1/  https://abs.twimg.com/emoji/v2/... draggable="false" alt="💭" title="Gedankenblase" aria-label="Emoji: Gedankenblase">Thoughts of a trainee
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💭" title="Gedankenblase" aria-label="Emoji: Gedankenblase">Thoughts of a trainee https://abs.twimg.com/emoji/v2/... draggable="false" alt="💭" title="Gedankenblase" aria-label="Emoji: Gedankenblase">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="💭" title="Gedankenblase" aria-label="Emoji: Gedankenblase">
“Should I call my [resident/fellow/attending]?”
“I don’t want to be a bother.”
“I don’t want them to think I’m dumb.”
Sound familiar?
I know these thoughts plagued me.
How can we prevent this?
This week’s #ClinicalTeaching topic: Be Available
“Should I call my [resident/fellow/attending]?”
“I don’t want to be a bother.”
“I don’t want them to think I’m dumb.”
Sound familiar?
I know these thoughts plagued me.
How can we prevent this?
This week’s #ClinicalTeaching topic: Be Available
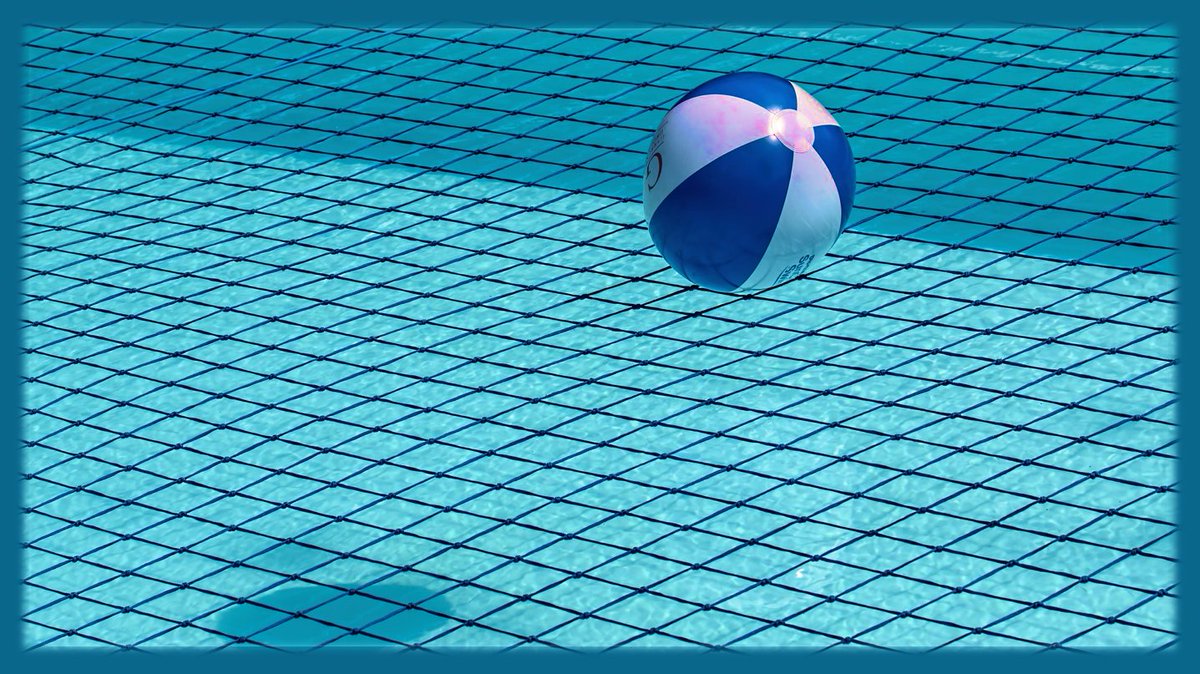
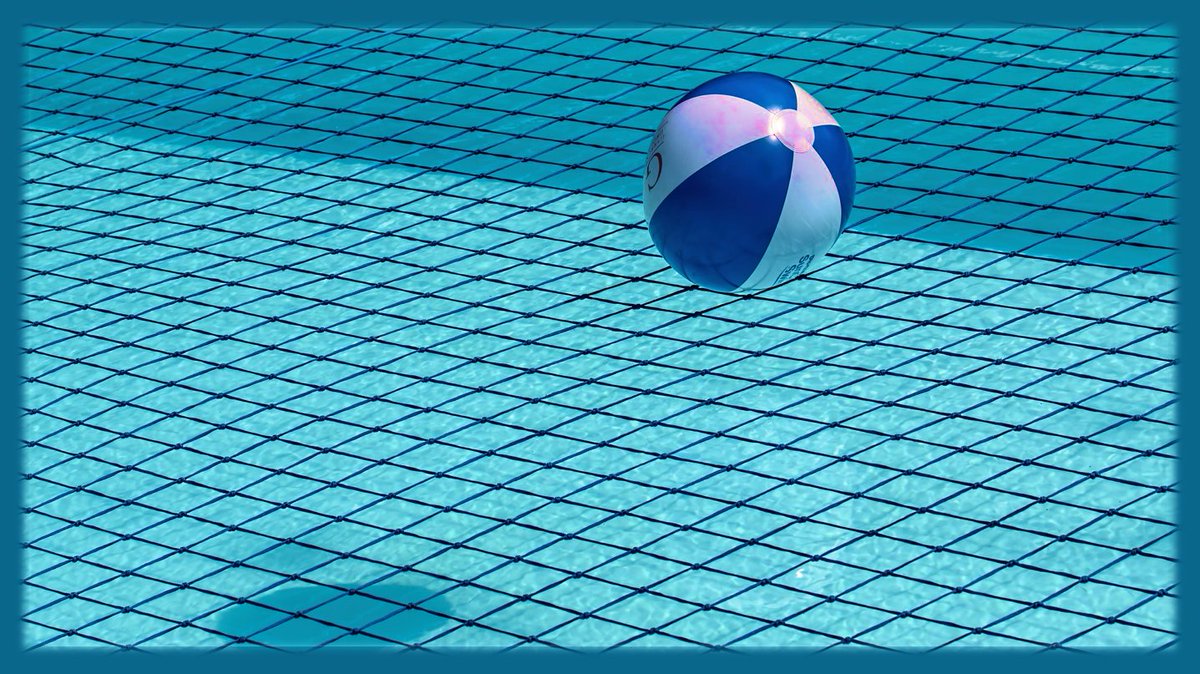
2/ To me, “Being Available” means ensuring that my team feels that I am their safety net
Nothing is beneath me.
I’m here to help.
WE, as a team, are responsible for our patients.
A failure of one, is a failure of all.
Yet, an accomplishment of one should be celebrated by all.
Nothing is beneath me.
I’m here to help.
WE, as a team, are responsible for our patients.
A failure of one, is a failure of all.
Yet, an accomplishment of one should be celebrated by all.
3/
In my mind, the concept of “Being Available” has two components:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="1⃣" title="Tastenkappe Ziffer 1" aria-label="Emoji: Tastenkappe Ziffer 1">Approachability (i.e. are people comfortable asking for help?)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="1⃣" title="Tastenkappe Ziffer 1" aria-label="Emoji: Tastenkappe Ziffer 1">Approachability (i.e. are people comfortable asking for help?)
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="2⃣" title="Tastenkappe Ziffer 2" aria-label="Emoji: Tastenkappe Ziffer 2">Proximity (i.e. are you physically & mentally “there” for your team?)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="2⃣" title="Tastenkappe Ziffer 2" aria-label="Emoji: Tastenkappe Ziffer 2">Proximity (i.e. are you physically & mentally “there” for your team?)
In my mind, the concept of “Being Available” has two components:
4/ Approachability has two inter-related aspects:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts"> Creating a safe learning climate
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts"> Creating a safe learning climate
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts"> Setting clear expectations
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts"> Setting clear expectations
5/ A safe learning climate means that team members are comfortable being vulnerable.
Imposter syndrome is prevalent in medicine:
https://link.springer.com/article/10.1007/s11606-019-05364-1
We">https://link.springer.com/article/1... should encourage team members to ask questions.
...And answer those questions.
Saying "look it up" is not always helpful
Imposter syndrome is prevalent in medicine:
https://link.springer.com/article/10.1007/s11606-019-05364-1
We">https://link.springer.com/article/1... should encourage team members to ask questions.
...And answer those questions.
Saying "look it up" is not always helpful
6/ Setting clear expectations regarding availability is helpful
As a trainee, I found myself worrying about “bothering” people when I called.
As attendings/fellows/residents, we should set the expectation that needing help is normal & reiterate that people should call if needed
As a trainee, I found myself worrying about “bothering” people when I called.
As attendings/fellows/residents, we should set the expectation that needing help is normal & reiterate that people should call if needed
7/ Go beyond saying “call if needed” & be explicit.
I tell trainees they can contact me anytime when I’m awake (5:00 am – 9:00 pm), & ANYTIME for the following:
If a patient decompensates
If a patient tries to leave AMA
If a time-sensitive decision needs to be made
I tell trainees they can contact me anytime when I’m awake (5:00 am – 9:00 pm), & ANYTIME for the following:
If a patient decompensates
If a patient tries to leave AMA
If a time-sensitive decision needs to be made
8/ Now let’s talk about proximity.
When I say proximity, I mean both:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts"> Physical proximity (i.e. in the same room, hospital, etc)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts"> Physical proximity (i.e. in the same room, hospital, etc)
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts"> Mental proximity (i.e. not staring at your phone, thinking of something else, etc)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts"> Mental proximity (i.e. not staring at your phone, thinking of something else, etc)
When I say proximity, I mean both:
9/ First, especially as an attending, try to be “mentally present” for your team by blocking off your schedule.
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Mittelgroßer Stern" aria-label="Emoji: Mittelgroßer Stern"> Avoid scheduling research meetings, other educational obligations, etc
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Mittelgroßer Stern" aria-label="Emoji: Mittelgroßer Stern"> Avoid scheduling research meetings, other educational obligations, etc
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Mittelgroßer Stern" aria-label="Emoji: Mittelgroßer Stern"> Cancel as many non-essential recurring meetings as possible
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Mittelgroßer Stern" aria-label="Emoji: Mittelgroßer Stern"> Cancel as many non-essential recurring meetings as possible
10/
Then, during rounds, pay attention.
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Use active learning techniques
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Use active learning techniques
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Use positive, open body language
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Use positive, open body language
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Avoid glancing at your phone
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Avoid glancing at your phone
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Avoid looking at the patient& #39;s chart
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Avoid looking at the patient& #39;s chart
And, if presentations are too long, then provide feedback instead of tuning out!
Then, during rounds, pay attention.
And, if presentations are too long, then provide feedback instead of tuning out!
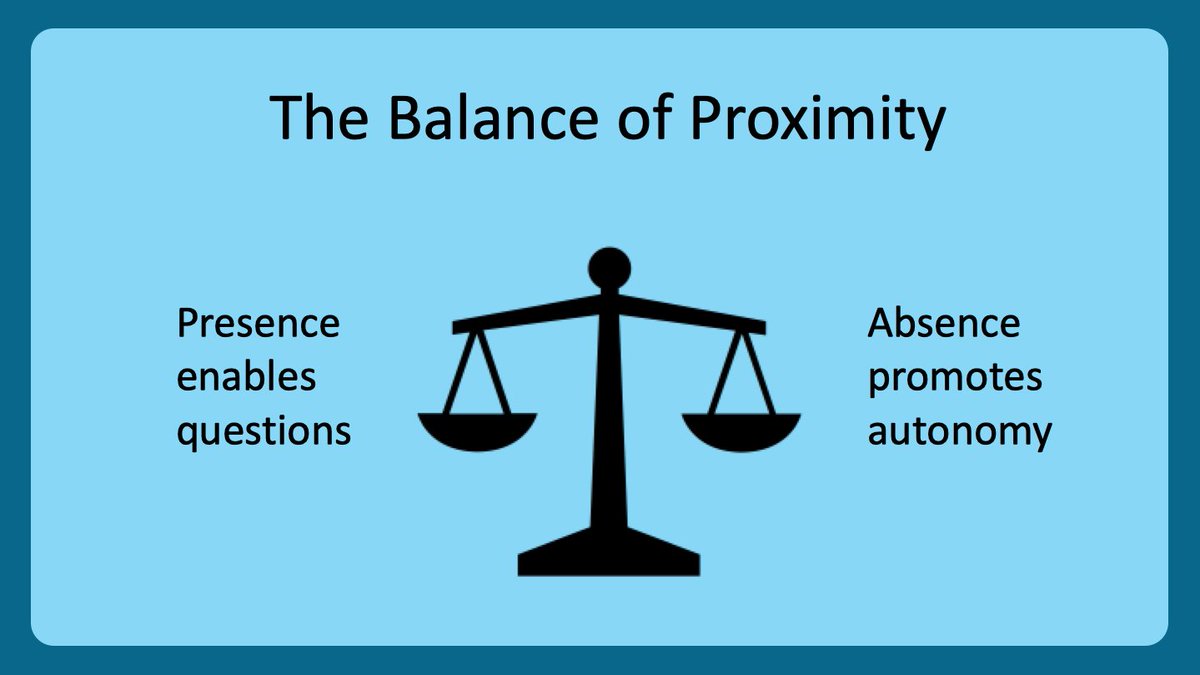
11/ Physical proximity lowers the barrier to ask questions, which has pros & cons.
Being present makes it easier for others to ask you questions.
This can be good.
But significant learning also occurs when learners are on their own (eg. nightfloat)
Appropriate balance is key
Being present makes it easier for others to ask you questions.
This can be good.
But significant learning also occurs when learners are on their own (eg. nightfloat)
Appropriate balance is key
12/ So what’s the ideal physical proximity?
It probably depends who you are on the team:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="*⃣" title="Tastenkappe Sternchen" aria-label="Emoji: Tastenkappe Sternchen"> Attending: stay during rounds, then let team do work
https://abs.twimg.com/emoji/v2/... draggable="false" alt="*⃣" title="Tastenkappe Sternchen" aria-label="Emoji: Tastenkappe Sternchen"> Attending: stay during rounds, then let team do work
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="*⃣" title="Tastenkappe Sternchen" aria-label="Emoji: Tastenkappe Sternchen"> Fellow: stay until residents done with notes
https://abs.twimg.com/emoji/v2/... draggable="false" alt="*⃣" title="Tastenkappe Sternchen" aria-label="Emoji: Tastenkappe Sternchen"> Fellow: stay until residents done with notes
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="*⃣" title="Tastenkappe Sternchen" aria-label="Emoji: Tastenkappe Sternchen"> Residents: stay until the team’s work is done
https://abs.twimg.com/emoji/v2/... draggable="false" alt="*⃣" title="Tastenkappe Sternchen" aria-label="Emoji: Tastenkappe Sternchen"> Residents: stay until the team’s work is done
It probably depends who you are on the team:
13/ Staying until the work is done helps:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Mittelgroßer Stern" aria-label="Emoji: Mittelgroßer Stern">Fellows
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Mittelgroßer Stern" aria-label="Emoji: Mittelgroßer Stern">Fellows https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Mittelgroßer Stern" aria-label="Emoji: Mittelgroßer Stern">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Mittelgroßer Stern" aria-label="Emoji: Mittelgroßer Stern">
Residents will write better consult notes b/c they are more likely to ask detail-oriented questions
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Mittelgroßer Stern" aria-label="Emoji: Mittelgroßer Stern">Residents
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Mittelgroßer Stern" aria-label="Emoji: Mittelgroßer Stern">Residents https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Mittelgroßer Stern" aria-label="Emoji: Mittelgroßer Stern">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Mittelgroßer Stern" aria-label="Emoji: Mittelgroßer Stern">
Interns will appreciate you helping them with work; plus, you will know more about their workflow & efficiency
Residents will write better consult notes b/c they are more likely to ask detail-oriented questions
Interns will appreciate you helping them with work; plus, you will know more about their workflow & efficiency
14/ And as an intern, being available to medical students is important & rewarding.
You have lots to teach.
And you can help the students shine on rounds.
Just set clear expectations with students to maximize learning & patient care
(more on this next week from @GStetsonMD!)
You have lots to teach.
And you can help the students shine on rounds.
Just set clear expectations with students to maximize learning & patient care
(more on this next week from @GStetsonMD!)
15/ So, in summary, be your team’s safety net using these concepts:
Approachability:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Create a safe learning climate
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Create a safe learning climate
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Set clear expectations regarding availability
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Set clear expectations regarding availability
Proximity:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Be physically close (while allowing autonomy)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Be physically close (while allowing autonomy)
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Be mentally present to the team
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Be mentally present to the team
Approachability:
Proximity:
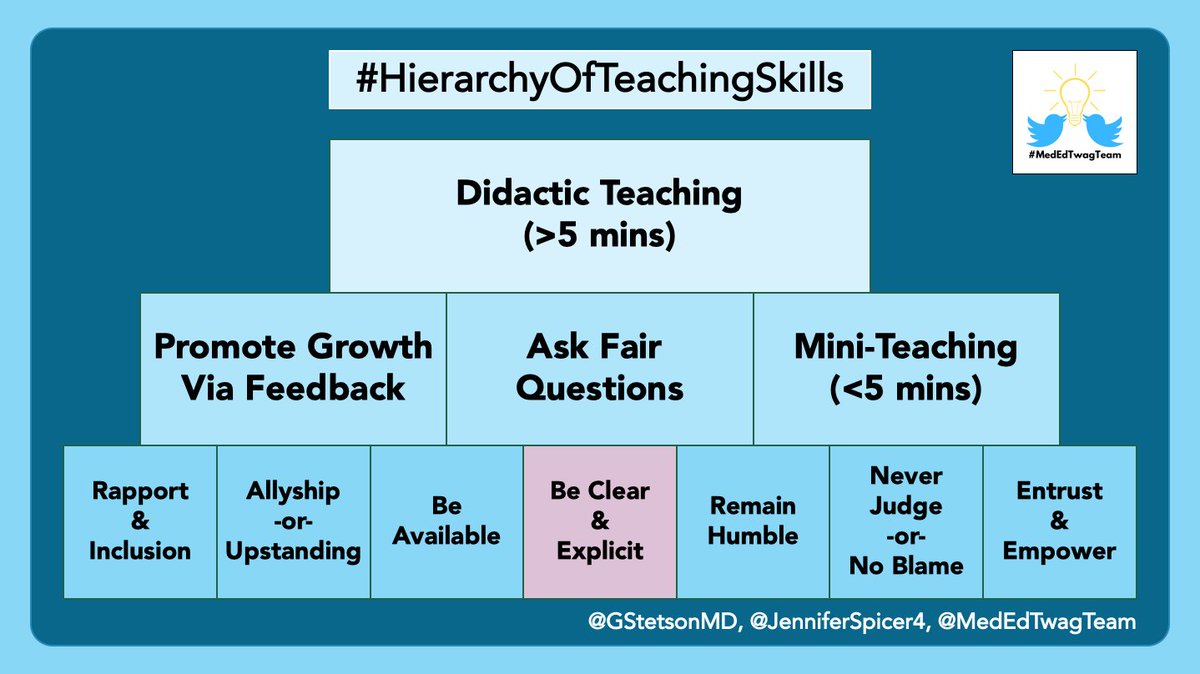
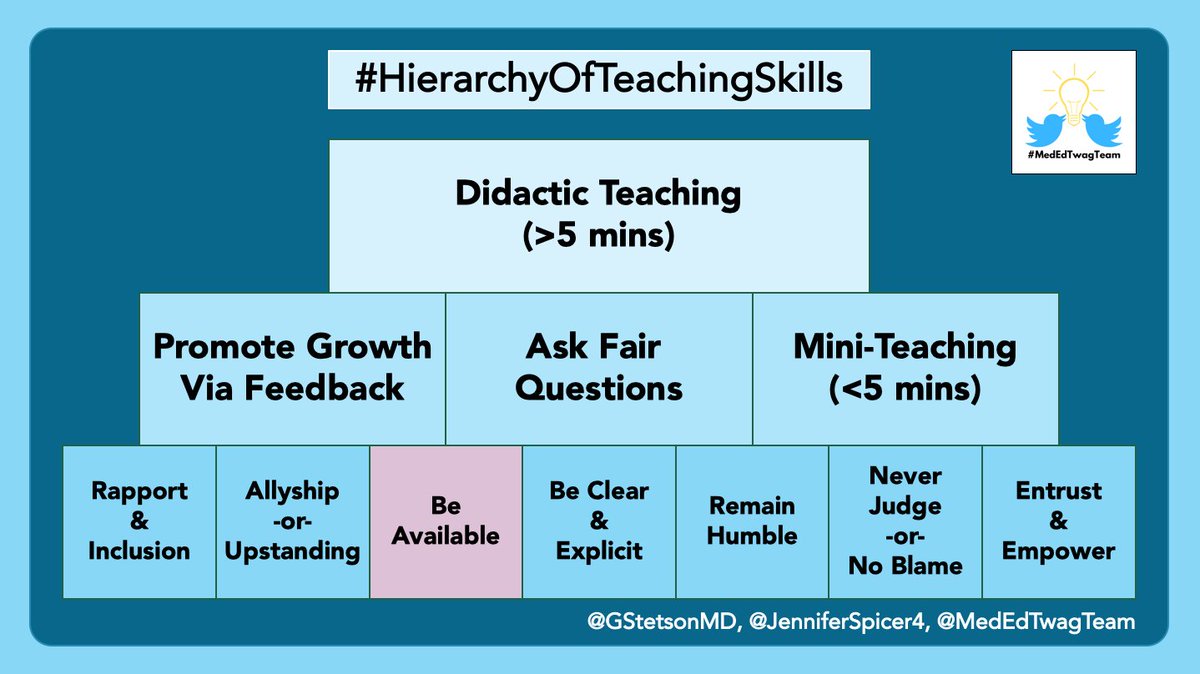
16/ And keep an eye out for @GStetsonMD’s thread next Tuesday on ”Be Clear & Explicit”
And check out the @MedEdTwagTeam if you want to see all of our threads in one place!
Thanks for joining, and we will see you next week!
And check out the @MedEdTwagTeam if you want to see all of our threads in one place!
Thanks for joining, and we will see you next week!

 Read on Twitter
Read on Twitter Thoughts of a traineehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="💭" title="Gedankenblase" aria-label="Emoji: Gedankenblase">“Should I call my [resident/fellow/attending]?”“I don’t want to be a bother.”“I don’t want them to think I’m dumb.”Sound familiar? I know these thoughts plagued me.How can we prevent this?This week’s #ClinicalTeaching topic: Be Available" title="1/ https://abs.twimg.com/emoji/v2/... draggable="false" alt="💭" title="Gedankenblase" aria-label="Emoji: Gedankenblase">Thoughts of a traineehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="💭" title="Gedankenblase" aria-label="Emoji: Gedankenblase">“Should I call my [resident/fellow/attending]?”“I don’t want to be a bother.”“I don’t want them to think I’m dumb.”Sound familiar? I know these thoughts plagued me.How can we prevent this?This week’s #ClinicalTeaching topic: Be Available" class="img-responsive" style="max-width:100%;"/>
Thoughts of a traineehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="💭" title="Gedankenblase" aria-label="Emoji: Gedankenblase">“Should I call my [resident/fellow/attending]?”“I don’t want to be a bother.”“I don’t want them to think I’m dumb.”Sound familiar? I know these thoughts plagued me.How can we prevent this?This week’s #ClinicalTeaching topic: Be Available" title="1/ https://abs.twimg.com/emoji/v2/... draggable="false" alt="💭" title="Gedankenblase" aria-label="Emoji: Gedankenblase">Thoughts of a traineehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="💭" title="Gedankenblase" aria-label="Emoji: Gedankenblase">“Should I call my [resident/fellow/attending]?”“I don’t want to be a bother.”“I don’t want them to think I’m dumb.”Sound familiar? I know these thoughts plagued me.How can we prevent this?This week’s #ClinicalTeaching topic: Be Available" class="img-responsive" style="max-width:100%;"/>
 Approachability (i.e. are people comfortable asking for help?)https://abs.twimg.com/emoji/v2/... draggable="false" alt="2⃣" title="Tastenkappe Ziffer 2" aria-label="Emoji: Tastenkappe Ziffer 2">Proximity (i.e. are you physically & mentally “there” for your team?)" title="3/ In my mind, the concept of “Being Available” has two components:https://abs.twimg.com/emoji/v2/... draggable="false" alt="1⃣" title="Tastenkappe Ziffer 1" aria-label="Emoji: Tastenkappe Ziffer 1">Approachability (i.e. are people comfortable asking for help?)https://abs.twimg.com/emoji/v2/... draggable="false" alt="2⃣" title="Tastenkappe Ziffer 2" aria-label="Emoji: Tastenkappe Ziffer 2">Proximity (i.e. are you physically & mentally “there” for your team?)" class="img-responsive" style="max-width:100%;"/>
Approachability (i.e. are people comfortable asking for help?)https://abs.twimg.com/emoji/v2/... draggable="false" alt="2⃣" title="Tastenkappe Ziffer 2" aria-label="Emoji: Tastenkappe Ziffer 2">Proximity (i.e. are you physically & mentally “there” for your team?)" title="3/ In my mind, the concept of “Being Available” has two components:https://abs.twimg.com/emoji/v2/... draggable="false" alt="1⃣" title="Tastenkappe Ziffer 1" aria-label="Emoji: Tastenkappe Ziffer 1">Approachability (i.e. are people comfortable asking for help?)https://abs.twimg.com/emoji/v2/... draggable="false" alt="2⃣" title="Tastenkappe Ziffer 2" aria-label="Emoji: Tastenkappe Ziffer 2">Proximity (i.e. are you physically & mentally “there” for your team?)" class="img-responsive" style="max-width:100%;"/>
 Creating a safe learning climatehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts"> Setting clear expectations" title="4/ Approachability has two inter-related aspects:https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts"> Creating a safe learning climatehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts"> Setting clear expectations" class="img-responsive" style="max-width:100%;"/>
Creating a safe learning climatehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts"> Setting clear expectations" title="4/ Approachability has two inter-related aspects:https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts"> Creating a safe learning climatehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Rückhand Zeigefinger nach rechts" aria-label="Emoji: Rückhand Zeigefinger nach rechts"> Setting clear expectations" class="img-responsive" style="max-width:100%;"/>
 Avoid scheduling research meetings, other educational obligations, etchttps://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Mittelgroßer Stern" aria-label="Emoji: Mittelgroßer Stern"> Cancel as many non-essential recurring meetings as possible" title="9/ First, especially as an attending, try to be “mentally present” for your team by blocking off your schedule.https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Mittelgroßer Stern" aria-label="Emoji: Mittelgroßer Stern"> Avoid scheduling research meetings, other educational obligations, etchttps://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Mittelgroßer Stern" aria-label="Emoji: Mittelgroßer Stern"> Cancel as many non-essential recurring meetings as possible" class="img-responsive" style="max-width:100%;"/>
Avoid scheduling research meetings, other educational obligations, etchttps://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Mittelgroßer Stern" aria-label="Emoji: Mittelgroßer Stern"> Cancel as many non-essential recurring meetings as possible" title="9/ First, especially as an attending, try to be “mentally present” for your team by blocking off your schedule.https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Mittelgroßer Stern" aria-label="Emoji: Mittelgroßer Stern"> Avoid scheduling research meetings, other educational obligations, etchttps://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Mittelgroßer Stern" aria-label="Emoji: Mittelgroßer Stern"> Cancel as many non-essential recurring meetings as possible" class="img-responsive" style="max-width:100%;"/>
 Attending: stay during rounds, then let team do workhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="*⃣" title="Tastenkappe Sternchen" aria-label="Emoji: Tastenkappe Sternchen"> Fellow: stay until residents done with noteshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="*⃣" title="Tastenkappe Sternchen" aria-label="Emoji: Tastenkappe Sternchen"> Residents: stay until the team’s work is done" title="12/ So what’s the ideal physical proximity?It probably depends who you are on the team:https://abs.twimg.com/emoji/v2/... draggable="false" alt="*⃣" title="Tastenkappe Sternchen" aria-label="Emoji: Tastenkappe Sternchen"> Attending: stay during rounds, then let team do workhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="*⃣" title="Tastenkappe Sternchen" aria-label="Emoji: Tastenkappe Sternchen"> Fellow: stay until residents done with noteshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="*⃣" title="Tastenkappe Sternchen" aria-label="Emoji: Tastenkappe Sternchen"> Residents: stay until the team’s work is done" class="img-responsive" style="max-width:100%;"/>
Attending: stay during rounds, then let team do workhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="*⃣" title="Tastenkappe Sternchen" aria-label="Emoji: Tastenkappe Sternchen"> Fellow: stay until residents done with noteshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="*⃣" title="Tastenkappe Sternchen" aria-label="Emoji: Tastenkappe Sternchen"> Residents: stay until the team’s work is done" title="12/ So what’s the ideal physical proximity?It probably depends who you are on the team:https://abs.twimg.com/emoji/v2/... draggable="false" alt="*⃣" title="Tastenkappe Sternchen" aria-label="Emoji: Tastenkappe Sternchen"> Attending: stay during rounds, then let team do workhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="*⃣" title="Tastenkappe Sternchen" aria-label="Emoji: Tastenkappe Sternchen"> Fellow: stay until residents done with noteshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="*⃣" title="Tastenkappe Sternchen" aria-label="Emoji: Tastenkappe Sternchen"> Residents: stay until the team’s work is done" class="img-responsive" style="max-width:100%;"/>
 Create a safe learning climatehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Set clear expectations regarding availabilityProximity:https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Be physically close (while allowing autonomy)https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Be mentally present to the team" title="15/ So, in summary, be your team’s safety net using these concepts:Approachability:https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Create a safe learning climatehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Set clear expectations regarding availabilityProximity:https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Be physically close (while allowing autonomy)https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Be mentally present to the team" class="img-responsive" style="max-width:100%;"/>
Create a safe learning climatehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Set clear expectations regarding availabilityProximity:https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Be physically close (while allowing autonomy)https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Be mentally present to the team" title="15/ So, in summary, be your team’s safety net using these concepts:Approachability:https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Create a safe learning climatehttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Set clear expectations regarding availabilityProximity:https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Be physically close (while allowing autonomy)https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="Fettes weißes Häkchen" aria-label="Emoji: Fettes weißes Häkchen"> Be mentally present to the team" class="img-responsive" style="max-width:100%;"/>