Two questions on this biopsy:
1. Would your interpretation differ based on the anatomical location of the biopsy? (i.e. would you call it the same irrespective from where the biopsy was taken?)
2. Would you ask for p16 IHC?
#pathology #IHCpath
1. Would your interpretation differ based on the anatomical location of the biopsy? (i.e. would you call it the same irrespective from where the biopsy was taken?)
2. Would you ask for p16 IHC?
#pathology #IHCpath
1/ Thanks everyone for the input and opinions  https://abs.twimg.com/emoji/v2/... draggable="false" alt="👌" title="Ok hand" aria-label="Emoji: Ok hand">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👌" title="Ok hand" aria-label="Emoji: Ok hand"> https://abs.twimg.com/emoji/v2/... draggable="false" alt="🙏" title="Folded hands" aria-label="Emoji: Folded hands"> great discussions
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🙏" title="Folded hands" aria-label="Emoji: Folded hands"> great discussions  https://abs.twimg.com/emoji/v2/... draggable="false" alt="👏" title="Applaus-Zeichen" aria-label="Emoji: Applaus-Zeichen">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👏" title="Applaus-Zeichen" aria-label="Emoji: Applaus-Zeichen"> https://abs.twimg.com/emoji/v2/... draggable="false" alt="👏" title="Applaus-Zeichen" aria-label="Emoji: Applaus-Zeichen"> I am having difficulties making diagnoses based on single images...this is not how we work and think, so the points on looking at the levels and the whole lesion is well taken
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👏" title="Applaus-Zeichen" aria-label="Emoji: Applaus-Zeichen"> I am having difficulties making diagnoses based on single images...this is not how we work and think, so the points on looking at the levels and the whole lesion is well taken  https://abs.twimg.com/emoji/v2/... draggable="false" alt="👍" title="Thumbs up" aria-label="Emoji: Thumbs up">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👍" title="Thumbs up" aria-label="Emoji: Thumbs up">
2/ A clear cut split is if we look at the head and neck lesions or anogenital lesions... nomenclature, grading, use of p16 IHC might different between these two anatomic sites ...
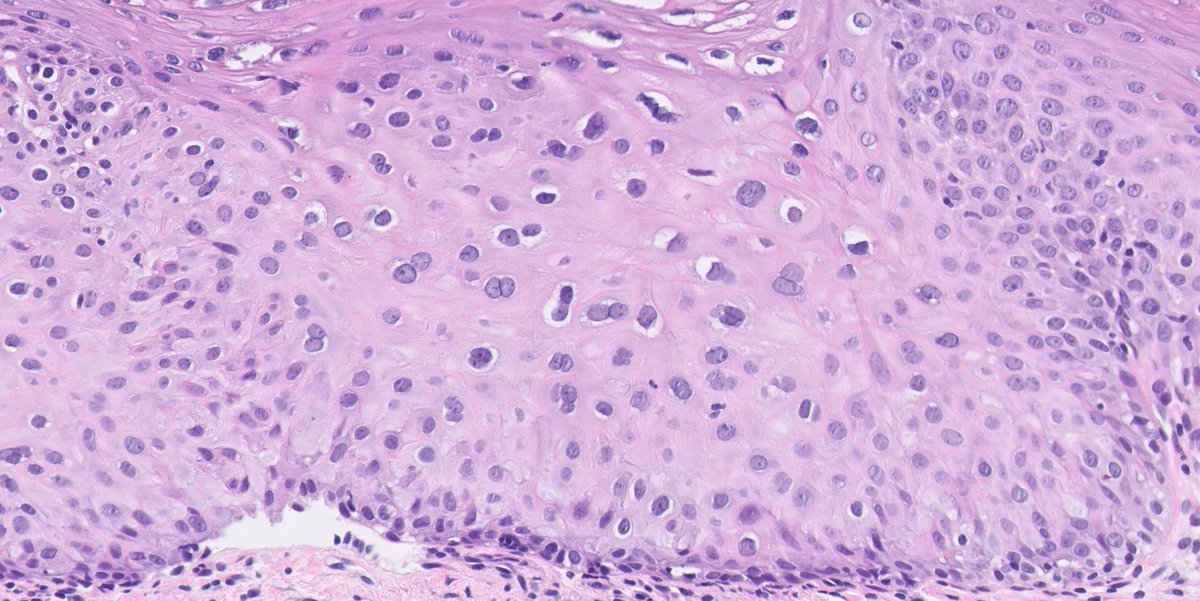
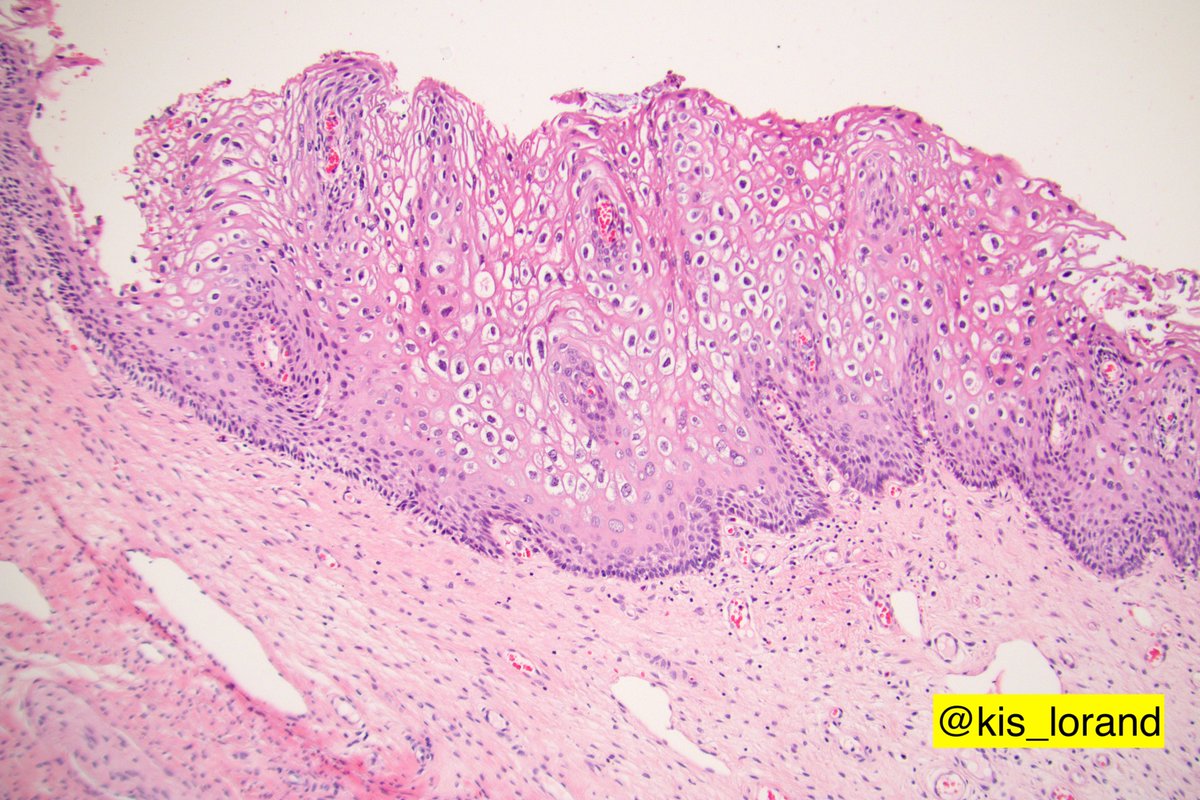
3/ If we restrict our discussion to the anogenital sites (anus, perianal, cervix, vagina, penis, scrotum) then looking at the images that show a disorganized but maturing squamous epithelium (cells have a lot of eosinophilic cytoplasm and they flatten at the top),
4/ but also show multi-/binucleation, nuclear enlargement, and pleomorphism accompanied by perinuclear halos that are diagnostic cytopathic effects of productive (virion-producing) HPV infection...
5/ in the absence of mitoses especially mitoses situated above the lower third of the epithelium or atypical mitoses, in the absence of increased nuclear-to-cytoplasmic ratio of the cells and presence of maturation, the lesion is diagnosed as ...
6/ LSIL- low-grade squamous intraepithelial lesion irrespective of the anogenital region  https://abs.twimg.com/emoji/v2/... draggable="false" alt="👍" title="Thumbs up" aria-label="Emoji: Thumbs up">this is because we learned that what we see in these lesions is the morphological expression of a virus producing viral-epithelial interaction...
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👍" title="Thumbs up" aria-label="Emoji: Thumbs up">this is because we learned that what we see in these lesions is the morphological expression of a virus producing viral-epithelial interaction...
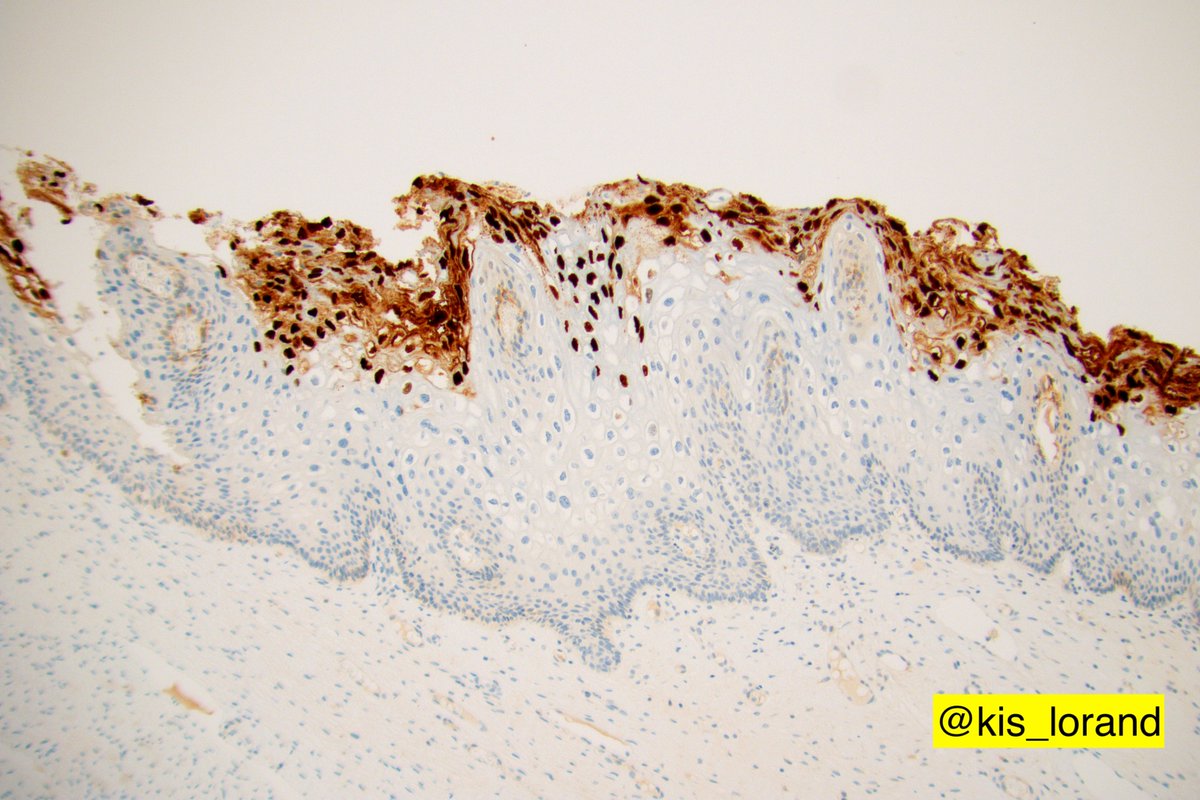
7/ what basically the virus wants it is to push the infected cell in the cell cycle and afterwards differentiate so the virion production can start and the new virus can spread ...this virion production you can easily visualize with IHC if you stain such a lesion for viral
8/ proteins that are expressed and incorporated in the virions, such as the VCA-viral capsid antigen shown on a different case  https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">the staining is limited to the superficial part of the epithelium because at this level is the viral protein expressed ...
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">the staining is limited to the superficial part of the epithelium because at this level is the viral protein expressed ...
9/ if you would do HPV DNA in situ hybridization on the same section you would see that the HPV DNA is present in the whole epithelial thickness but the expression of different viral proteins is linked to the differentiation of the squamous cells,
10/ produced when needed... at the surface...assembled and released so it can spread... enough with the virology  https://abs.twimg.com/emoji/v2/... draggable="false" alt="😄" title="Lächelndes Gesicht mit geöffnetem Mund und lächelnden Augen" aria-label="Emoji: Lächelndes Gesicht mit geöffnetem Mund und lächelnden Augen">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="😄" title="Lächelndes Gesicht mit geöffnetem Mund und lächelnden Augen" aria-label="Emoji: Lächelndes Gesicht mit geöffnetem Mund und lächelnden Augen"> https://abs.twimg.com/emoji/v2/... draggable="false" alt="😁" title="Grinsendes Gesicht mit lächelnden Augen" aria-label="Emoji: Grinsendes Gesicht mit lächelnden Augen"> from diagnostic perspectives...
https://abs.twimg.com/emoji/v2/... draggable="false" alt="😁" title="Grinsendes Gesicht mit lächelnden Augen" aria-label="Emoji: Grinsendes Gesicht mit lächelnden Augen"> from diagnostic perspectives...
11/ if you sign out biopsies from the named anogenital sites then you HAVE TO READ the The Lower Anogenital Squamous Terminology Standardization Project recommendations - freely available from 2012 https://meridian.allenpress.com/aplm/article/136/10/1266/133088/The-Lower-Anogenital-Squamous-Terminology">https://meridian.allenpress.com/aplm/arti...
12/ the LAST recommendations clearly state why we want to split the anogenital HPV-related squamous lesions between LSIL and HSIL (2 categories instead of 3), why we can unify the different anogenital sites, what are the possible biomarkers and when to use them and other issues
13/ do also note that based on literature review and data extractions the LAST project concluded that ONLY p16 had sufficient evidence on which to make recommendations regarding use in lower anogenital squamous lesions.
14/ the short answer to the p16 IHC (as a surrogate marker to the activation of HPV E6/ E7–driven cell proliferation) is that if you committed yourself to the LSIL or HSIL diagnoses based on H&E then you should NOT do the p16 IHC  https://abs.twimg.com/emoji/v2/... draggable="false" alt="👍" title="Thumbs up" aria-label="Emoji: Thumbs up">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👍" title="Thumbs up" aria-label="Emoji: Thumbs up">
15/ When you should order the p16 IHC in such anogenital lesions  https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">I discussed it in a previous thread, please take a look at it if interested https://twitter.com/kis_lorand/status/1065689666219839488">https://twitter.com/kis_loran...
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">I discussed it in a previous thread, please take a look at it if interested https://twitter.com/kis_lorand/status/1065689666219839488">https://twitter.com/kis_loran...
16/ let& #39;s stop here for today  https://abs.twimg.com/emoji/v2/... draggable="false" alt="😄" title="Lächelndes Gesicht mit geöffnetem Mund und lächelnden Augen" aria-label="Emoji: Lächelndes Gesicht mit geöffnetem Mund und lächelnden Augen">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="😄" title="Lächelndes Gesicht mit geöffnetem Mund und lächelnden Augen" aria-label="Emoji: Lächelndes Gesicht mit geöffnetem Mund und lächelnden Augen"> https://abs.twimg.com/emoji/v2/... draggable="false" alt="😂" title="Gesicht mit Freudentränen" aria-label="Emoji: Gesicht mit Freudentränen">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="😂" title="Gesicht mit Freudentränen" aria-label="Emoji: Gesicht mit Freudentränen">

 Read on Twitter
Read on Twitter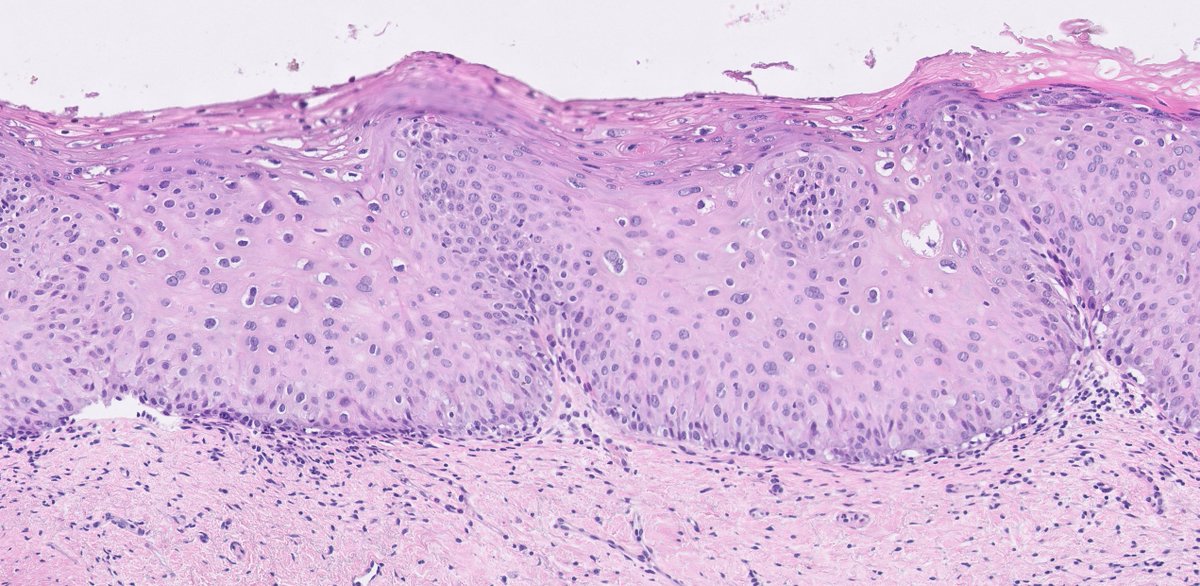
 the staining is limited to the superficial part of the epithelium because at this level is the viral protein expressed ..." title="8/ proteins that are expressed and incorporated in the virions, such as the VCA-viral capsid antigen shown on a different case https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">the staining is limited to the superficial part of the epithelium because at this level is the viral protein expressed ...">
the staining is limited to the superficial part of the epithelium because at this level is the viral protein expressed ..." title="8/ proteins that are expressed and incorporated in the virions, such as the VCA-viral capsid antigen shown on a different case https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">the staining is limited to the superficial part of the epithelium because at this level is the viral protein expressed ...">
 the staining is limited to the superficial part of the epithelium because at this level is the viral protein expressed ..." title="8/ proteins that are expressed and incorporated in the virions, such as the VCA-viral capsid antigen shown on a different case https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">the staining is limited to the superficial part of the epithelium because at this level is the viral protein expressed ...">
the staining is limited to the superficial part of the epithelium because at this level is the viral protein expressed ..." title="8/ proteins that are expressed and incorporated in the virions, such as the VCA-viral capsid antigen shown on a different case https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">the staining is limited to the superficial part of the epithelium because at this level is the viral protein expressed ...">


