1/ #medtwitter #tweetorial Raise your hand if you have ever inappropriately checked an ammonia level. https://abs.twimg.com/emoji/v2/... draggable="false" alt="🙋" title="Glückliche Person, die eine Hand hebt" aria-label="Emoji: Glückliche Person, die eine Hand hebt">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🙋" title="Glückliche Person, die eine Hand hebt" aria-label="Emoji: Glückliche Person, die eine Hand hebt">
1. Why is ammonia https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> in liver failure and how is this connected w/ encephalopathy?
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> in liver failure and how is this connected w/ encephalopathy?
2. When should levels be checked?
3. Aside from cirrhosis, what other conditions https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">ammonia?
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">ammonia?
1. Why is ammonia
2. When should levels be checked?
3. Aside from cirrhosis, what other conditions
2/ Ammonia is primarily produced by bacteria w/ urease enz in intestines but is also produced in muscle and the kidneys.
Table source: https://www.ccjm.org/content/76/4/252">https://www.ccjm.org/content/7...
Table source: https://www.ccjm.org/content/76/4/252">https://www.ccjm.org/content/7...
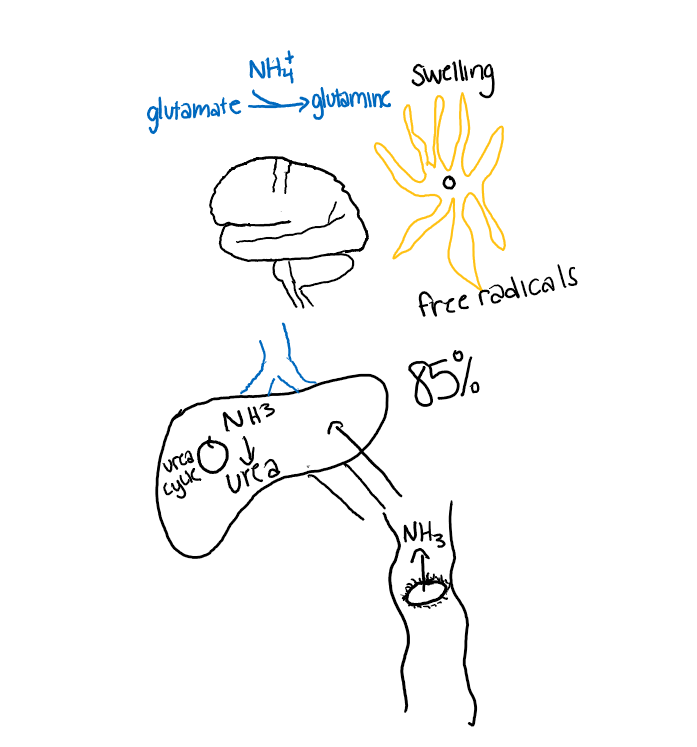
3/ 85% of ammonia is cleared by the liver through the urea cycle. 15% is cleared by muscle/kidneys. If the ammonia (/other nitrogenous waste) not metabolized it passes through the blood brain barrier glutamate>glutamine> astrocyte swelling and free radicals>encephalopathy.
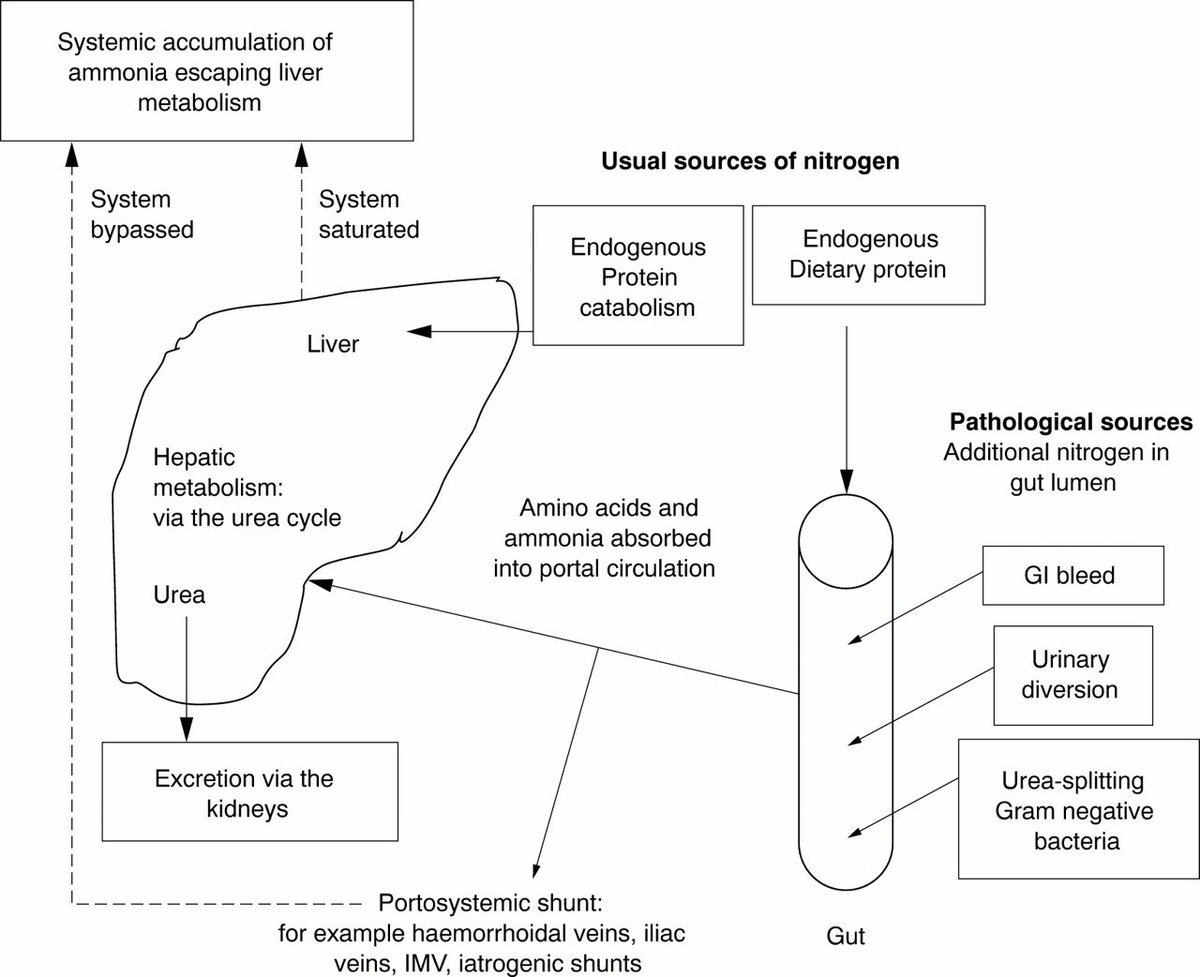
4/ Ammonia can build up though  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">production,
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">production,  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">clearance, or combo. In both acute or chronic liver failure,
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">clearance, or combo. In both acute or chronic liver failure,  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> urea cycle
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> urea cycle  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> ammonia production. Portosystemic shunting can also
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> ammonia production. Portosystemic shunting can also  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> ammonia since less passes though liver (why TIPS
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> ammonia since less passes though liver (why TIPS  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> risk of encephalopathy).
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> risk of encephalopathy).
5/ You might be thinking based on above that if a patient comes in with cirrhosis, you should check an ammonia level to evaluate for HE However, there are several reasons why HE is a clinical diagnosis.
6/I will discuss some of the reasons outlined in these two articles which I highly suggest reading:
https://www.journalofhospitalmedicine.com/jhospmed/article/143598/hospital-medicine/ammonia-levels-and-hepatic-encephalopathy-patients-known">https://www.journalofhospitalmedicine.com/jhospmed/... https://jamanetwork.com/journals/jama/article-abstract/1895229">https://jamanetwork.com/journals/...
https://www.journalofhospitalmedicine.com/jhospmed/article/143598/hospital-medicine/ammonia-levels-and-hepatic-encephalopathy-patients-known">https://www.journalofhospitalmedicine.com/jhospmed/... https://jamanetwork.com/journals/jama/article-abstract/1895229">https://jamanetwork.com/journals/...
7/Ammonia is a difficult test to obtain. You may have tried to add this lab test on and been dismayed when you saw it required a new draw. Using a tourniquet can falsely  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> values as can
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> values as can https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> time prior to processing. The collected sample also has to be place on ice.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> time prior to processing. The collected sample also has to be place on ice.
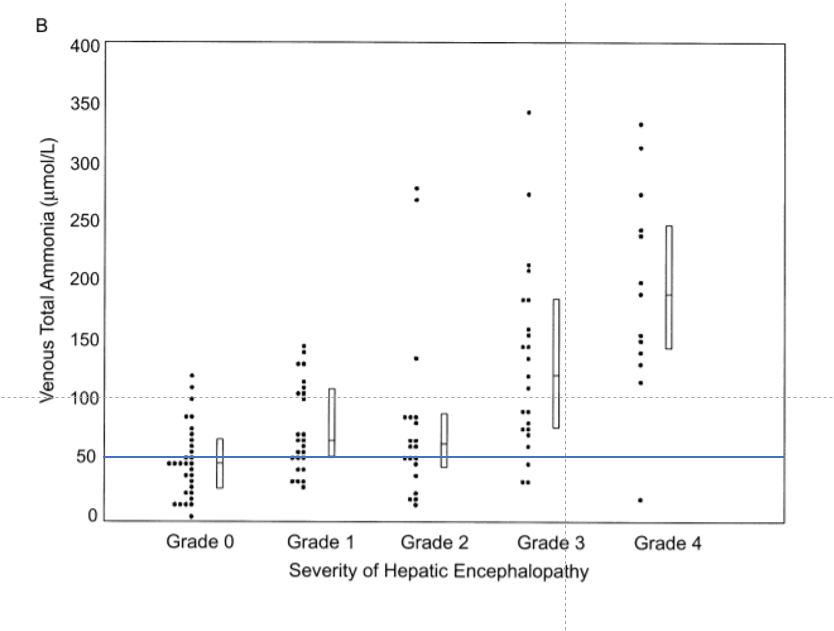
8/ In this study from 2003, arterial and venous ammonia levels where obtained to assess correlation with samples and degree of encephalopathy. There was a correleation between venous/arterial sample and degree of encephalopahy r = 0.56 for venous. https://pubmed.ncbi.nlm.nih.gov/12637132/ ">https://pubmed.ncbi.nlm.nih.gov/12637132/...
9/ The problem? The ULN for ammonia was 47 in this study. I used a cut off of 50 for ease. If you look at the sample a significant amount of pts with HE had normal ammonia levels and a significant amount w/o HE had  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> ammonia levels.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> ammonia levels.
10/Another paper found that blood ammonia levels had a diagnostic accuracy of 59%, sensitivity 47%, specifity 78%. It certainly should not be used as a screening test as you would miss over 1/2 of cases of HE. https://pubmed.ncbi.nlm.nih.gov/23293201/ ">https://pubmed.ncbi.nlm.nih.gov/23293201/...
11/A recent propensity matched study showed that in cirrhotic pts w/ HE that lactulose dose was the same regardless of ammonia level. This points to the fact we likely are not using ammonia level to guide mng. Why check a lab you don& #39;t need? https://pubmed.ncbi.nlm.nih.gov/31658104/ ">https://pubmed.ncbi.nlm.nih.gov/31658104/...
12/ Although not helpful in cirrhosis, checking ammonia levels can be helpful in acute liver failure as  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> levels are associated with worse prognosis. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1856380/">https://www.ncbi.nlm.nih.gov/pmc/artic...
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> levels are associated with worse prognosis. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1856380/">https://www.ncbi.nlm.nih.gov/pmc/artic...
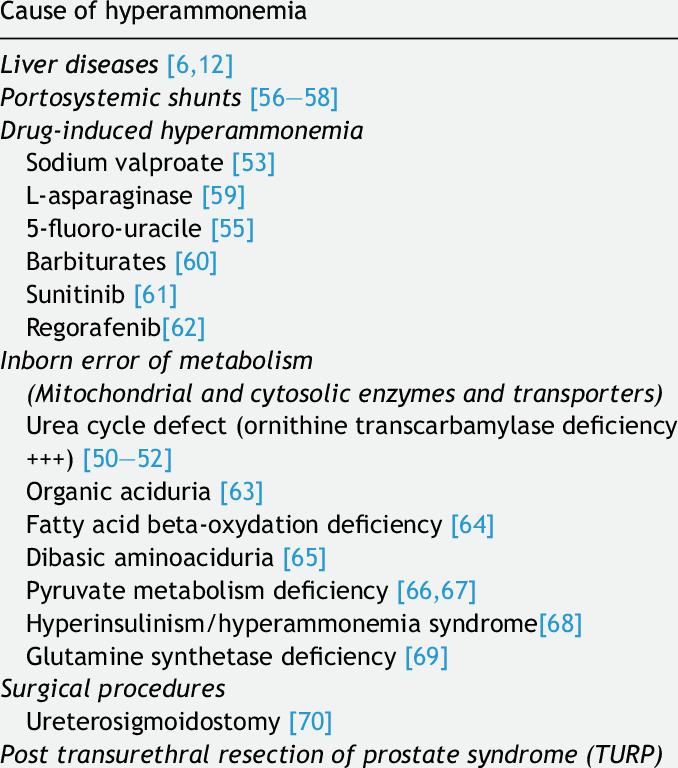
13/There are situations aside from liver failure in which ammonia  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">
1. Drug toxicity including valproic acid & chemo meds
2. Urea cycle disorder
3. Glycerin toxicity- historically caused TURP syndrome (now rarely used)
Table source: https://pubmed.ncbi.nlm.nih.gov/29551609/ ">https://pubmed.ncbi.nlm.nih.gov/29551609/...
1. Drug toxicity including valproic acid & chemo meds
2. Urea cycle disorder
3. Glycerin toxicity- historically caused TURP syndrome (now rarely used)
Table source: https://pubmed.ncbi.nlm.nih.gov/29551609/ ">https://pubmed.ncbi.nlm.nih.gov/29551609/...
4. SIBO with dehydration
14/ 4. SIBO with dehydration
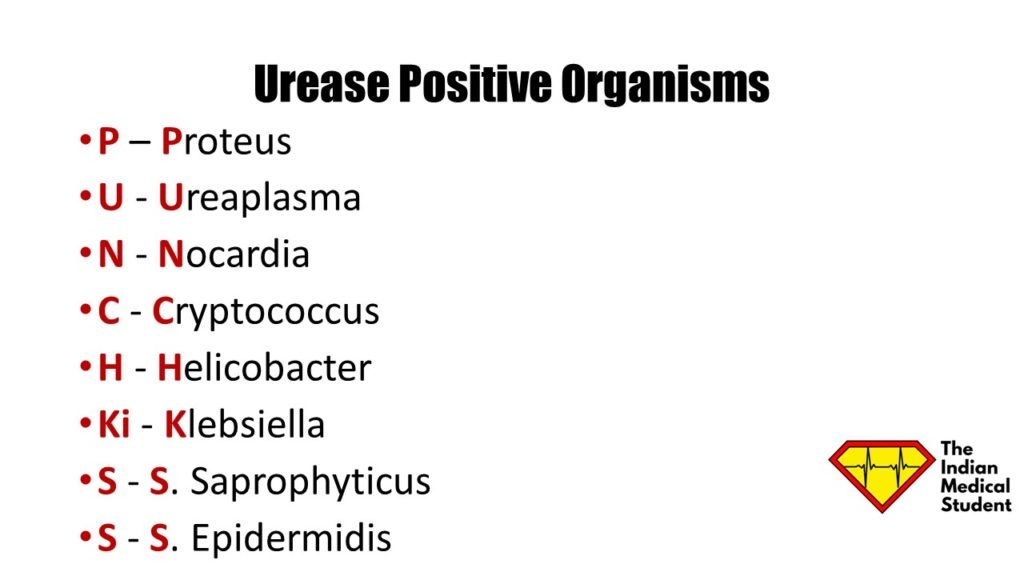
5. Urease producing organisms including Ureaplasma urealyticum in an immunocompromised host https://academic.oup.com/ofid/article/6/3/ofz033/5371475
Mnemonic">https://academic.oup.com/ofid/arti... source: https://theindianmedicalstudent.com/3-mnemonics-for-urease-positive-organisms-tonic-mnemonics-for-clonic-teens/">https://theindianmedicalstudent.com/3-mnemoni...
5. Urease producing organisms including Ureaplasma urealyticum in an immunocompromised host https://academic.oup.com/ofid/article/6/3/ofz033/5371475
Mnemonic">https://academic.oup.com/ofid/arti... source: https://theindianmedicalstudent.com/3-mnemonics-for-urease-positive-organisms-tonic-mnemonics-for-clonic-teens/">https://theindianmedicalstudent.com/3-mnemoni...
15/Checking an ammonia level in these situations is helpful because it may guide specific treatment. Valproic acid can cause  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> ammonia leading to AMS w/o liver failure or supratherapeutic levels. Being aware of it is important b/c treated w/ carnitine . https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5536406/">https://www.ncbi.nlm.nih.gov/pmc/artic...
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> ammonia leading to AMS w/o liver failure or supratherapeutic levels. Being aware of it is important b/c treated w/ carnitine . https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5536406/">https://www.ncbi.nlm.nih.gov/pmc/artic...
16/Conclusions:
1. While https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> ammonia is common in cirrhosis, HE is a clinical diagnosis. Ammonia has poor sensitivity/specificity and diagnostic accuracy and has not been shown to change treatment of HE in cirrhosis.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> ammonia is common in cirrhosis, HE is a clinical diagnosis. Ammonia has poor sensitivity/specificity and diagnostic accuracy and has not been shown to change treatment of HE in cirrhosis.
2. https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">Ammonia can have prognostic implications in ALF.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">Ammonia can have prognostic implications in ALF.
1. While
2.
17/ 3. Other conditions such as drug toxicity (especially valproic acid), urea cycle disorder, and certain bacterial infections can also cause  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> ammonia. It may be helpful to check ammonia levels in these conditions b/c it may change managment. /end
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> ammonia. It may be helpful to check ammonia levels in these conditions b/c it may change managment. /end
On related note, just saw this case report of 3 cases of non-hepatic hyperammonaemia with this great diagram.
https://pmj.bmj.com/content/77/913/717">https://pmj.bmj.com/content/7...
https://pmj.bmj.com/content/77/913/717">https://pmj.bmj.com/content/7...

 Read on Twitter
Read on Twitter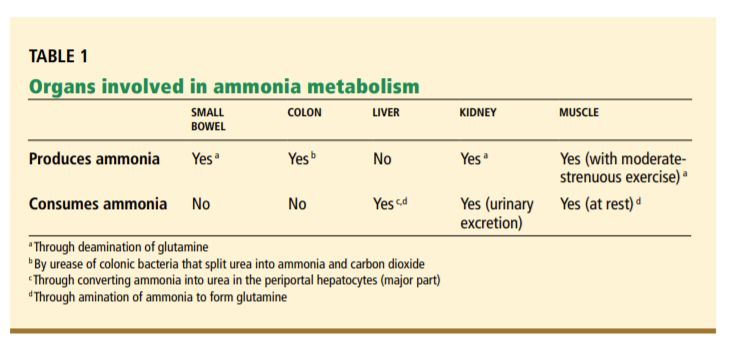
 ammonia levels." title="9/ The problem? The ULN for ammonia was 47 in this study. I used a cut off of 50 for ease. If you look at the sample a significant amount of pts with HE had normal ammonia levels and a significant amount w/o HE had https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> ammonia levels." class="img-responsive" style="max-width:100%;"/>
ammonia levels." title="9/ The problem? The ULN for ammonia was 47 in this study. I used a cut off of 50 for ease. If you look at the sample a significant amount of pts with HE had normal ammonia levels and a significant amount w/o HE had https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> ammonia levels." class="img-responsive" style="max-width:100%;"/>
 1. Drug toxicity including valproic acid & chemo meds2. Urea cycle disorder3. Glycerin toxicity- historically caused TURP syndrome (now rarely used)Table source: https://pubmed.ncbi.nlm.nih.gov/29551609/..." title="13/There are situations aside from liver failure in which ammonia https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">1. Drug toxicity including valproic acid & chemo meds2. Urea cycle disorder3. Glycerin toxicity- historically caused TURP syndrome (now rarely used)Table source: https://pubmed.ncbi.nlm.nih.gov/29551609/..." class="img-responsive" style="max-width:100%;"/>
1. Drug toxicity including valproic acid & chemo meds2. Urea cycle disorder3. Glycerin toxicity- historically caused TURP syndrome (now rarely used)Table source: https://pubmed.ncbi.nlm.nih.gov/29551609/..." title="13/There are situations aside from liver failure in which ammonia https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">1. Drug toxicity including valproic acid & chemo meds2. Urea cycle disorder3. Glycerin toxicity- historically caused TURP syndrome (now rarely used)Table source: https://pubmed.ncbi.nlm.nih.gov/29551609/..." class="img-responsive" style="max-width:100%;"/>