Pleased to finally present this work! Large (n=1130), global (67 countries) case-control study of exposures associated with HCP illness with COVID-19. Granular look at workplace exposures with respirator vs. medical mask data. https://pubmed.ncbi.nlm.nih.gov/32900402/
Three">https://pubmed.ncbi.nlm.nih.gov/32900402/... main findings: a https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧵" title="Thread" aria-label="Emoji: Thread">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧵" title="Thread" aria-label="Emoji: Thread">
Three">https://pubmed.ncbi.nlm.nih.gov/32900402/... main findings: a
1.1
Considered “risky” by most: AGPs on COVID patients. AGPs not associated with infection in this work (OR 0.9)
Considered “risky” by most: AGPs on COVID patients. AGPs not associated with infection in this work (OR 0.9)
1.2
Considered “risky” by many: work on wards enriched with COVID patients (COVID units) or sicker COVID patients (ICUs, COVID ICUs). These areas associated with lower likelihood of HCP infection than work on regular hospital ward (ORs 0.5-0.7 vs. OR 1.4).
Considered “risky” by many: work on wards enriched with COVID patients (COVID units) or sicker COVID patients (ICUs, COVID ICUs). These areas associated with lower likelihood of HCP infection than work on regular hospital ward (ORs 0.5-0.7 vs. OR 1.4).
1.3
ORs are modest, but 2 implications:
1) Shift focus to “lower risk” areas less familiar with PPE / COVID protocols?
2) COVID care including AGPs can be confidently performed (w/o waiting for negative tests? Looking at you, trachs in some hospitals) with appropriate PPE.
ORs are modest, but 2 implications:
1) Shift focus to “lower risk” areas less familiar with PPE / COVID protocols?
2) COVID care including AGPs can be confidently performed (w/o waiting for negative tests? Looking at you, trachs in some hospitals) with appropriate PPE.
1.4
These data also suggest PPE is generally quite effective. Of note: HCPs who were always observed donning/doffing PPE by dedicated observers had OR 0.4 for infection compared to no PPE observers. Potentially actionable result!
These data also suggest PPE is generally quite effective. Of note: HCPs who were always observed donning/doffing PPE by dedicated observers had OR 0.4 for infection compared to no PPE observers. Potentially actionable result!
2.1
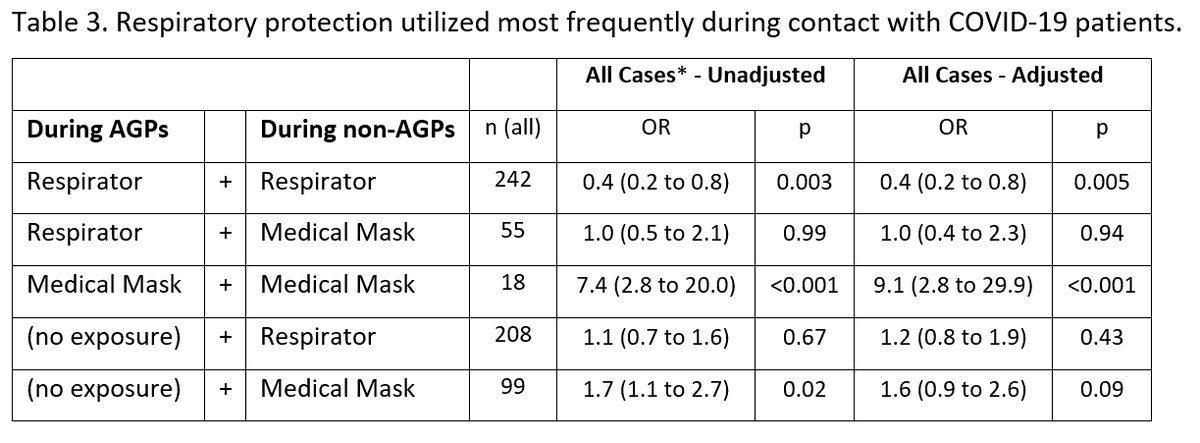
Respirators vs. medical masks for COVID pt contact has been a hot topic ever since ‘AGP’ became a household acronym. When this manuscript was drafted, there were no real-world COVID-specific data on respirators vs. masks re: risk of HCP infection. Maybe still the case?
Respirators vs. medical masks for COVID pt contact has been a hot topic ever since ‘AGP’ became a household acronym. When this manuscript was drafted, there were no real-world COVID-specific data on respirators vs. masks re: risk of HCP infection. Maybe still the case?
2.2
Respirators clearly protective during AGPs (OR 0.4). In non-AGP contact, medical masks were associated with higher likelihood of infection only in situations of prolonged (>45 min) continuous COVID patient contact.
Respirators clearly protective during AGPs (OR 0.4). In non-AGP contact, medical masks were associated with higher likelihood of infection only in situations of prolonged (>45 min) continuous COVID patient contact.
2.3
This finding, plus lower likelihood of HCP infection with negative pressure room use (OR 0.4), provides additional evidence for a more nuanced view of the droplet vs. aerosol debate. Hard to distill this down further, pertinent paragraph attached.
This finding, plus lower likelihood of HCP infection with negative pressure room use (OR 0.4), provides additional evidence for a more nuanced view of the droplet vs. aerosol debate. Hard to distill this down further, pertinent paragraph attached.
2.4
Acknowledging inherent limitations, a randomized or cluster randomized trial of respirator vs. mask for non-AGP contact, similar to prior influenza trials, would be most informative on this topic. Quick search yields one in the works: https://clinicaltrials.gov/ct2/show/NCT04296643">https://clinicaltrials.gov/ct2/show/...
Acknowledging inherent limitations, a randomized or cluster randomized trial of respirator vs. mask for non-AGP contact, similar to prior influenza trials, would be most informative on this topic. Quick search yields one in the works: https://clinicaltrials.gov/ct2/show/NCT04296643">https://clinicaltrials.gov/ct2/show/...
3.1
Finally, most workplace ORs for HCP infection were modest, but ORs for non-work exposures were not! Ill household member (OR 3.8), gatherings >10 (OR 4.6), patronizing restaurant/bar (OR 16.2), public transport (OR 4.4) all registered. Remain vigilant outside the workplace.
Finally, most workplace ORs for HCP infection were modest, but ORs for non-work exposures were not! Ill household member (OR 3.8), gatherings >10 (OR 4.6), patronizing restaurant/bar (OR 16.2), public transport (OR 4.4) all registered. Remain vigilant outside the workplace.
3.2
Also noteworthy – workplace exposure to ill HCP colleague also associated with infection (OR 4.9). Another situation in which exposures without PPE expectations were associated with HCP infection. Caution in breakrooms, etc.
Also noteworthy – workplace exposure to ill HCP colleague also associated with infection (OR 4.9). Another situation in which exposures without PPE expectations were associated with HCP infection. Caution in breakrooms, etc.
Major thanks to @Bronchorg and @MaldonadoFabien for spearheading this project, our global champions (all named authors) who recruited HCPs across the globe, and to all those who participated!
Finally, big acknowledgement to @trtalbotmd and Bryan Harris. What began, selfishly, as a narrow look at risk during bronchs evolved into this much more comprehensive project with them. Much respect to #Epitwitter and our infection control colleagues. This research is hard work.
(Lastly, many potential limitations in case-control design such as this. Extensive discussion of these and methods used to limit bias/confounding where possible in the manuscript. Conscious decision was made to not pre-print a study with this design, needed peer review.)

 Read on Twitter
Read on Twitter " title="Pleased to finally present this work! Large (n=1130), global (67 countries) case-control study of exposures associated with HCP illness with COVID-19. Granular look at workplace exposures with respirator vs. medical mask data. https://pubmed.ncbi.nlm.nih.gov/32900402/... main findings: a https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧵" title="Thread" aria-label="Emoji: Thread">" class="img-responsive" style="max-width:100%;"/>
" title="Pleased to finally present this work! Large (n=1130), global (67 countries) case-control study of exposures associated with HCP illness with COVID-19. Granular look at workplace exposures with respirator vs. medical mask data. https://pubmed.ncbi.nlm.nih.gov/32900402/... main findings: a https://abs.twimg.com/emoji/v2/... draggable="false" alt="🧵" title="Thread" aria-label="Emoji: Thread">" class="img-responsive" style="max-width:100%;"/>