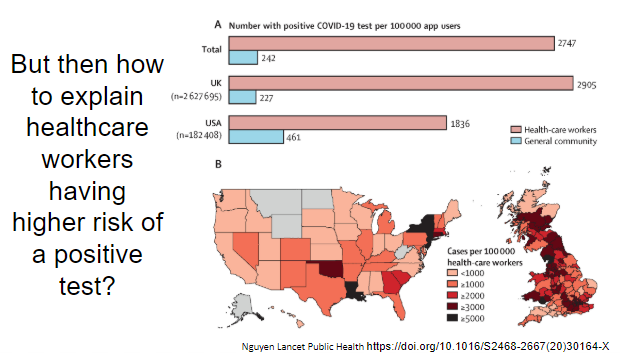
But how do we square these findings with ongoing reports of HCW making up large numbers of cases worldwide? https://www.washingtonpost.com/world/2020/09/17/health-care-workers-make-up-one-seven-covid-19-cases-recorded-globally-who-says/">https://www.washingtonpost.com/world/202...
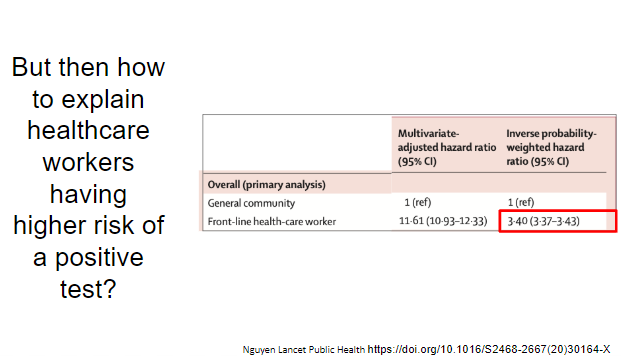
To explore this, we will go through this very interesting paper published in Lancet Public health, study of voluntary mobile app use including 2 million community members and 100k front-line hcw
https://doi.org/10.1016/S2468-2667(20)30164-X">https://doi.org/10.1016/S...
https://doi.org/10.1016/S2468-2667(20)30164-X">https://doi.org/10.1016/S...
They used multivariable models to find positive test highly associated with being a HCW, even after attempting to adjust for the much greater likelihood of having a test as a HCW (although much attenuated)
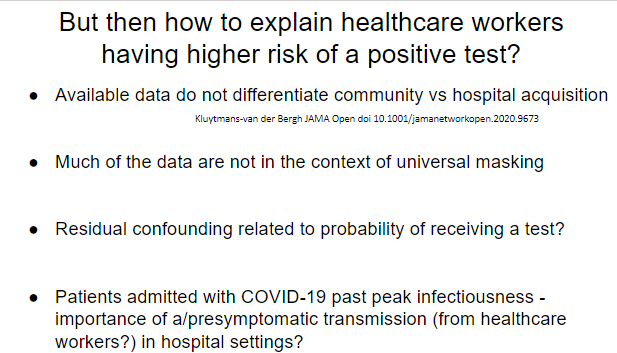
So, how do we explain all of these findings? The short answer is I don’t think we exactly know yet, but here are some proposed considerations.
What we really need is a detailed contact tracing study of healthcare worker infections in the universal masking era.
What we really need is a detailed contact tracing study of healthcare worker infections in the universal masking era.
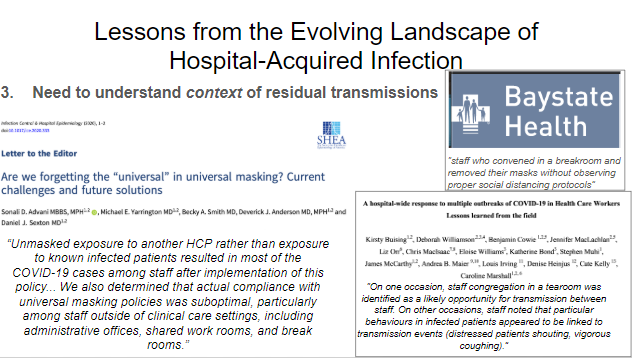
Lesson 3 - MOST critical point IMO. We need to understand residual outbreaks in the universal masking setting. Unmasked in work rooms or cafeterias = major culprit so far, we MUST support HCW to be able to work safely rather than pointing fingers (people gotta eat!!)
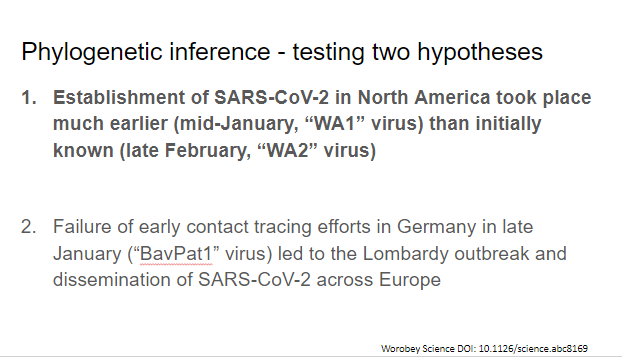
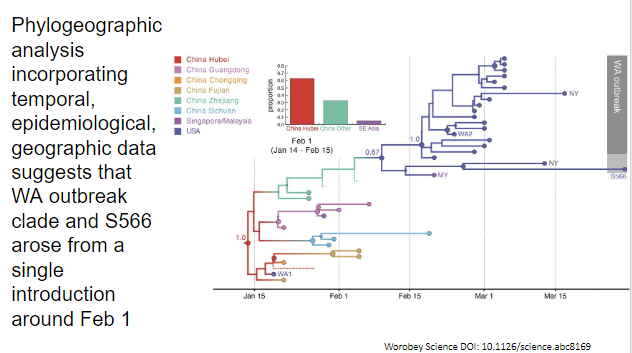
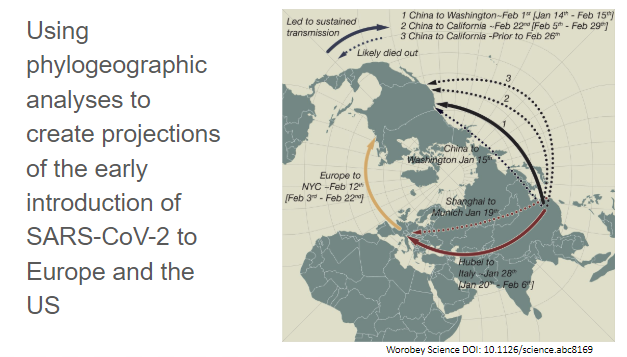
For this we will be going through a few pieces of this fascinating paper, an almost forensic phylogenetic analysis providing lessons from the early global spread of CoV-2
https://science.sciencemag.org/content/early/2020/09/11/science.abc8169">https://science.sciencemag.org/content/e...
https://science.sciencemag.org/content/early/2020/09/11/science.abc8169">https://science.sciencemag.org/content/e...
They address two hypotheses in this paper, we’ll focus on the first one, the introduction of CoV-2 into North America
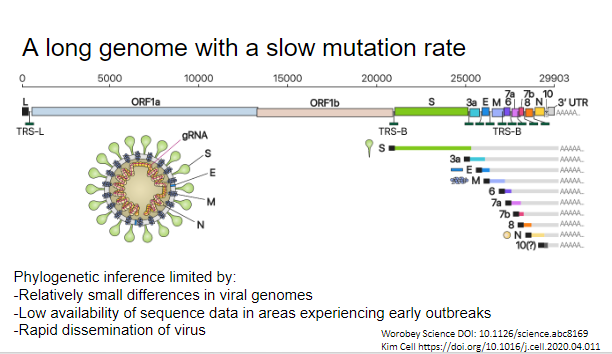
Before we get there, important points abt cov-2 genome:
1. As a cov, large relative to RNA viruses (~30k bp)
2. #1 possible because of a high fidelity proofreading exoribonuclease
3. Because of #2, v slow rate of evolution (evolutionary rate much slower than transmission rate)
1. As a cov, large relative to RNA viruses (~30k bp)
2. #1 possible because of a high fidelity proofreading exoribonuclease
3. Because of #2, v slow rate of evolution (evolutionary rate much slower than transmission rate)
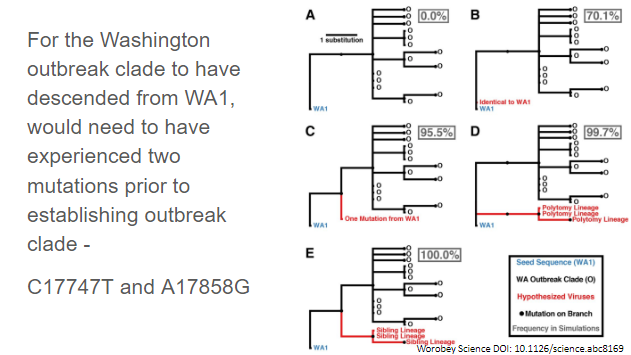
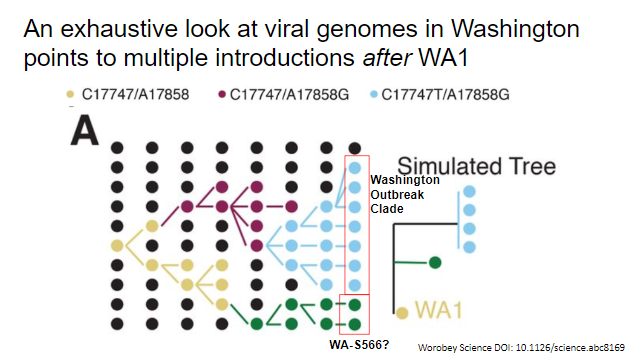
Back to the paper. They used sampling from simulations to show that observed pattern of observed viruses through March 15 would be extremely unlikely if descended from WA1
They further bolstered this claim by looking at more exhaustive collection of genomes in Washington area, finding a later virus that lacked two washington outbreak clade-defining mutations and showing that again unlikely to descend from WA1
They then proceed to a bayesian phylogeographic analysis suggestion this phylogeny accounting for gaps in the data, placing the initial introduction from which the washington outbreak clade descended around Feb 1.
They do a number of other analyses to generate this projection of early introductions into Europe and the US. Key pt: multiple “dead end” intros prior to establishment, highlighting narrow opportunity for contact tracing / case finding to prevent this
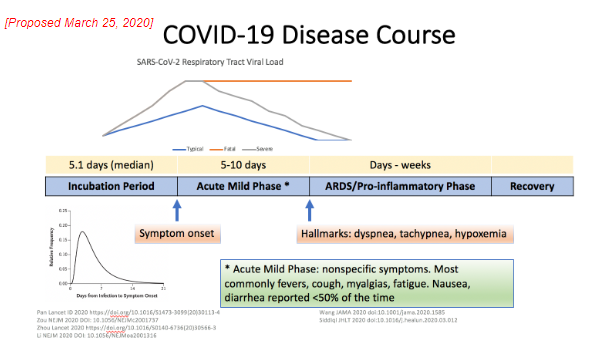
We presented this model on 3/25 based on what was known at that time. Even at that time a lot was known about the illness course. In general, it involves a complex interplay between the virus and the immune system
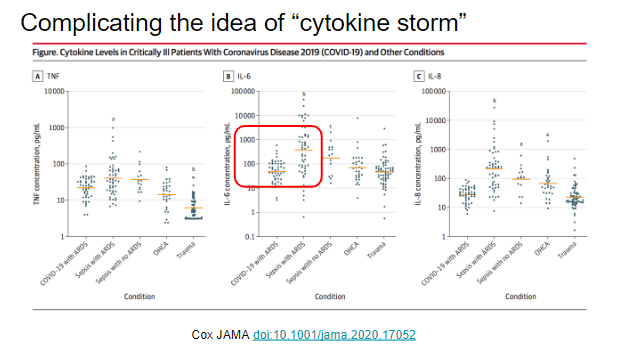
This small study compared 3 cytokines from patients with critical COVID to other patients needing ICU level with non-cytokine storm states and found cytokine levels were lower among the patients with COVID.
-->Critical COVID may not be a cytokine storm
https://jamanetwork.com/journals/jama/fullarticle/2770484">https://jamanetwork.com/journals/...
-->Critical COVID may not be a cytokine storm
https://jamanetwork.com/journals/jama/fullarticle/2770484">https://jamanetwork.com/journals/...
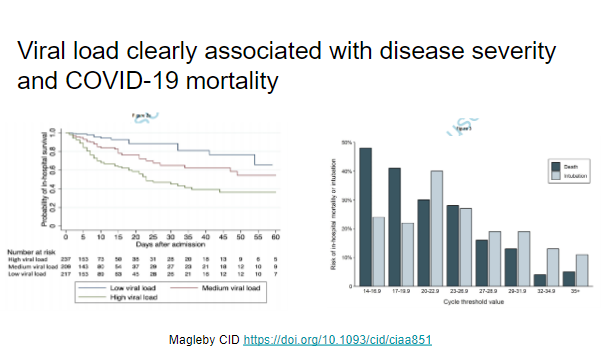
There is now stronger evidence that viral load is associated with mortality and severe COVID-19 outcomes. This is from a NYC cohort with 678 patients
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa851/5865363">https://academic.oup.com/cid/advan...
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa851/5865363">https://academic.oup.com/cid/advan...
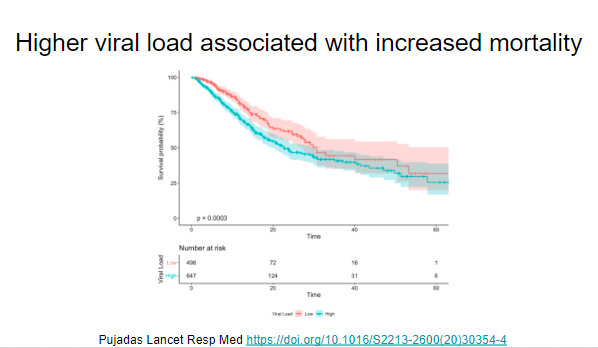
Another NYC cohort of nearly 1200 patients with similar findings https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(20)30354-4/fulltext">https://www.thelancet.com/journals/...
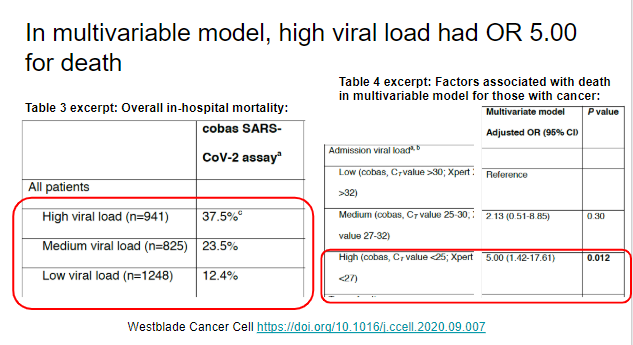
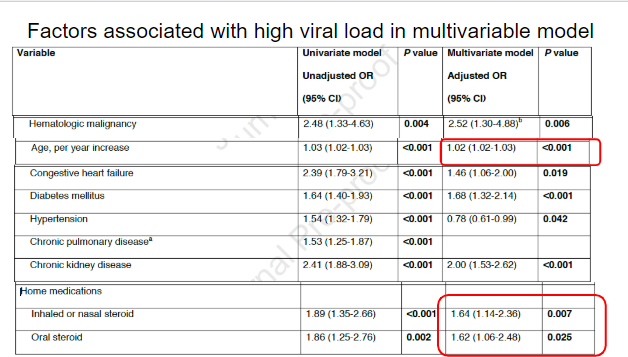
Recent paper from Cancer Cell looking at more than 3000 patients with COVID-19 also from NYC and similarly found a strong association between high viral load and severe outcomes
https://www.sciencedirect.com/science/article/pii/S1535610820304815?via%3Dihub">https://www.sciencedirect.com/science/a...
https://www.sciencedirect.com/science/article/pii/S1535610820304815?via%3Dihub">https://www.sciencedirect.com/science/a...
In a multivariable model they found some factors associated with higher viral loads, including age and baseline inhaled, nasal, or oral corticosteroids.
Moving on to an important update in the adaptive immune response to COVID-19. The group presenting this next paper has already done important COVID-19 work. Here Dr. Fauci holding an earlier paper we have discussed
https://www.cell.com/cell/pdf/S0092-8674(20)30610-3.pdf">https://www.cell.com/cell/pdf/...
https://www.cell.com/cell/pdf/S0092-8674(20)30610-3.pdf">https://www.cell.com/cell/pdf/...
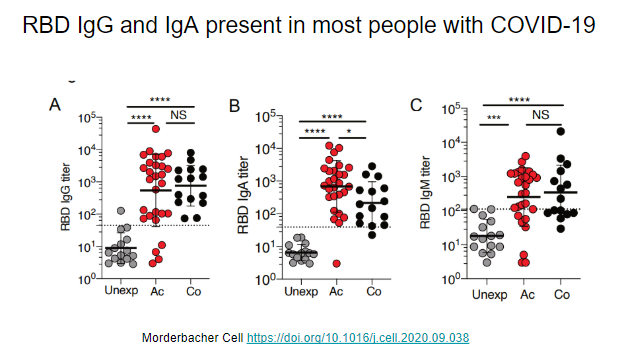
In their new paper, this research team classifies broad adaptive immune responses to COVID-19. First, they look at RBD antibodies and find IgG and IgA are frequently present, but IgM less so
https://www.cell.com/cell/pdf/S0092-8674(20)31235-6.pdf?_returnURL=https%3A%2F%2Flinkinghub.elsevier.com%2Fretrieve%2Fpii%2FS0092867420312356%3Fshowall%3Dtrue">https://www.cell.com/cell/pdf/...
https://www.cell.com/cell/pdf/S0092-8674(20)31235-6.pdf?_returnURL=https%3A%2F%2Flinkinghub.elsevier.com%2Fretrieve%2Fpii%2FS0092867420312356%3Fshowall%3Dtrue">https://www.cell.com/cell/pdf/...
They find receptor binding domain (RBD) IgG titers correlate with Spike IgG and neutralizing antibody titers
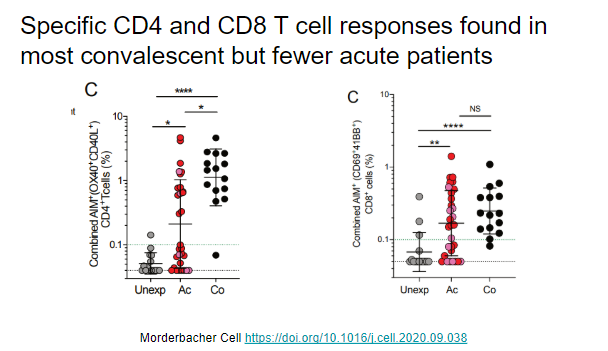
They look at specific CD4 and CD8 cell responses to SARS-CoV-2 and fine these are common in convalescent patients but less common in acute patients
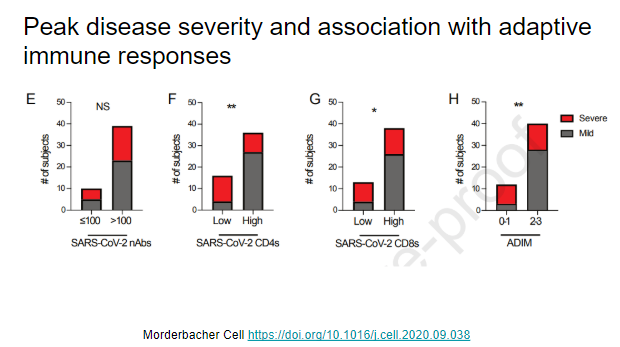
They then look at adaptive immune responses and disease severity and find: no association for neutralizing Abs. Stronger specific CD4, CD8 and composite adaptive immune responses are associated with more mild outcomes
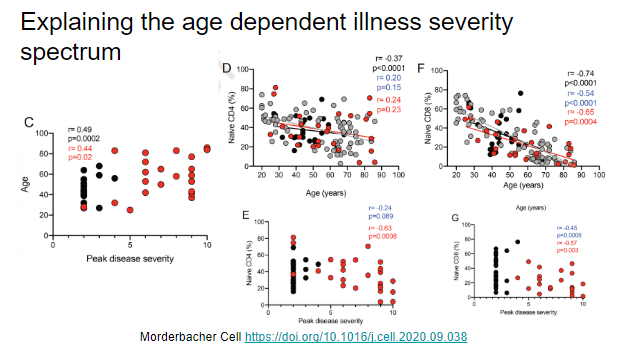
That age is associated with severe outcomes has been found around the globe. They report this in their cohort. They find that naive CD4 and CD8 cell percentage declines with age and that naive CD8 cell percentage is associated with severe disease for acute and convalescent cases
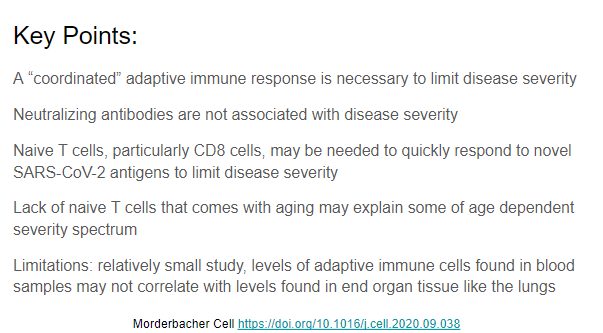
They conclude that a coordinated adaptive immune response and not just an antibody response seem to be needed to limit disease severity. Immunologic changes with age may at least partially explain severity spectrum
We propose updating the model for pathogenesis as in this slide. In mild cases a modest viral load is associated with robust coordinated adaptive immune response. Severe cases are marked by much higher viral loads with an uncoordinated response
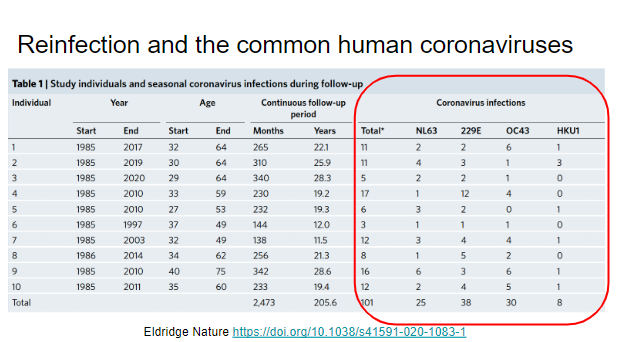
This paper looks at reinfection in other common covs. Researchers use a cohort with years samples and look at reinfections in 10 patients, defining reinfection as increase in antibody titers of the 4 common coronaviruses. They find reinfections are common
https://doi.org/10.1038/s41591-020-1083-1">https://doi.org/10.1038/s...
https://doi.org/10.1038/s41591-020-1083-1">https://doi.org/10.1038/s...
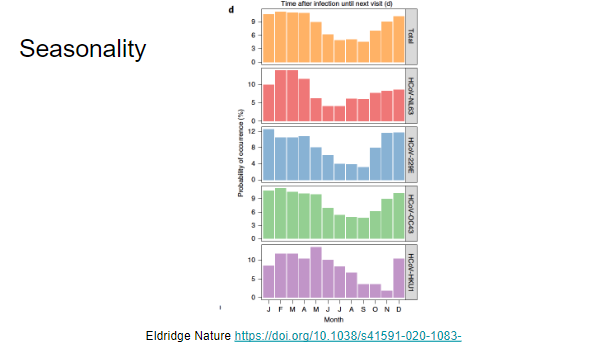
A seasonality in incidence of new coronavirus infections was seen. This is predicted eventually once SARS-CoV-2 has circulated widely enough
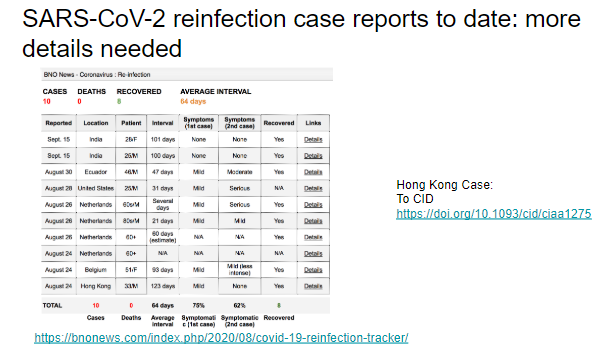
Hong Kong case was first credible cov2 reinfection case
Many other cases need more details. Perplexing that some are reporting possible worse symptoms at reinfection (immune protection from prior episode might be expected)
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa1275/5897019">https://academic.oup.com/cid/advan...
Many other cases need more details. Perplexing that some are reporting possible worse symptoms at reinfection (immune protection from prior episode might be expected)
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa1275/5897019">https://academic.oup.com/cid/advan...
A summary slide of the papers we covered here
Slide deck here: https://docs.google.com/presentation/d/17m2NB4ZMErfDkH-J6G0T0435S7LWKw0wjt1vcjGpFVE/edit?usp=sharing
Again,">https://docs.google.com/presentat... video here:
http://www.hopeconference.net/conferences/files/2020-09-22/2020-09-22.mp4">https://www.hopeconference.net/conferenc...
Slide deck here: https://docs.google.com/presentation/d/17m2NB4ZMErfDkH-J6G0T0435S7LWKw0wjt1vcjGpFVE/edit?usp=sharing
Again,">https://docs.google.com/presentat... video here:
http://www.hopeconference.net/conferences/files/2020-09-22/2020-09-22.mp4">https://www.hopeconference.net/conferenc...

 Read on Twitter
Read on Twitter @HarvardCFAR @RMKGandhi" title="Yesterday @EricMeyerowitz and I presented insights from new COVID19 papers published over the last month at the HOPE conference. Posting slides and video if interestedVideo: https://www.hopeconference.net/conferenc... deck at end of thread https://twitter.com/HarvardCF... href="https://twitter.com/HarvardCFAR">@HarvardCFAR @RMKGandhi" class="img-responsive" style="max-width:100%;"/>
@HarvardCFAR @RMKGandhi" title="Yesterday @EricMeyerowitz and I presented insights from new COVID19 papers published over the last month at the HOPE conference. Posting slides and video if interestedVideo: https://www.hopeconference.net/conferenc... deck at end of thread https://twitter.com/HarvardCF... href="https://twitter.com/HarvardCFAR">@HarvardCFAR @RMKGandhi" class="img-responsive" style="max-width:100%;"/>