Tweetpost: Functioning and its cost
1.This post is about functioning in psychiatry and mental illness but a lot of it will apply to most areas of health and medicine.
1.This post is about functioning in psychiatry and mental illness but a lot of it will apply to most areas of health and medicine.
http://2.Here"> http://2.Here I’m going to talk about functioning for a given individual i.e. how well they are able to function in their own lives NOT about the expectations of the society or rabidly capitalistic system that they happen to be born into (more on that in next tweetpost)
3.Functioning for our present purposes can be thought of as: to what extent is the person able to manage what they need to and want to do in their life? Both ‘need to’ and ‘want to’ are important and we should consider as far as possible all aspects of their life.
4.We usually come at this from the perspective of impairment of functioning. ‘How has this problem been affecting your life? How has it been affecting your work/education/social life/intimate relationships/etc? and by how much?’
5. This is very sensible as it is the change in a person’s functioning is important for the person, for understanding the impact of the condition on their life, for making diagnoses, and sadly for accessing healthcare (especially in underfunded health services).
6.However it is critical to always compare the person’s current functioning to their own baseline (before they became ill or before the current episode of illness/impairment) and not go by one’s own sense of what a reasonable level of functioning is.
http://7.So"> http://7.So if one concludes, ‘Well you’re managing your job and looking after your family so you’re clearly functioning reasonably well’, that is incorrect and deeply unfair to and dismissive of the person before you.
http://8.It"> http://8.It is incredibly hurtful and demoralising to have someone misjudge your capabilities or make assumptions about what they think you are capable of.
9.NOTE: with longer term illnesses, for various reasons people can lose former capabilities and this is incredibly painful. Helping people realise this and work through the grief of these losses is an important part of what we do but that is very different.
http://10.It"> http://10.It is not difficult to get a sense of what someone’s baseline was, and a series of now and then comparisons will get you this information. Example in the next tweet.
11.For concentration,
“Before, how long could you sit and read at a stretch for? How efficiently could you read?”
“How much are you able to manage now? How efficient are you? Do you find yourself having to re-read a lot? Do you struggle to remember what you’ve just read?”
“Before, how long could you sit and read at a stretch for? How efficiently could you read?”
“How much are you able to manage now? How efficient are you? Do you find yourself having to re-read a lot? Do you struggle to remember what you’ve just read?”
12.Getting a sense of both an individual’s baseline and how far they are from that baseline gives you a better measure of the severity of their impairment and also allows you track progression and recovery more accurately.
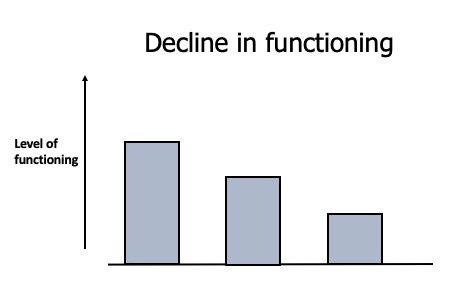
13.This post however is more about one of my major beefs with the concept of functioning, which is that we do not consider the cost of functioning sufficiently. We tend to think of functioning deteriorating like in the figure below.
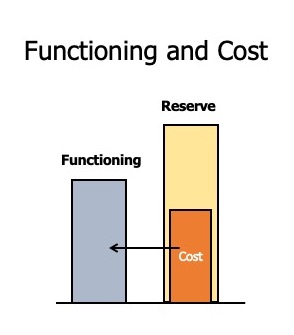
http://14.To"> http://14.To maintain a certain level of functioning, one has to incur a certain cost and one could think about this an energetic cost i.e. how much energy (physical/mental/emotional) does one have to expend every day?
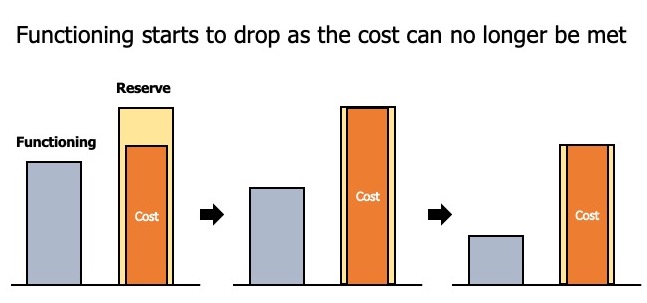
15.This of course depends on both internal and external demands. We’ll come to internal demands a bit later, but external demands are those from one’s environment and life situation e.g. the nature of one’s job, caring responsibilities, etc.
http://16.So"> http://16.So changes in environment and life situation are vital to factor in when one thinks about changes in a person’s functioning and the cost of maintaining that functioning. As always it is vital to get the person& #39;s sense of the impact of the increased demand.
17. One can think about the cost of functioning being met out of a reserve tank that one has and ideally the cost of one’s daily functioning should be met without difficulty leaving one with sufficient reserve for a change in demand i.e. you need to or want to do more.
18.Some of the key components of the cost are:
a.Attention & concentration
b.Mental multitasking
c.Planning
d.Making decisions
e.Emotional processing
http://f.Social"> http://f.Social interaction
g.Cognitive control
h.Processing the information from and physically navigating the world
a.Attention & concentration
b.Mental multitasking
c.Planning
d.Making decisions
e.Emotional processing
http://f.Social"> http://f.Social interaction
g.Cognitive control
h.Processing the information from and physically navigating the world
19.These various costs can go up if the demands increase or if the intrinsic capabilities are affected, say by illness. E.g. fatigue greatly affects the cost of physically navigating the world. Similarly, depression reduces the ability to concentrate.
20. My key point is this, to think about functioning, it is imperative to consider the cost of functioning. Because functioning usually only starts to drop when people are no longer able to meet the cost of functioning and this is already a considerable level of impairment.
22.This is particularly important with high functioning* individuals in unforgiving systems. Doctors and academics are two groups I frequently encounter where this is relevant
*I do not like this commonly used term but I hope you can take the meaning it is intended to convey.
*I do not like this commonly used term but I hope you can take the meaning it is intended to convey.
23. So it is important to consider not just, how has your functioning been affected? But also, how much is it costing you to maintain your current level of functioning?
24. Two important questions follow from this:
http://a.How"> http://a.How does one ask about cost?
b.When does one ask about cost?
http://a.How"> http://a.How does one ask about cost?
b.When does one ask about cost?
25. How does one ask about cost? Here are various pointers to an increased cost of functioning:
a.Feeling more/continuously worn out
b.Reduced efficiency: takes longer to do things, more mistakes
c.Loss of patience
a.Feeling more/continuously worn out
b.Reduced efficiency: takes longer to do things, more mistakes
c.Loss of patience
25. Contd.
d.Loss of confidence: harder to project oneself into the future
e.Reduced capacity for empathy: simply not having the emotional energy to deal with other people’s emotions
f.Irritability: with oneself and others.
d.Loss of confidence: harder to project oneself into the future
e.Reduced capacity for empathy: simply not having the emotional energy to deal with other people’s emotions
f.Irritability: with oneself and others.
26. Contd.
g.Reduced capacity for the unexpected: life becomes more regimented as available energy is carefully rationed out for the expected demands, feeling thrown by unexpected demands of the sort that would have easily been taken in stride before.
g.Reduced capacity for the unexpected: life becomes more regimented as available energy is carefully rationed out for the expected demands, feeling thrown by unexpected demands of the sort that would have easily been taken in stride before.
27. Contd
h. Longer preparation times or having to plan for things that one would have done spontaneously.
i. Longer recovery: wiped out at the end of regular days, spending evenings recovering from the day, weekends recovering from the week, lots of resting but never rested.
h. Longer preparation times or having to plan for things that one would have done spontaneously.
i. Longer recovery: wiped out at the end of regular days, spending evenings recovering from the day, weekends recovering from the week, lots of resting but never rested.
28.
j.Loss of spontaneity and narrowing of life activities: often leisure and restorative activities are given up to have enough time to meet the demands or recover from meeting them.
j.Loss of spontaneity and narrowing of life activities: often leisure and restorative activities are given up to have enough time to meet the demands or recover from meeting them.
29.
k. Anticipatory weariness, dread, anxiety of events: the unexpected, the more demanding expected and then the routine e.g. spending Sunday evenings dreading the next morning.
k. Anticipatory weariness, dread, anxiety of events: the unexpected, the more demanding expected and then the routine e.g. spending Sunday evenings dreading the next morning.
30.
l.Shortening of temporal perspective and decision timescales: thinking about how to get through this week, then how to get through this day. Making short-term (often suboptimal) decisions as it becomes hard to look very far into the future.
l.Shortening of temporal perspective and decision timescales: thinking about how to get through this week, then how to get through this day. Making short-term (often suboptimal) decisions as it becomes hard to look very far into the future.
31. When does one ask about cost?
This is much shorter: at all stages.
Ask about the cost of functioning early on when people are becoming stressed/burnt out/unwell.
There is a particular issue here when it comes to diagnosis and service thresholds.
This is much shorter: at all stages.
Ask about the cost of functioning early on when people are becoming stressed/burnt out/unwell.
There is a particular issue here when it comes to diagnosis and service thresholds.
32. Diagnostic systems and service thresholds set great weight by functional impairment. My view is that cost has to be considered as well and waiting for people to become sufficiently impaired is waiting for things to get worse before intervening. However this is complex.
33. Ask when people are recovering from the episode of illness. This is particularly important when looking for residual symptoms especially when more prominent symptoms like depressed mood may have abated. Ask during the ongoing illness (especially so for long-term illness).
34. Think about the cost of functioning when thinking about recovery. Symptomatic improvement is very important but you do really want to help people get back to both their previous level of and cost of functioning.
35. I did say I was going to come back to internal demands and this is specifically about the impact of different mental illness, particularly ongoing and long-term conditions where people have to deal with the demands of managing the illness alongside everything else.
36. So going back to those components of cost, here are some examples:
a.Attention & concentration: ruminations (depressive, anxious, obsessive compulsive) take up a huge amount of attention and cognitive space as people are often dealing with them alongside other demands.
a.Attention & concentration: ruminations (depressive, anxious, obsessive compulsive) take up a huge amount of attention and cognitive space as people are often dealing with them alongside other demands.
37.
b.Mental multitasking: allocating mental space to ruminations and hallucinatory experiences, allocating attention in ADHD
c.Planning: both internal resource allocation (major problem in ADHD) and action (anxiety, psychosis)
b.Mental multitasking: allocating mental space to ruminations and hallucinatory experiences, allocating attention in ADHD
c.Planning: both internal resource allocation (major problem in ADHD) and action (anxiety, psychosis)
38.
d. Emotional processing and social interaction: pretty much every mental illness but particular mention here for autistic spectrum disorders (this is a continuous demand) and the problematic construct of borderline personality where emotions are extremely intense and painful.
d. Emotional processing and social interaction: pretty much every mental illness but particular mention here for autistic spectrum disorders (this is a continuous demand) and the problematic construct of borderline personality where emotions are extremely intense and painful.
39.
e. Making decisions: massively increased demand in depression and OCD were decision making becomes extremely fraught and difficult..
f. Cognitive control: deciding what to do and not to do, major issue in ADHD and OCD.
e. Making decisions: massively increased demand in depression and OCD were decision making becomes extremely fraught and difficult..
f. Cognitive control: deciding what to do and not to do, major issue in ADHD and OCD.
40.
g. Processing the information from and physically navigating the world: can be extremely demanding in psychosis and a continuous demand in ASD.
g. Processing the information from and physically navigating the world: can be extremely demanding in psychosis and a continuous demand in ASD.
41. The above list is not meant to be exhaustive but only to illustrate that living with mental illnesses incurs a significant cost and often people have to make major adjustments to their lives to accommodate this e.g. giving up on particular jobs/activities.
42. It’s also important to remember that costs and demands accrue over time and one is often having to deal with the consequences/remainders of the previous day(s).
43. A particular point about considering cost in people with long-term illnesses across medical specialities. People can present as reasonably well in short cross-sections and if one does not ask about cost, you can assume that things are much better than they are.
44. When people come to see us in clinics, they make a huge effort to present themselves as well as possible. This is a strong cultural expectation i.e. ‘I need to look decent if I’m going to see the doctor’ and like all such expectations, it is unfairly harder on women.
45. People have to be very impaired before they look obviously impaired. A frequent experience that my patients with chronic physical illness have had when they go to the general hospital is being told that they look very well so they must be doing ok.
46. As one lady very memorably told me, ‘They don’t realise that it took me 6 hours to get ready for the appointment and it’ll take me 2 days in bed to recover from it’.
47. I usually ask something along these lines, ‘Seeing you in this brief snapshot today, you come across as pretty well but I wonder how much effort it has taken for you to get yourself here today.’
48. As I mentioned earlier, as illnesses go on, impairments accrue and people (often repeatedly) have to deal with the grief of losing important aspects of their selves, their abilities and their lives. Thinking about functioning and cost has to track all this.
49. Nearly at the end. Complete disclosure: this is all from my experience in clinic and my own experiences with depression. I am sure people have written about this with much more thought and clarity. If you have any references to suggest, please do, they would be very welcome.
50. Christine Miserandino& #39;s 2003 essay on Spoon Theory is very helpful for thinking about the impact of chronic illness on life and functioning. I think it is important to take a much wider view on the cost of functioning at all stages of illnesses.
51. So this tweetpost has been focussed on what’s happening in the person. In the next tweetpost we’ll look at the impact of environments (and the role of societal expectations) in ‘The Multiplying Wounds and Scars of Trauma’.
END.
END.

 Read on Twitter
Read on Twitter