#ISA2020 Yesterday: Plenery Session on Diagnosis and Management of AL #amyloidosis chaired by @awechalekar and Stefan Schönland. Here is my take home message @AmyloidosisSupp @Amyloidosisfdn @Amyloidosis_ARC @AmyloidC @MayoAmyloid @amyloid_papers
@ADispenzieri talked about Diagnosis and work-up. Fat pad biopsy and bone marrow biopsy are able to determine the diagnosis of AL in 50-79%. In those cases an organ biospy is not necessary
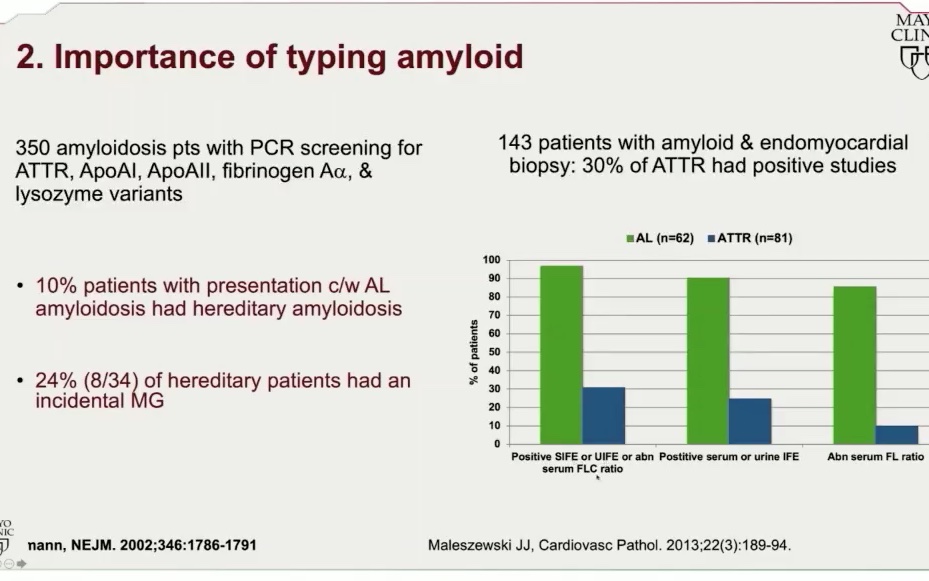
@ADispenzieri at #ISA2020: 10 % of patients with Congo Red+ amyloid detection have TTR Amyloidosis and elevated FLC--> you need to determine the diagnosis by mass spec or IHC
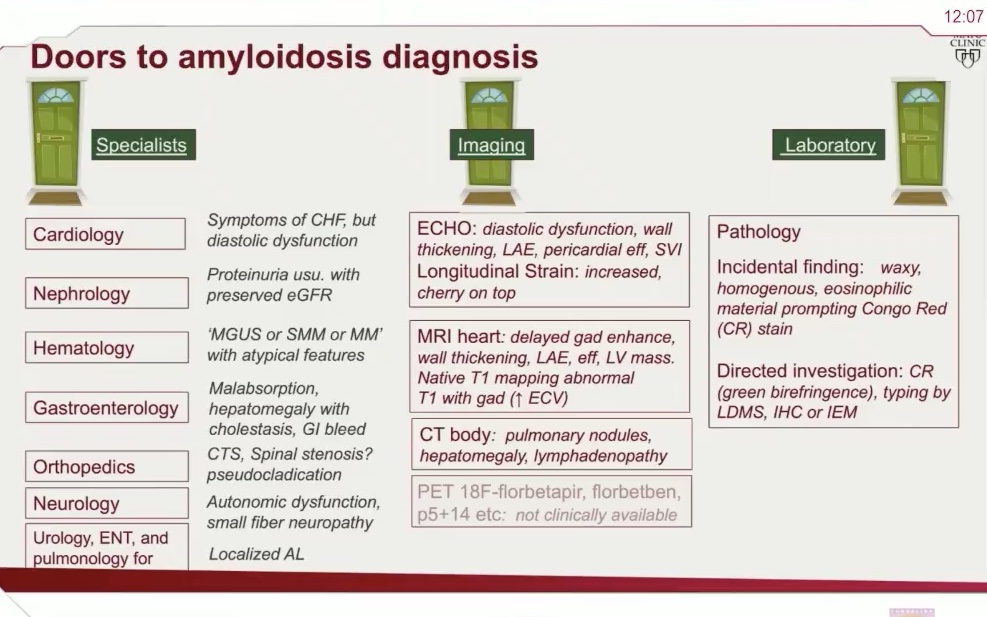
@ADispenzieri at #ISA2020: Clinical presentation of AL is very heterogenous --> look for the "Doors to amyloidosis diagnosis" with symptoms such as spinal stenosis, hepatomegaly or pseudoclaudication
Dr Hegenbart at #ISA2020 pointed out RED FLAGS  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🚩" title="Dreieckige Fahne an einem Pfosten" aria-label="Emoji: Dreieckige Fahne an einem Pfosten">for AL #amyloidosis and suggested NT-proBNP for all patients with MGUS and elevated Free Light Chins. NT-proBNP can detect cardiac involvement before symptoms of heart failure occur in 20% of patients.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🚩" title="Dreieckige Fahne an einem Pfosten" aria-label="Emoji: Dreieckige Fahne an einem Pfosten">for AL #amyloidosis and suggested NT-proBNP for all patients with MGUS and elevated Free Light Chins. NT-proBNP can detect cardiac involvement before symptoms of heart failure occur in 20% of patients.
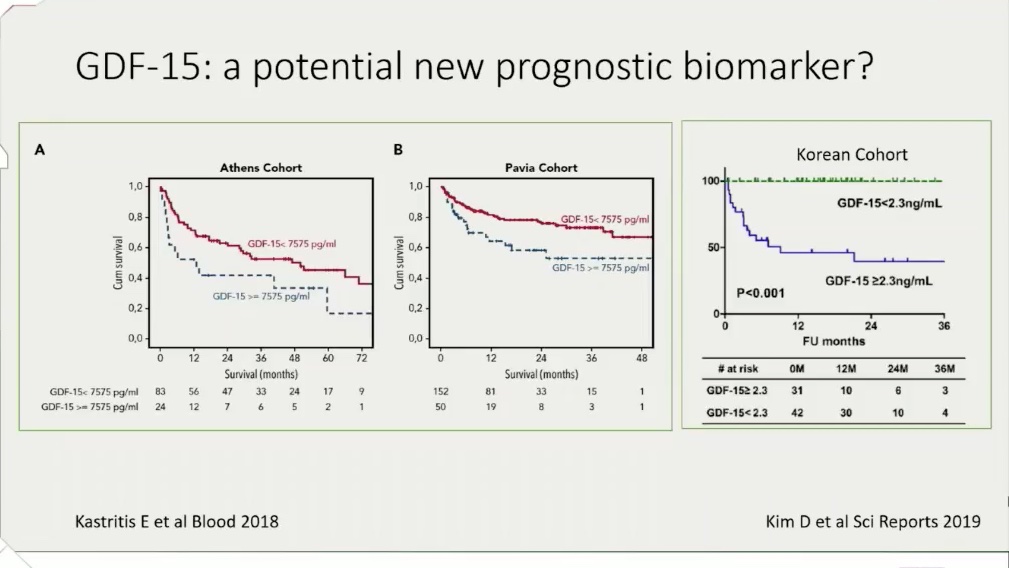
Dr Kastritis presented at #ISA2020 data to use Growth Differentiation Factor-15 (GDF-15) as an independent prognostic marker for survival and renal outcomes in (AL) Amyloidosis
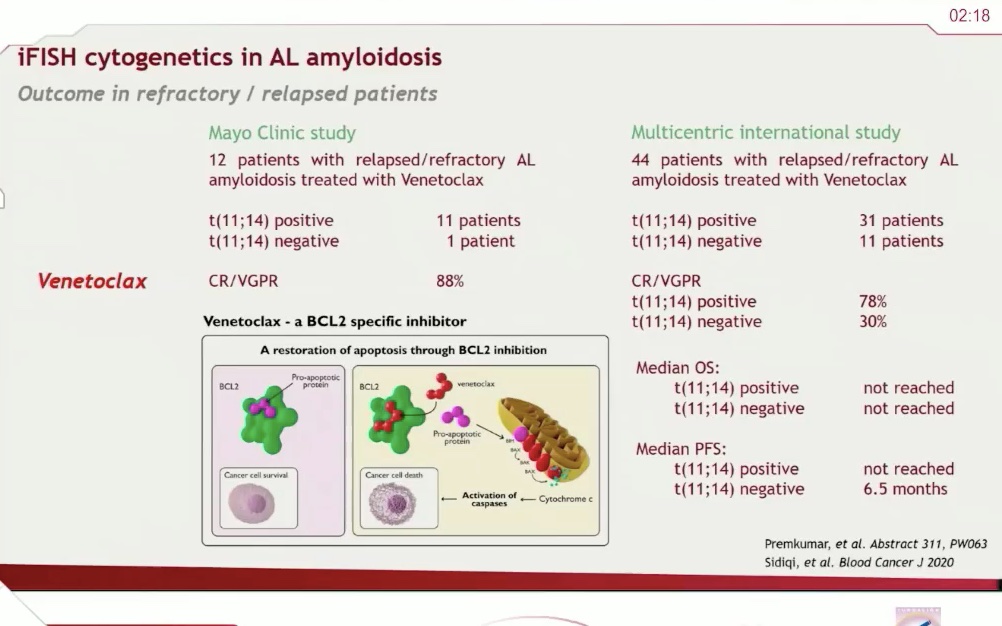
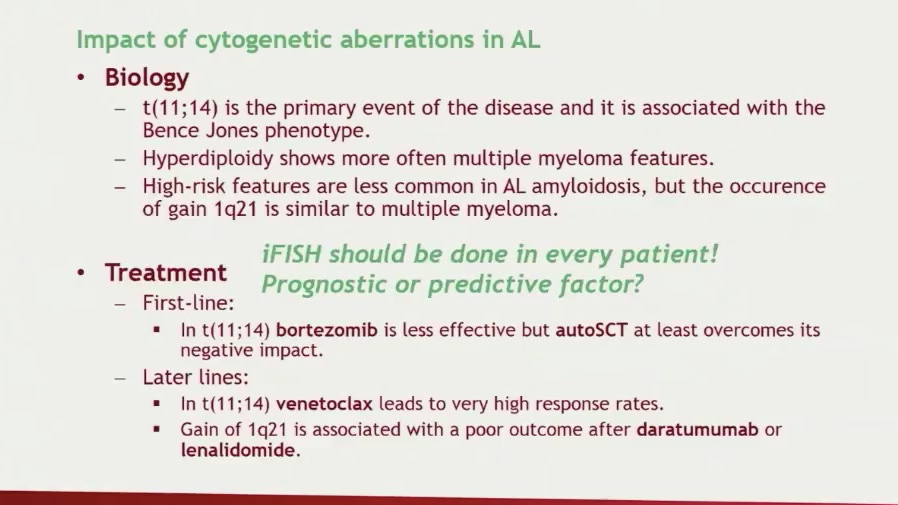
Dr Schönland at #ISA2020 t(11;14) is a negative prognostic marker for AL patients treated with bortezomib but a positive prognostic marker for patients receiving ASCT  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤔" title="Denkendes Gesicht" aria-label="Emoji: Denkendes Gesicht">ASCT for all patients with t(11;14)?
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤔" title="Denkendes Gesicht" aria-label="Emoji: Denkendes Gesicht">ASCT for all patients with t(11;14)?
Dr Schönland at #ISA2020 cytogenetic aberration impact prognosis in AL --> 1q21 gain has poorer prognosis in AL similar to MM. In t(11;14)consider venetoclax ASAP
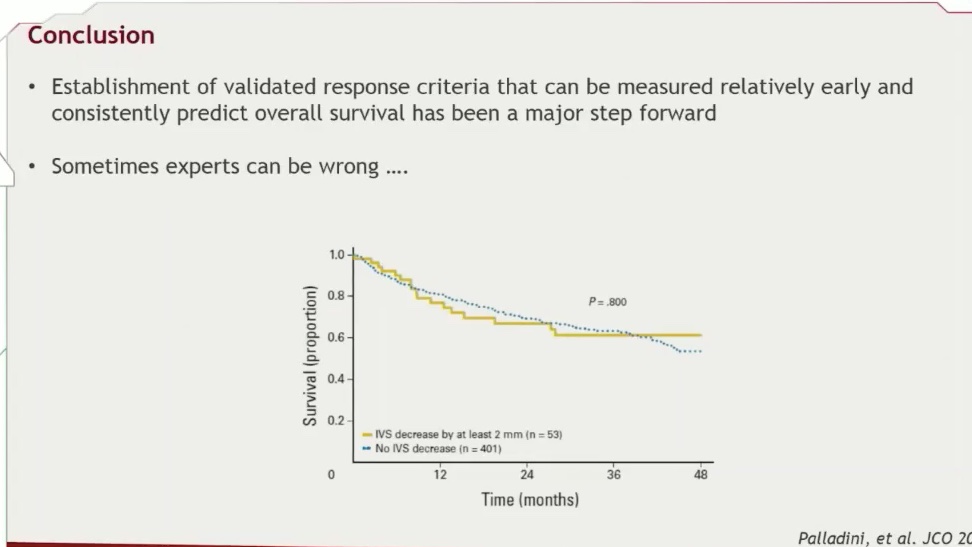
Dr Palladini at #ISA2020 stated that decrease in IVS does not correlate with OS--> and should not ne used for organ response!
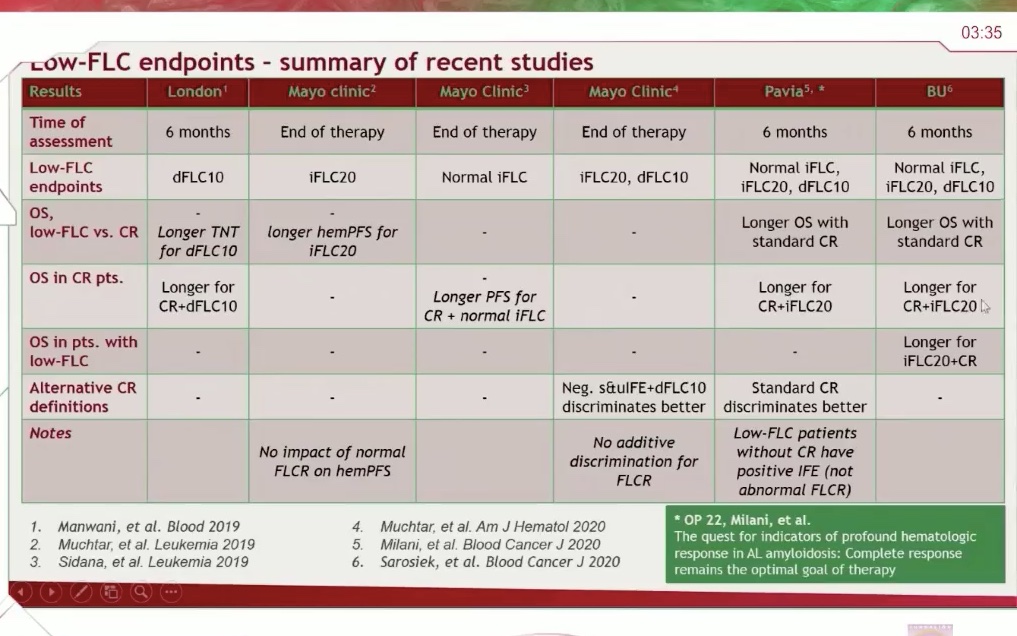
Dr Palladini at #ISA2020 summarised the goal for hematologic response--> Goal should be dFLC 10 or iFLC 20. Do not use FLC ratio in AL Amyloidosis

 Read on Twitter
Read on Twitter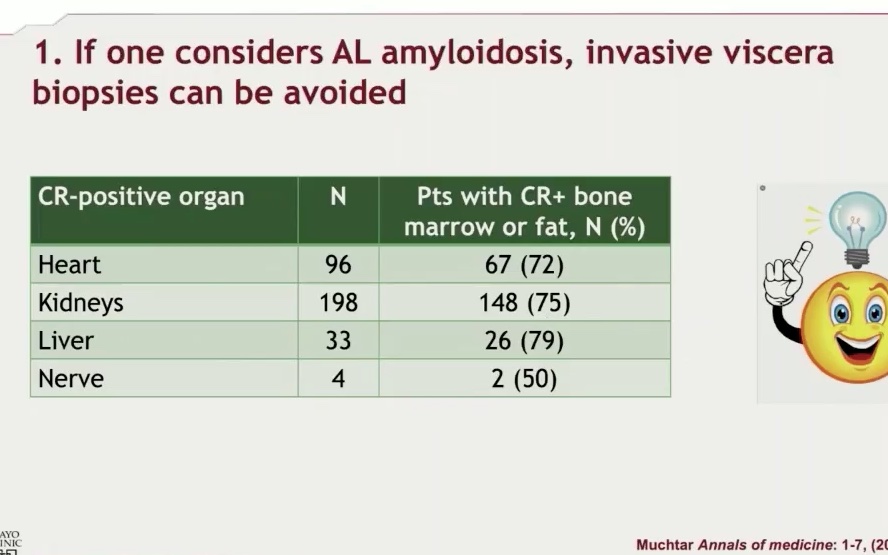
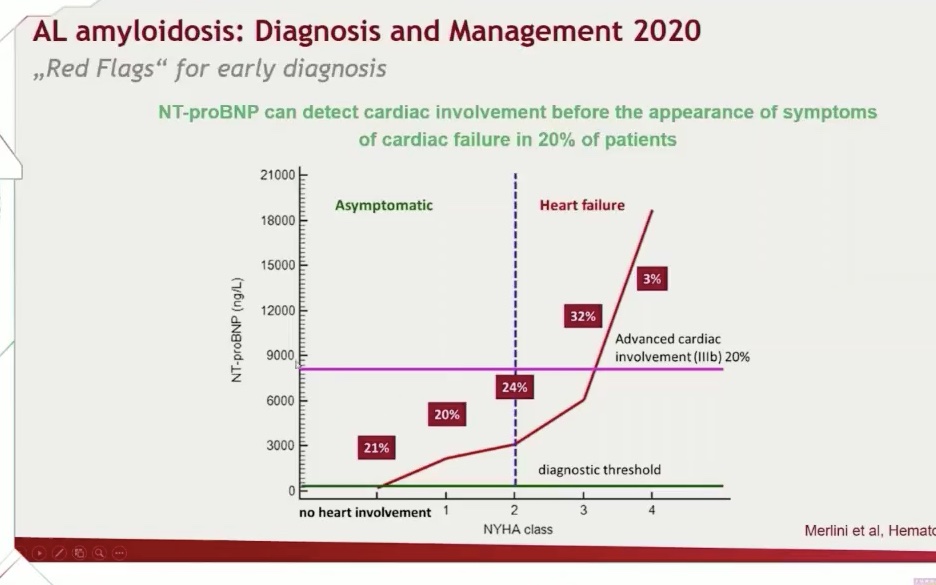 for AL #amyloidosis and suggested NT-proBNP for all patients with MGUS and elevated Free Light Chins. NT-proBNP can detect cardiac involvement before symptoms of heart failure occur in 20% of patients." title="Dr Hegenbart at #ISA2020 pointed out RED FLAGS https://abs.twimg.com/emoji/v2/... draggable="false" alt="🚩" title="Dreieckige Fahne an einem Pfosten" aria-label="Emoji: Dreieckige Fahne an einem Pfosten">for AL #amyloidosis and suggested NT-proBNP for all patients with MGUS and elevated Free Light Chins. NT-proBNP can detect cardiac involvement before symptoms of heart failure occur in 20% of patients.">
for AL #amyloidosis and suggested NT-proBNP for all patients with MGUS and elevated Free Light Chins. NT-proBNP can detect cardiac involvement before symptoms of heart failure occur in 20% of patients." title="Dr Hegenbart at #ISA2020 pointed out RED FLAGS https://abs.twimg.com/emoji/v2/... draggable="false" alt="🚩" title="Dreieckige Fahne an einem Pfosten" aria-label="Emoji: Dreieckige Fahne an einem Pfosten">for AL #amyloidosis and suggested NT-proBNP for all patients with MGUS and elevated Free Light Chins. NT-proBNP can detect cardiac involvement before symptoms of heart failure occur in 20% of patients.">
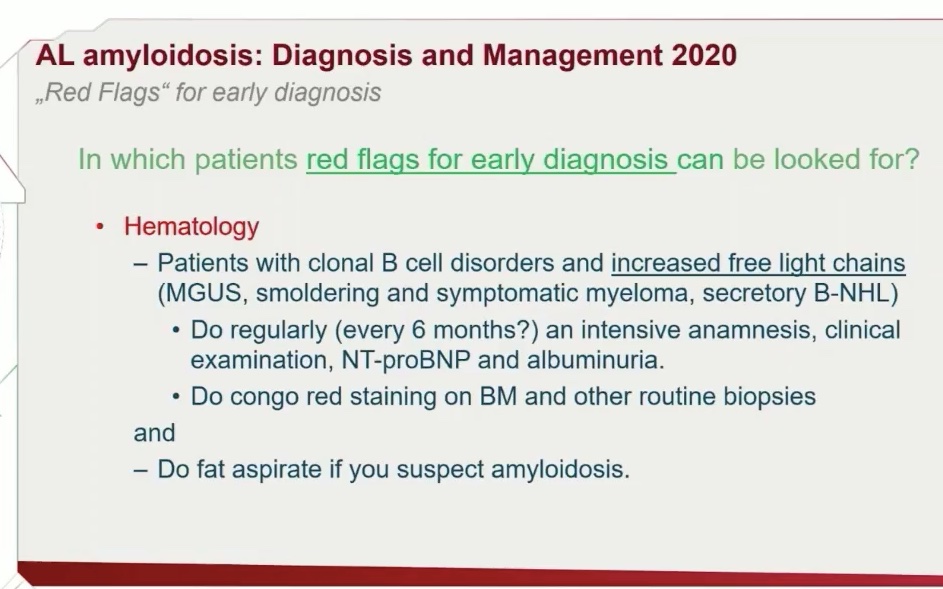 for AL #amyloidosis and suggested NT-proBNP for all patients with MGUS and elevated Free Light Chins. NT-proBNP can detect cardiac involvement before symptoms of heart failure occur in 20% of patients." title="Dr Hegenbart at #ISA2020 pointed out RED FLAGS https://abs.twimg.com/emoji/v2/... draggable="false" alt="🚩" title="Dreieckige Fahne an einem Pfosten" aria-label="Emoji: Dreieckige Fahne an einem Pfosten">for AL #amyloidosis and suggested NT-proBNP for all patients with MGUS and elevated Free Light Chins. NT-proBNP can detect cardiac involvement before symptoms of heart failure occur in 20% of patients.">
for AL #amyloidosis and suggested NT-proBNP for all patients with MGUS and elevated Free Light Chins. NT-proBNP can detect cardiac involvement before symptoms of heart failure occur in 20% of patients." title="Dr Hegenbart at #ISA2020 pointed out RED FLAGS https://abs.twimg.com/emoji/v2/... draggable="false" alt="🚩" title="Dreieckige Fahne an einem Pfosten" aria-label="Emoji: Dreieckige Fahne an einem Pfosten">for AL #amyloidosis and suggested NT-proBNP for all patients with MGUS and elevated Free Light Chins. NT-proBNP can detect cardiac involvement before symptoms of heart failure occur in 20% of patients.">
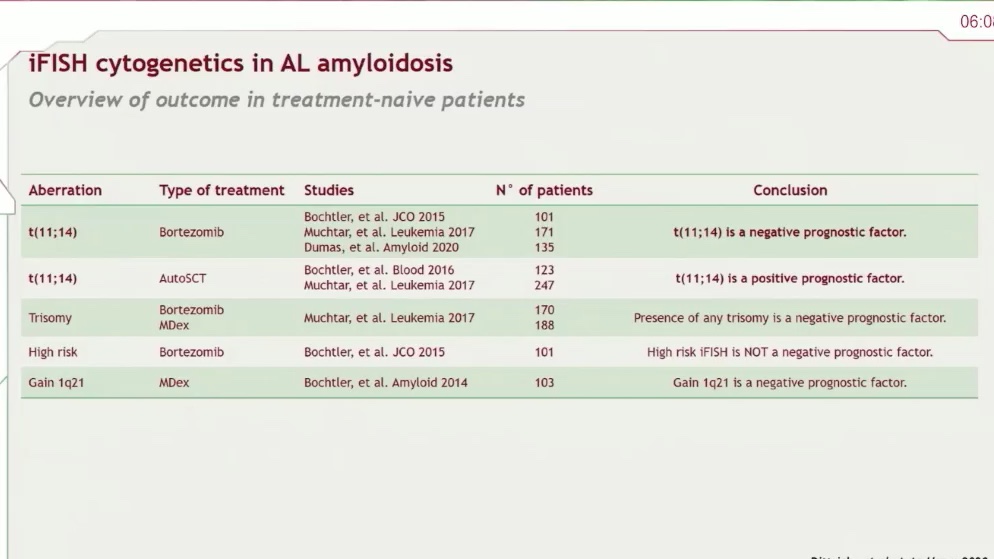 ASCT for all patients with t(11;14)?" title="Dr Schönland at #ISA2020 t(11;14) is a negative prognostic marker for AL patients treated with bortezomib but a positive prognostic marker for patients receiving ASCT https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤔" title="Denkendes Gesicht" aria-label="Emoji: Denkendes Gesicht">ASCT for all patients with t(11;14)?" class="img-responsive" style="max-width:100%;"/>
ASCT for all patients with t(11;14)?" title="Dr Schönland at #ISA2020 t(11;14) is a negative prognostic marker for AL patients treated with bortezomib but a positive prognostic marker for patients receiving ASCT https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤔" title="Denkendes Gesicht" aria-label="Emoji: Denkendes Gesicht">ASCT for all patients with t(11;14)?" class="img-responsive" style="max-width:100%;"/>