We had two preprints out last week. They might seem unrelated, but have lots to do with each other. In this thread I will outline the results and what they have to do with recent discussions around testing. @JHIDDynamics
https://doi.org/10.1101/2020.09.02.20186916
https://doi.org/10.1101/2... href=" https://doi.org/10.1101/2020.09.01.20182469
(1/16)">https://doi.org/10.1101/2...
https://doi.org/10.1101/2020.09.02.20186916
(1/16)">https://doi.org/10.1101/2...
First, a shout out to all the folks who worked hard on these papers: @qifangb @andrewazman @khgrantz @ymax @lucystats @qhanlee @CJEMetcalf @EmilyGurley3
Also, note these have not been peer reviewed, so use caution in interpretation. (2/16)
Also, note these have not been peer reviewed, so use caution in interpretation. (2/16)
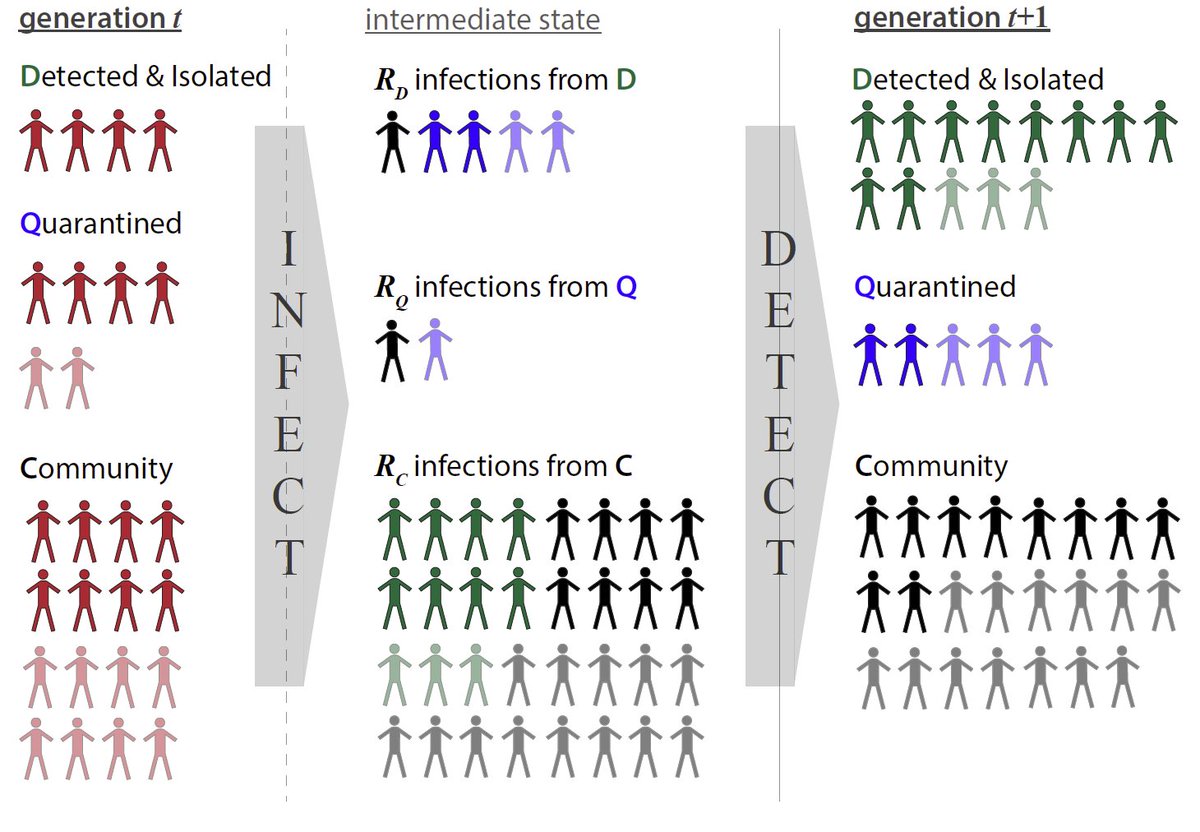
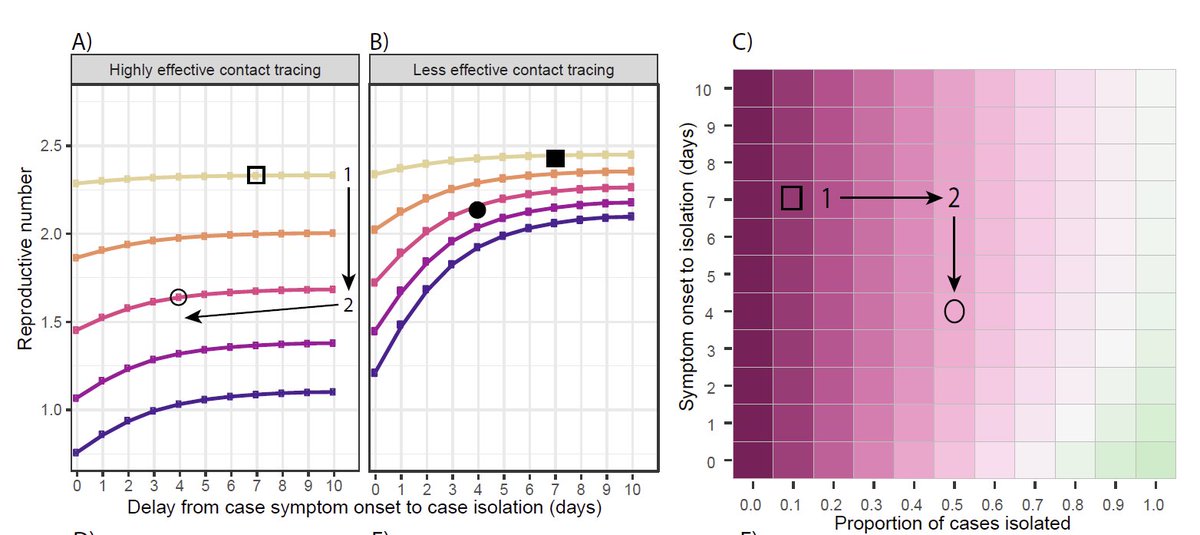
The first paper ( https://doi.org/10.1101/2020.09.01.20182469)">https://doi.org/10.1101/2... presents the algorithms behind the ConTESSA app ( https://www.iddynamics.jhsph.edu/apps/connect/contessa)">https://www.iddynamics.jhsph.edu/apps/conn... aimed to help evaluate contact tracing programs. (3/16)
The big message: if you don’t capture enough cases from the untraced population, speed and coverage of contact tracing programs don’t have a huge impact. Those community cases are the seeds from which every other part of a test-trace-isolate program springs. (4/16)
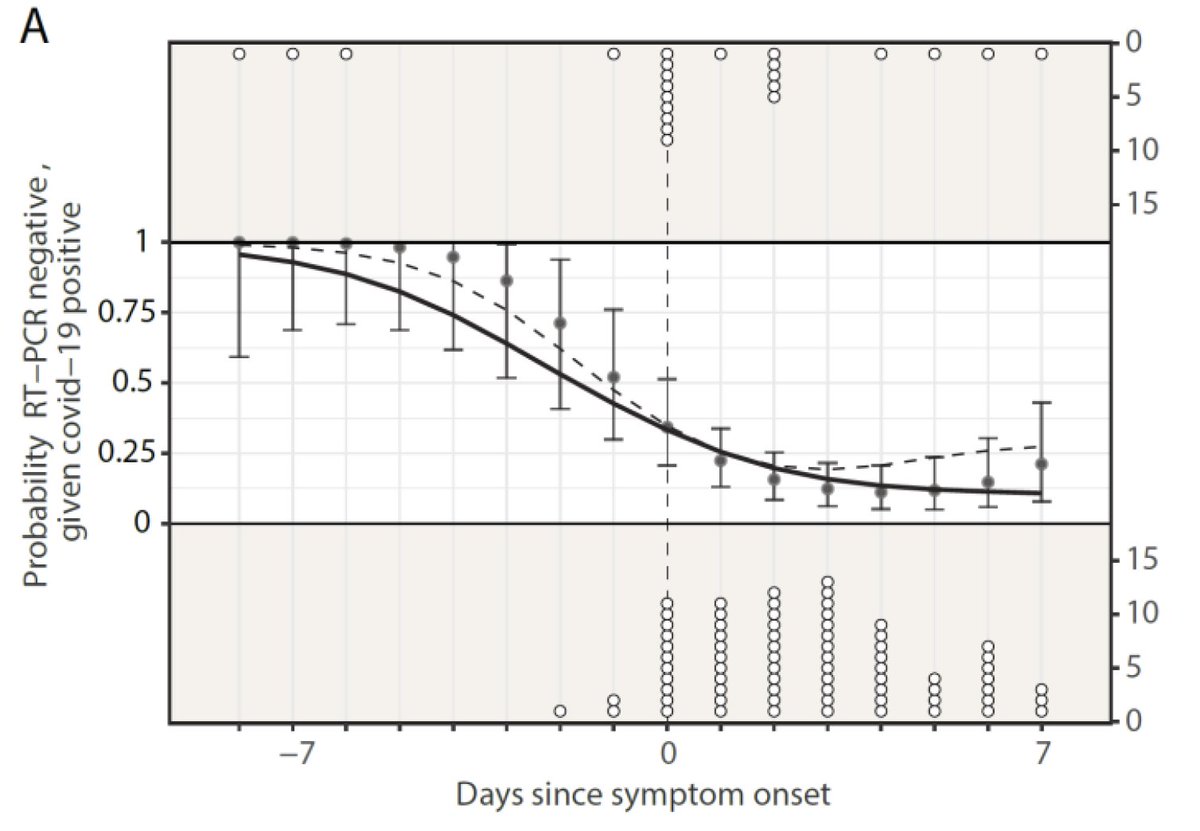
One big factor in capturing those seeds is the sensitivity of testing protocols. The 2nd paper uses serological data to understand the practical performance of RT-PCR in Shenzhen China. Punchline: even a rigorous protocol missed 1/3 of infections:
https://doi.org/10.1101/2020.09.01.20182469
(5/16)">https://doi.org/10.1101/2...
https://doi.org/10.1101/2020.09.01.20182469
(5/16)">https://doi.org/10.1101/2...
This paper brings new estimates of RT-PCR performance (see earlier work https://dx.doi.org/10.7326%2FM20-1495)">https://dx.doi.org/10.7326%2... over the course of the infection. The picture looks a bit better for RT-PCR, but the pattern of a test that is imperfect, particularly early in the course of infection remains (6/16)
So what does all this mean for how we think about testing? Particularly recent debates around changing @CDCgov recommendations, and claims in @nytimes that maybe some positive tests “shouldn’t be” https://www.nytimes.com/2020/08/29/health/coronavirus-testing.html?ocid=uxbndlbing">https://www.nytimes.com/2020/08/2... (7/16)
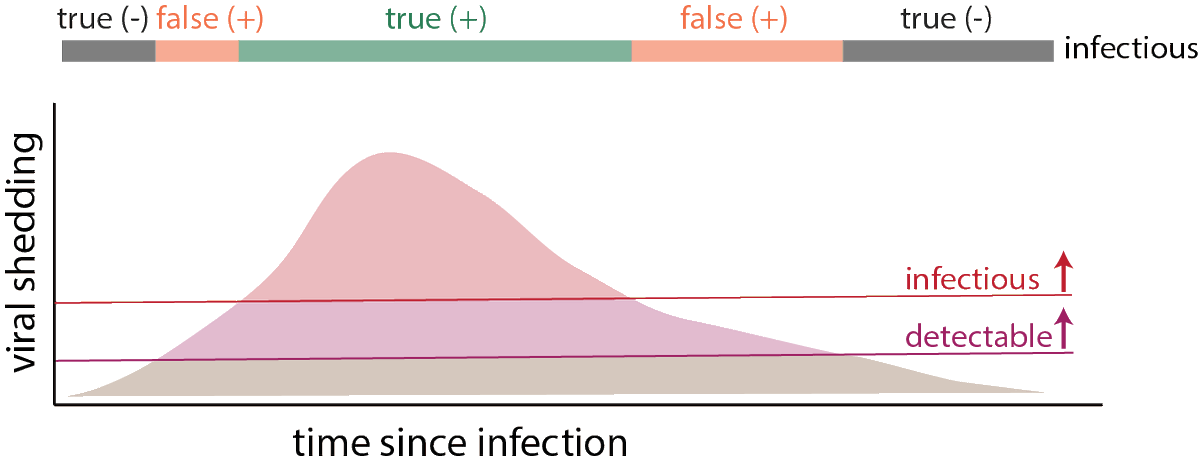
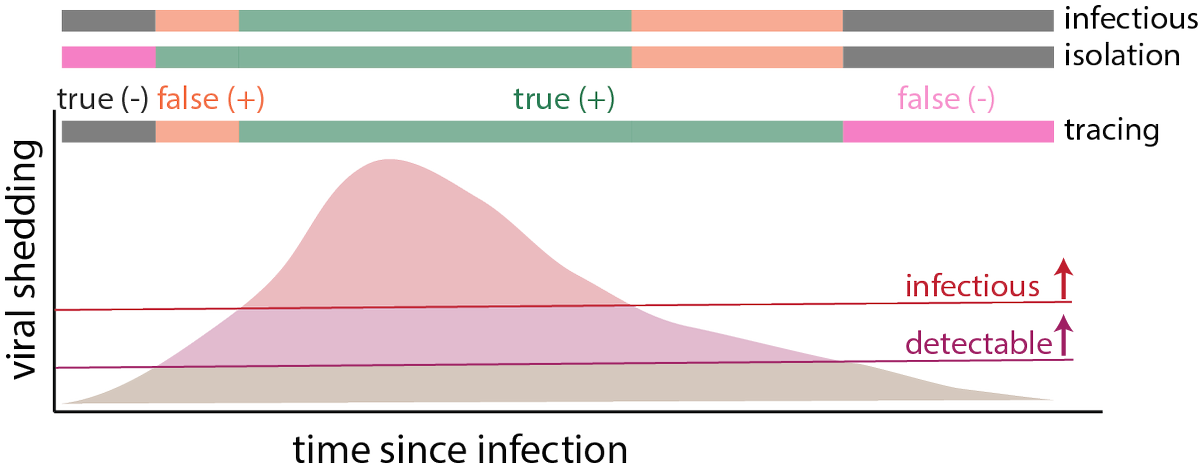
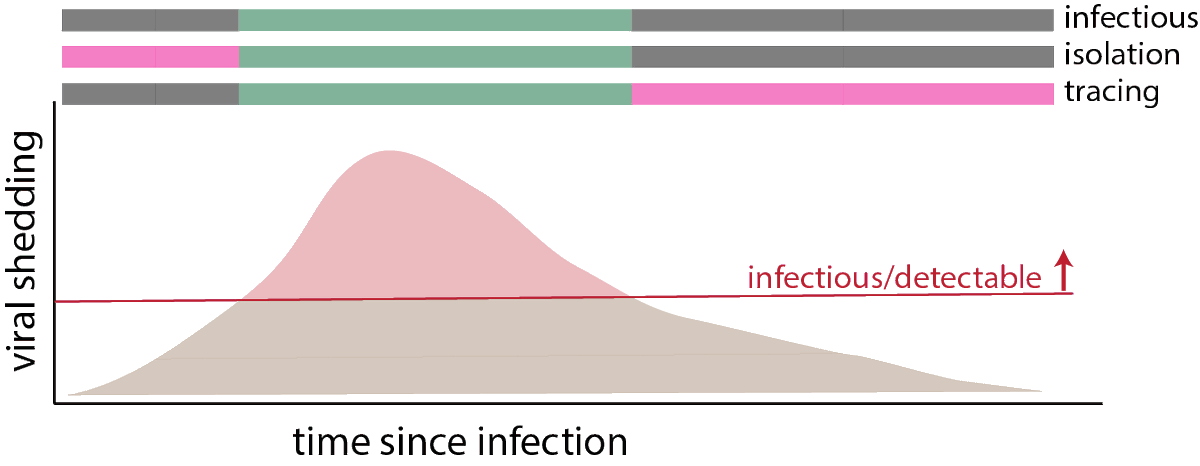
It is helpful to think about an idealized course of illness, and how infectivity and test performance vary. It is a simplification, but assume there is some threshold of viral shedding over which a test can detect the virus, and a higher one for infectiousness. (8/16)
Testing is a tool. When we want it to be positive depends on how we use it. If we want to find people who are infectious right now, then we only care about the time above the infectiousness threshold. A positive test any other time is a “false positive” for this purpose (9/16)
If want to get people in isolation as soon as possible so they do not transmit to others, then any positive test during or before infectiousness is a true positive, and any negative test then is a false negative. Positive tests after infectiousness are “false” positives (10/16)
If we are interested in tracing people who a case may have infected and getting them into quarantine, then positive tests after infectiousness are true positives, and those before are false. Negatives after infection are “false negatives” (11/16)
If we make a test less sensitive, so those testing positive are more likely to be infectious, we get rid of all the false positives, but really increase the chances of false negatives if we are interested in isolation or contact tracing (12/16)
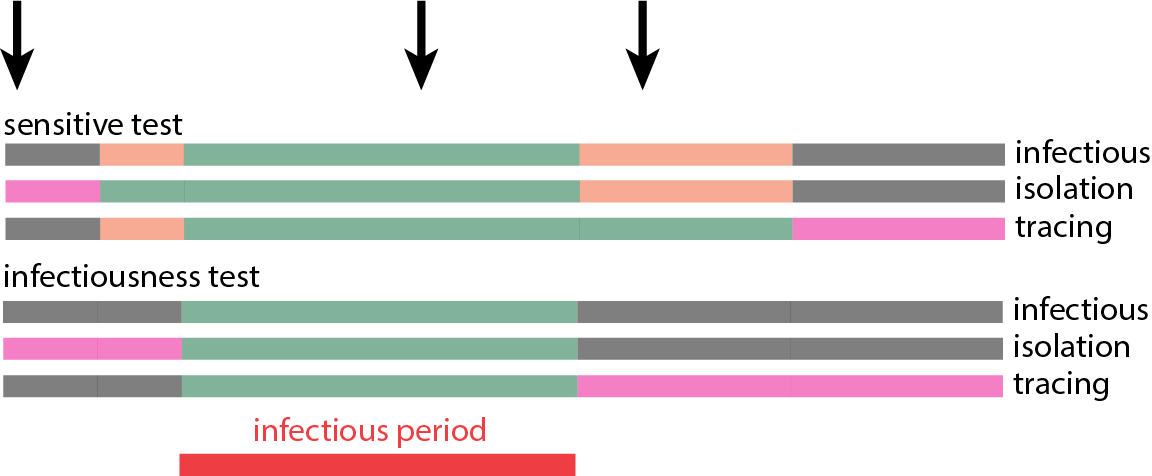
I think about this is in terms of productive an unproductive interventions. If people are only tested occasionally shrinking the period they would test positive eliminates unproductive interventions, but at the expense of missed opportunities the intervene productively (13/16)
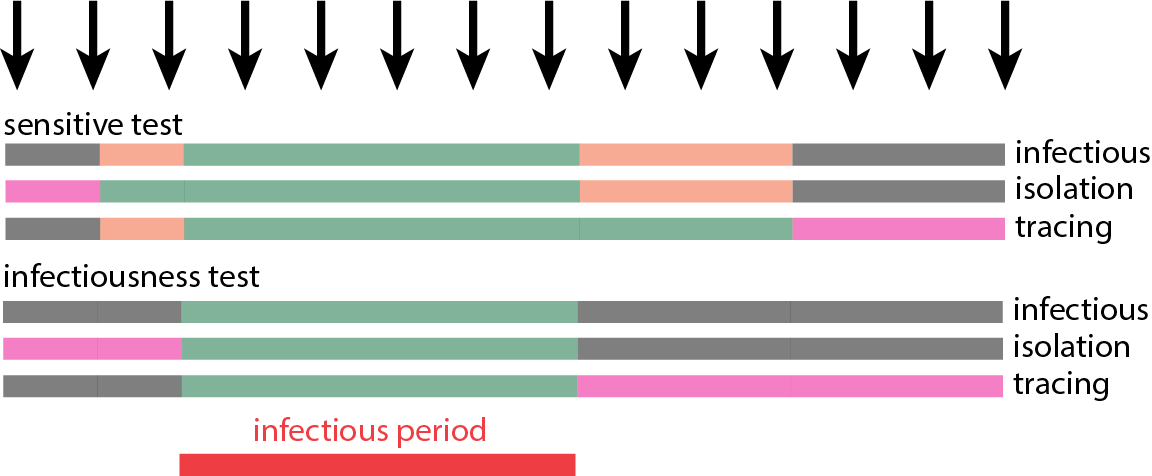
But this problem goes away if use of our less sensitive test allows us to test frequently…so we can still hit that infectious period (but beware false positives) (14/16)
It is worth noting that there may be some people who will never get to the infectious threshold, and for them all positive tests are “false”. One big question is: are the 1/3 of people missed by PCR but caught by serology in Shenzhen all in this group? (15/16)
Bringing it back around. Testing is a tool, and we show even our best version (PCR) is imperfect. If our goal is disease control, its all about getting people into isolation and quarantine. So, we should be cautious about lowering sensitivity unless we can test more often(16/16)

 Read on Twitter
Read on Twitter