Thread/
Do you look after patients with HHS?
UK guidelines use calculated osmolality = 2Na + Glucose + Urea
“What’s the problem?”
Including urea lowers the diagnostic threshold in patients with CKD
- a group at https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">risk of treatment harm
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">risk of treatment harm
But it gets much worse https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">
#medtwitter
Do you look after patients with HHS?
UK guidelines use calculated osmolality = 2Na + Glucose + Urea
“What’s the problem?”
Including urea lowers the diagnostic threshold in patients with CKD
- a group at
But it gets much worse
#medtwitter
2/
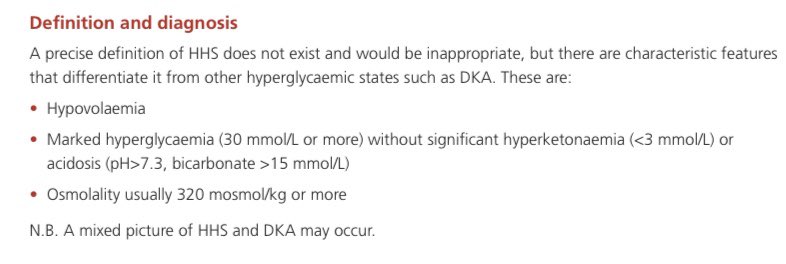
You do the calculation & the recommendation is to use a cut-off of >320 mosmol/kg = hyperosmolar
But what if the patient has advanced CKD and their urea is always 30?
Well, there’s no mention of that in the 20+ page UK guidance....
http://www.diabetologists-abcd.org.uk/JBDS/JBDS_IP_HHS_Adults.pdf">https://www.diabetologists-abcd.org.uk/JBDS/JBDS...
You do the calculation & the recommendation is to use a cut-off of >320 mosmol/kg = hyperosmolar
But what if the patient has advanced CKD and their urea is always 30?
Well, there’s no mention of that in the 20+ page UK guidance....
http://www.diabetologists-abcd.org.uk/JBDS/JBDS_IP_HHS_Adults.pdf">https://www.diabetologists-abcd.org.uk/JBDS/JBDS...
3/
“So what happens?”
When these CKD patients come in with hyperglycaemia it is MUCH easier for them to meet the biochemical criteria for calculated hyperosmolality
= lots of IV fluids (+-insulin) if HHS protocol is started inappropriately
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="❗️" title="Rotes Ausrufezeichen" aria-label="Emoji: Rotes Ausrufezeichen">not a good look in late CKD
https://abs.twimg.com/emoji/v2/... draggable="false" alt="❗️" title="Rotes Ausrufezeichen" aria-label="Emoji: Rotes Ausrufezeichen">not a good look in late CKD https://abs.twimg.com/emoji/v2/... draggable="false" alt="❗️" title="Rotes Ausrufezeichen" aria-label="Emoji: Rotes Ausrufezeichen">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="❗️" title="Rotes Ausrufezeichen" aria-label="Emoji: Rotes Ausrufezeichen">
“So what happens?”
When these CKD patients come in with hyperglycaemia it is MUCH easier for them to meet the biochemical criteria for calculated hyperosmolality
= lots of IV fluids (+-insulin) if HHS protocol is started inappropriately
4/
“But it’s not the guidelines fault that urea is raising tonicity and risking fluids shifts in these CKD patients?”
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="❌" title="Kreuzzeichen" aria-label="Emoji: Kreuzzeichen"> Except it doesn’t
https://abs.twimg.com/emoji/v2/... draggable="false" alt="❌" title="Kreuzzeichen" aria-label="Emoji: Kreuzzeichen"> Except it doesn’t
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="❌" title="Kreuzzeichen" aria-label="Emoji: Kreuzzeichen"> No, it really doesn’t in anybody
https://abs.twimg.com/emoji/v2/... draggable="false" alt="❌" title="Kreuzzeichen" aria-label="Emoji: Kreuzzeichen"> No, it really doesn’t in anybody
Let’s quickly detour via the concept of effective and ineffective osmoles https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">
“But it’s not the guidelines fault that urea is raising tonicity and risking fluids shifts in these CKD patients?”
Let’s quickly detour via the concept of effective and ineffective osmoles
5/
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Na = effective osmole = it contributes to fluid shifts
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Na = effective osmole = it contributes to fluid shifts
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> The sum has ‘2Na’ to simplify for equal number of effective anions (mostly Cl & HCO3)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> The sum has ‘2Na’ to simplify for equal number of effective anions (mostly Cl & HCO3)
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Glucose can’t get into cells in absence of (enough) insulin, so also exerts pull on water in HHS
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Glucose can’t get into cells in absence of (enough) insulin, so also exerts pull on water in HHS
Plug: @TheSkeletonKG case8
Plug: @TheSkeletonKG case8
6/
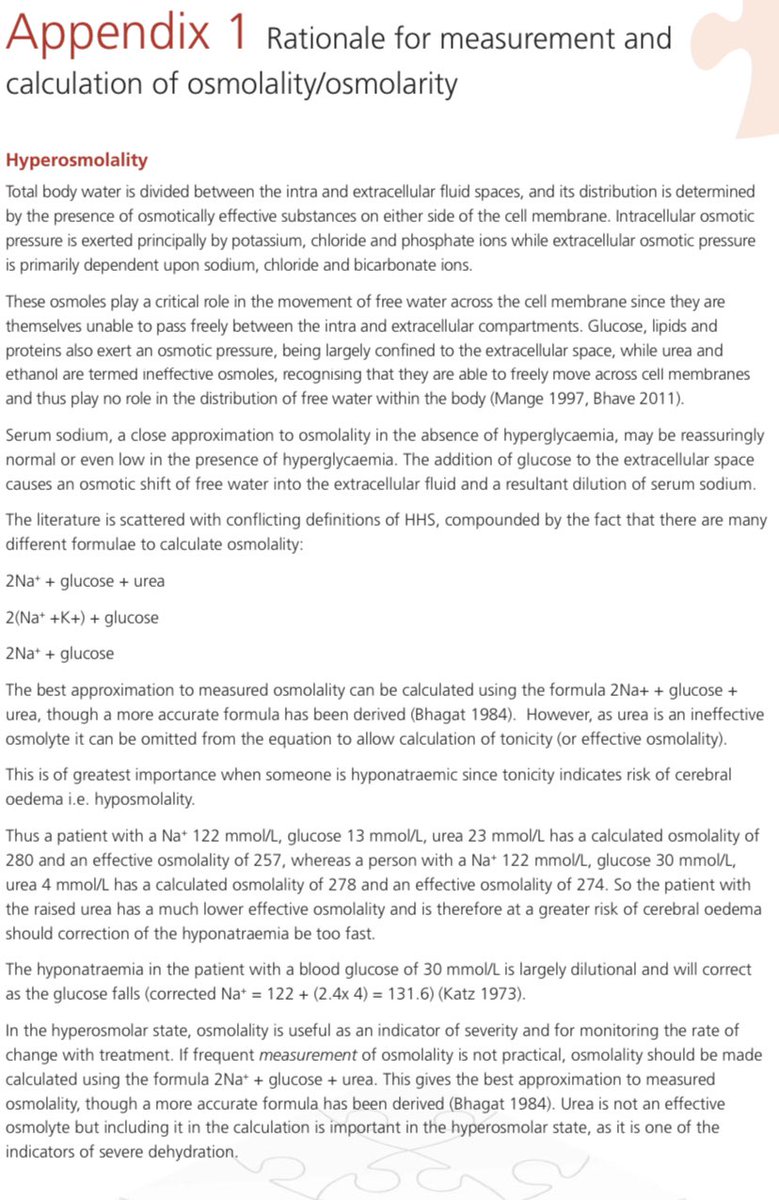
However, unlike glucose and sodium,
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Mittelgroßer Stern" aria-label="Emoji: Mittelgroßer Stern">urea is an ineffective osmole
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Mittelgroßer Stern" aria-label="Emoji: Mittelgroßer Stern">urea is an ineffective osmole https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Mittelgroßer Stern" aria-label="Emoji: Mittelgroßer Stern">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Mittelgroßer Stern" aria-label="Emoji: Mittelgroßer Stern">
This means that urea:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> moves quickly & freely across cell membranes
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> moves quickly & freely across cell membranes
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> won’t contribute to raising extracellular tonicity
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> won’t contribute to raising extracellular tonicity
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> won’t cause the fluid shifts we fear in HHS (in CKD or pre-renal states)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> won’t cause the fluid shifts we fear in HHS (in CKD or pre-renal states)
However, unlike glucose and sodium,
This means that urea:
7/
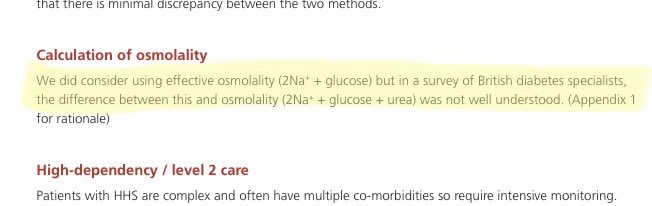
“So why include urea in the calculation?”
They justify inclusion by saying https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">urea is an “indicator of severe dehydration”.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">urea is an “indicator of severe dehydration”.
So they think it’s worth having a marker of disease severity in the formula, & in patients with normal baseline urea who look dry & sick, that’s fine.
“So why include urea in the calculation?”
They justify inclusion by saying
So they think it’s worth having a marker of disease severity in the formula, & in patients with normal baseline urea who look dry & sick, that’s fine.
8/
But though this ‘dehydration marker’ argument is fine for most patients, it falls apart in advanced CKD (a not uncommon condition for patients in and out with high blood sugars to have)
It also doesn’t work in other causes of https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">urea that aren’t hypovolaemia
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">urea that aren’t hypovolaemia
Plug: @BukuRenal https://twitter.com/bukurenal/status/1306500678790123520">https://twitter.com/bukurenal...
But though this ‘dehydration marker’ argument is fine for most patients, it falls apart in advanced CKD (a not uncommon condition for patients in and out with high blood sugars to have)
It also doesn’t work in other causes of
Plug: @BukuRenal https://twitter.com/bukurenal/status/1306500678790123520">https://twitter.com/bukurenal...
9/
“So given urea is an ineffective osmole, why not just use effective osmolality = 2Na + Glucose instead?”
This is where they slip in a reason which is a slightly devastating critique of UK diabetologists within their own HHS guidelines (and I’m sure not true!)
“So given urea is an ineffective osmole, why not just use effective osmolality = 2Na + Glucose instead?”
This is where they slip in a reason which is a slightly devastating critique of UK diabetologists within their own HHS guidelines (and I’m sure not true!)
10/
To be fair the guideline discourages using biochemistry alone & also stresses the hypovolaemic diagnostic criteria
BUT
A concern is that the clinical diagnosis of hypovolaemia has large inter-observer variability, & I’ve seen doctors focus effort on the calculation instead
To be fair the guideline discourages using biochemistry alone & also stresses the hypovolaemic diagnostic criteria
BUT
A concern is that the clinical diagnosis of hypovolaemia has large inter-observer variability, & I’ve seen doctors focus effort on the calculation instead
11/
Take home points:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔸" title="Kleine orangene Raute" aria-label="Emoji: Kleine orangene Raute"> If you calculate osmolality in HHS including urea you’re using it as a ‘dehydration severity marker’
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔸" title="Kleine orangene Raute" aria-label="Emoji: Kleine orangene Raute"> If you calculate osmolality in HHS including urea you’re using it as a ‘dehydration severity marker’
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔸" title="Kleine orangene Raute" aria-label="Emoji: Kleine orangene Raute"> But when urea is simply at it’s high baseline this is illogical, & you decrease diagnostic specificity in a group at high risk of treatment harm
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔸" title="Kleine orangene Raute" aria-label="Emoji: Kleine orangene Raute"> But when urea is simply at it’s high baseline this is illogical, & you decrease diagnostic specificity in a group at high risk of treatment harm
Take home points:
Fin/
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔸" title="Kleine orangene Raute" aria-label="Emoji: Kleine orangene Raute">Starting HHS protocols is risky given the large IV fluid volumes: in advanced CKD always discuss early with specialists
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔸" title="Kleine orangene Raute" aria-label="Emoji: Kleine orangene Raute">Starting HHS protocols is risky given the large IV fluid volumes: in advanced CKD always discuss early with specialists
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔸" title="Kleine orangene Raute" aria-label="Emoji: Kleine orangene Raute">Guidelines should note calculation limitations & exclusions (& expect us to be able to learn the difference between effective & ineffective osmoles!)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔸" title="Kleine orangene Raute" aria-label="Emoji: Kleine orangene Raute">Guidelines should note calculation limitations & exclusions (& expect us to be able to learn the difference between effective & ineffective osmoles!)

 Read on Twitter
Read on Twitter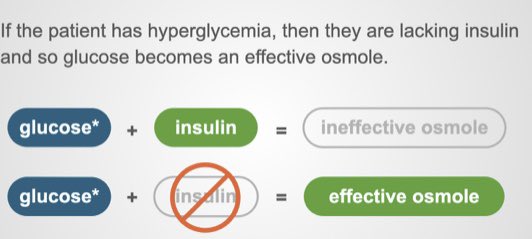 Na = effective osmole = it contributes to fluid shiftshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> The sum has ‘2Na’ to simplify for equal number of effective anions (mostly Cl & HCO3)https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Glucose can’t get into cells in absence of (enough) insulin, so also exerts pull on water in HHSPlug: @TheSkeletonKG case8" title="5/https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Na = effective osmole = it contributes to fluid shiftshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> The sum has ‘2Na’ to simplify for equal number of effective anions (mostly Cl & HCO3)https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Glucose can’t get into cells in absence of (enough) insulin, so also exerts pull on water in HHSPlug: @TheSkeletonKG case8" class="img-responsive" style="max-width:100%;"/>
Na = effective osmole = it contributes to fluid shiftshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> The sum has ‘2Na’ to simplify for equal number of effective anions (mostly Cl & HCO3)https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Glucose can’t get into cells in absence of (enough) insulin, so also exerts pull on water in HHSPlug: @TheSkeletonKG case8" title="5/https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Na = effective osmole = it contributes to fluid shiftshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> The sum has ‘2Na’ to simplify for equal number of effective anions (mostly Cl & HCO3)https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Glucose can’t get into cells in absence of (enough) insulin, so also exerts pull on water in HHSPlug: @TheSkeletonKG case8" class="img-responsive" style="max-width:100%;"/>
 urea is an “indicator of severe dehydration”.So they think it’s worth having a marker of disease severity in the formula, & in patients with normal baseline urea who look dry & sick, that’s fine." title="7/“So why include urea in the calculation?”They justify inclusion by saying https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">urea is an “indicator of severe dehydration”.So they think it’s worth having a marker of disease severity in the formula, & in patients with normal baseline urea who look dry & sick, that’s fine." class="img-responsive" style="max-width:100%;"/>
urea is an “indicator of severe dehydration”.So they think it’s worth having a marker of disease severity in the formula, & in patients with normal baseline urea who look dry & sick, that’s fine." title="7/“So why include urea in the calculation?”They justify inclusion by saying https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">urea is an “indicator of severe dehydration”.So they think it’s worth having a marker of disease severity in the formula, & in patients with normal baseline urea who look dry & sick, that’s fine." class="img-responsive" style="max-width:100%;"/>