I& #39;m seeing more and more suggestions that groups at low risk of COVID-19 should go back to normal while high risk groups are protected. What would the logical implications of this be? 1/
First, let& #39;s pick an example definition of risk. If we use infection fatality risk alone for simplicity (which of course isn& #39;t only measure of severity), there is a clear age pattern, which rises above ~0.1% around age 50 and above ~1% around age 70 ( https://www.medrxiv.org/content/10.1101/2020.08.24.20180851v1)">https://www.medrxiv.org/content/1... 2/
Suppose hypothetically we define the over 65 age group as & #39;high risk& #39;. That& #39;s about 18% of the UK population, and doesn& #39;t include others with health conditions that put them at more at risk of severe COVID. 3/
The question, therefore, would be how to prevent any large outbreak among & #39;low risk& #39; groups from spreading into & #39;high risk& #39; ones without shutting these risk groups out of society for several months or more (if that were even feasible). 4/
There have been attempts to have & #39;shielding& #39; of risk groups (either explicitly or implicitly) in many countries. But large epidemics have still tended to result in infection in these groups, because not all transmission routes were prevented. 5/
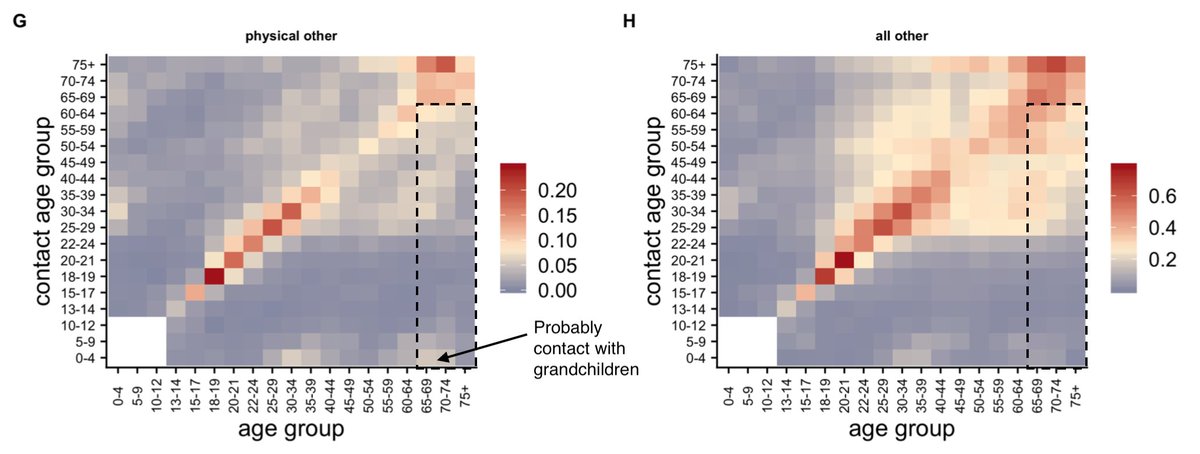
For context, here& #39;s data on pre-COVID social contacts between different age groups in UK outside home/work/school (from: https://www.medrxiv.org/content/10.1101/2020.02.16.20023754v2).">https://www.medrxiv.org/content/1... Dashed box shows over 65s reporting contacts with under 65s. 6/
So in this hypothetical example, how to prevent contacts in the box from spreading infection into the over 65s? Removing interactions in that box would be removing a large part of people& #39;s lives, but could the contacts be made less risky? 7/
One option would be to use rapid testing to make sure that these contacts are not infectious, e.g. testing attendees ahead of events/venues/gatherings. But remember, 18% of population are over 65, so that& #39;s a lot of (low risk) contacts who would need to be tested regularly. 8/
Then there& #39;s the question of what happens if contacts are positive... Would they need to self-isolate? People might well do anyway if they knew they& #39;re infected, which could reduce wider transmission... 9/
Depending on what % of population is defined as at high risk, and how many contacts are tested regularly and isolate, could well get a situation where measures reduce transmission in the low risk groups too, leading to a low reproduction number. 10/
If this were to happen, it may become equivalent to a light-touch suppression approach via mass testing: https://twitter.com/AdamJKucharski/status/1303245754853658624?s=20">https://twitter.com/AdamJKuch... 11/
It wouldn& #39;t be the first example of a situation where we start with two different approaches but end up with similar outcomes: https://twitter.com/AdamJKucharski/status/1292861098971070467?s=20">https://twitter.com/AdamJKuch... 12/

 Read on Twitter
Read on Twitter