On consults this weekend, I faced a question of whether a patient& #39;s thrombocytosis was secondary to iron deficiency or due to a clonal process, and it got me thinking...
Why does iron deficiency (ID) cause thrombocytosis?
Why does iron deficiency (ID) cause thrombocytosis?
2/
The data clearly support an association between iron deficiency and https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> in plt ct
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> in plt ct
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉🏼" title="Rückhand Zeigefinger nach rechts (mittelheller Hautton)" aria-label="Emoji: Rückhand Zeigefinger nach rechts (mittelheller Hautton)"> Review of all 5k patients, 1 clinic, 1 yr:
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉🏼" title="Rückhand Zeigefinger nach rechts (mittelheller Hautton)" aria-label="Emoji: Rückhand Zeigefinger nach rechts (mittelheller Hautton)"> Review of all 5k patients, 1 clinic, 1 yr:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔸" title="Kleine orangene Raute" aria-label="Emoji: Kleine orangene Raute">10% of pts with IDA had
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔸" title="Kleine orangene Raute" aria-label="Emoji: Kleine orangene Raute">10% of pts with IDA had  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> plt
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> plt
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔸" title="Kleine orangene Raute" aria-label="Emoji: Kleine orangene Raute">Only 1% of control pts (nl iron) had
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔸" title="Kleine orangene Raute" aria-label="Emoji: Kleine orangene Raute">Only 1% of control pts (nl iron) had  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> plt
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> plt
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔸" title="Kleine orangene Raute" aria-label="Emoji: Kleine orangene Raute">Lower ferritin corr. with higher plt count
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔸" title="Kleine orangene Raute" aria-label="Emoji: Kleine orangene Raute">Lower ferritin corr. with higher plt count
https://doi.org/10.1182/blood-2018-99-119352">https://doi.org/10.1182/b...
The data clearly support an association between iron deficiency and
https://doi.org/10.1182/blood-2018-99-119352">https://doi.org/10.1182/b...
3/
In patients with ID-assoc. thrombocytosis, usually mild-moderate https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> plt
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> plt
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉🏼" title="Rückhand Zeigefinger nach rechts (mittelheller Hautton)" aria-label="Emoji: Rückhand Zeigefinger nach rechts (mittelheller Hautton)"> Series of 100 consec. patients with IDA
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉🏼" title="Rückhand Zeigefinger nach rechts (mittelheller Hautton)" aria-label="Emoji: Rückhand Zeigefinger nach rechts (mittelheller Hautton)"> Series of 100 consec. patients with IDA
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔹" title="Kleine blaue Raute" aria-label="Emoji: Kleine blaue Raute">Average plt 499k
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔹" title="Kleine blaue Raute" aria-label="Emoji: Kleine blaue Raute">Average plt 499k
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔹" title="Kleine blaue Raute" aria-label="Emoji: Kleine blaue Raute">Only 7% with plt > 1 million
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔹" title="Kleine blaue Raute" aria-label="Emoji: Kleine blaue Raute">Only 7% with plt > 1 million
https://www.jstage.jst.go.jp/article/internalmedicine/44/10/44_10_1025/_pdf">https://www.jstage.jst.go.jp/article/i...
In patients with ID-assoc. thrombocytosis, usually mild-moderate
https://www.jstage.jst.go.jp/article/internalmedicine/44/10/44_10_1025/_pdf">https://www.jstage.jst.go.jp/article/i...
4/
So I& #39;ve shown that iron deficiency is associated with thrombocytosis, but we haven& #39;t discussed causality, and haven& #39;t gotten any closer to answering the question: WHY?
So I& #39;ve shown that iron deficiency is associated with thrombocytosis, but we haven& #39;t discussed causality, and haven& #39;t gotten any closer to answering the question: WHY?
5/
To answer that, let& #39;s start with a quick refresher on platelet maturation.
We start with the multipotent hematopoietic stem cell: this little guy can ultimately become any sort of blood cell the body needs: platelet, RBC, and the full spectrum of WBCs.
To answer that, let& #39;s start with a quick refresher on platelet maturation.
We start with the multipotent hematopoietic stem cell: this little guy can ultimately become any sort of blood cell the body needs: platelet, RBC, and the full spectrum of WBCs.
6/
The HSC progresses to a megakaryocyte (MK)/erythrocyte precursor
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="↪️" title="Nach rechts zeigender Pfeil mit Haken" aria-label="Emoji: Nach rechts zeigender Pfeil mit Haken"> then to a MK
https://abs.twimg.com/emoji/v2/... draggable="false" alt="↪️" title="Nach rechts zeigender Pfeil mit Haken" aria-label="Emoji: Nach rechts zeigender Pfeil mit Haken"> then to a MK
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="↪️" title="Nach rechts zeigender Pfeil mit Haken" aria-label="Emoji: Nach rechts zeigender Pfeil mit Haken"> which flicks off pieces of its cytoplasm to create platelets
https://abs.twimg.com/emoji/v2/... draggable="false" alt="↪️" title="Nach rechts zeigender Pfeil mit Haken" aria-label="Emoji: Nach rechts zeigender Pfeil mit Haken"> which flicks off pieces of its cytoplasm to create platelets
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="↪️" title="Nach rechts zeigender Pfeil mit Haken" aria-label="Emoji: Nach rechts zeigender Pfeil mit Haken"> that then leave the BM and go out into the bloodstream.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="↪️" title="Nach rechts zeigender Pfeil mit Haken" aria-label="Emoji: Nach rechts zeigender Pfeil mit Haken"> that then leave the BM and go out into the bloodstream.
TPO (Thrombopoietin) drives this maturation process.
The HSC progresses to a megakaryocyte (MK)/erythrocyte precursor
TPO (Thrombopoietin) drives this maturation process.
7/
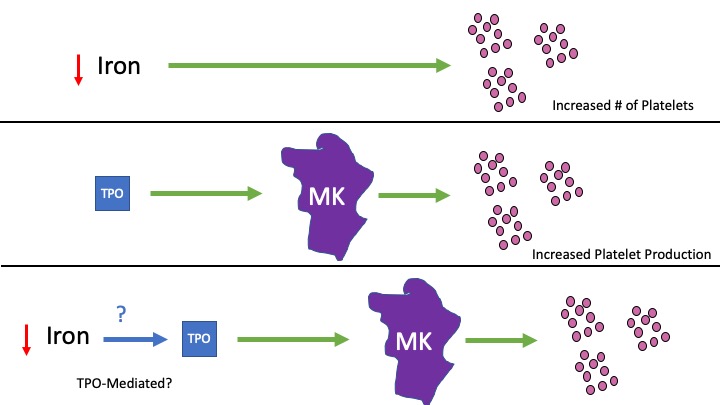
Therefore, since TPO leads to more platelets, and iron deficiency leads to more platelets...
Is this the mechanism?
I.e. does decreased iron lead to more TPO and that& #39;s why platelets go up?
Therefore, since TPO leads to more platelets, and iron deficiency leads to more platelets...
Is this the mechanism?
I.e. does decreased iron lead to more TPO and that& #39;s why platelets go up?
8/
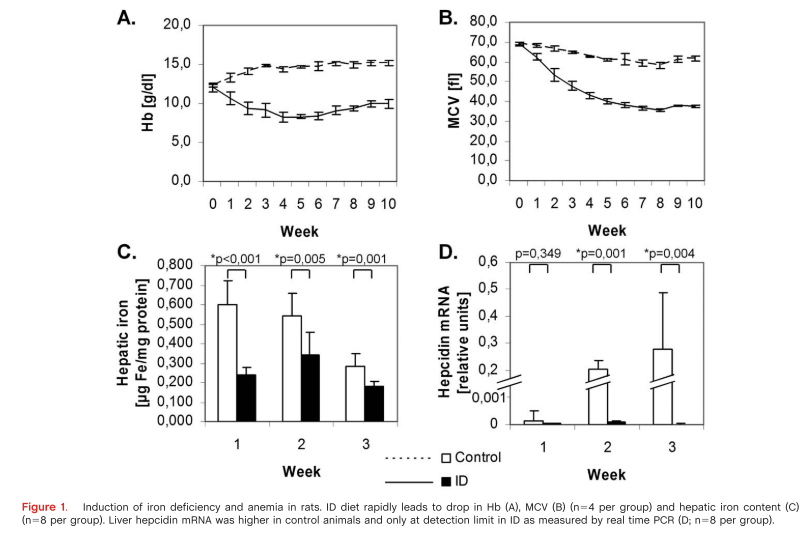
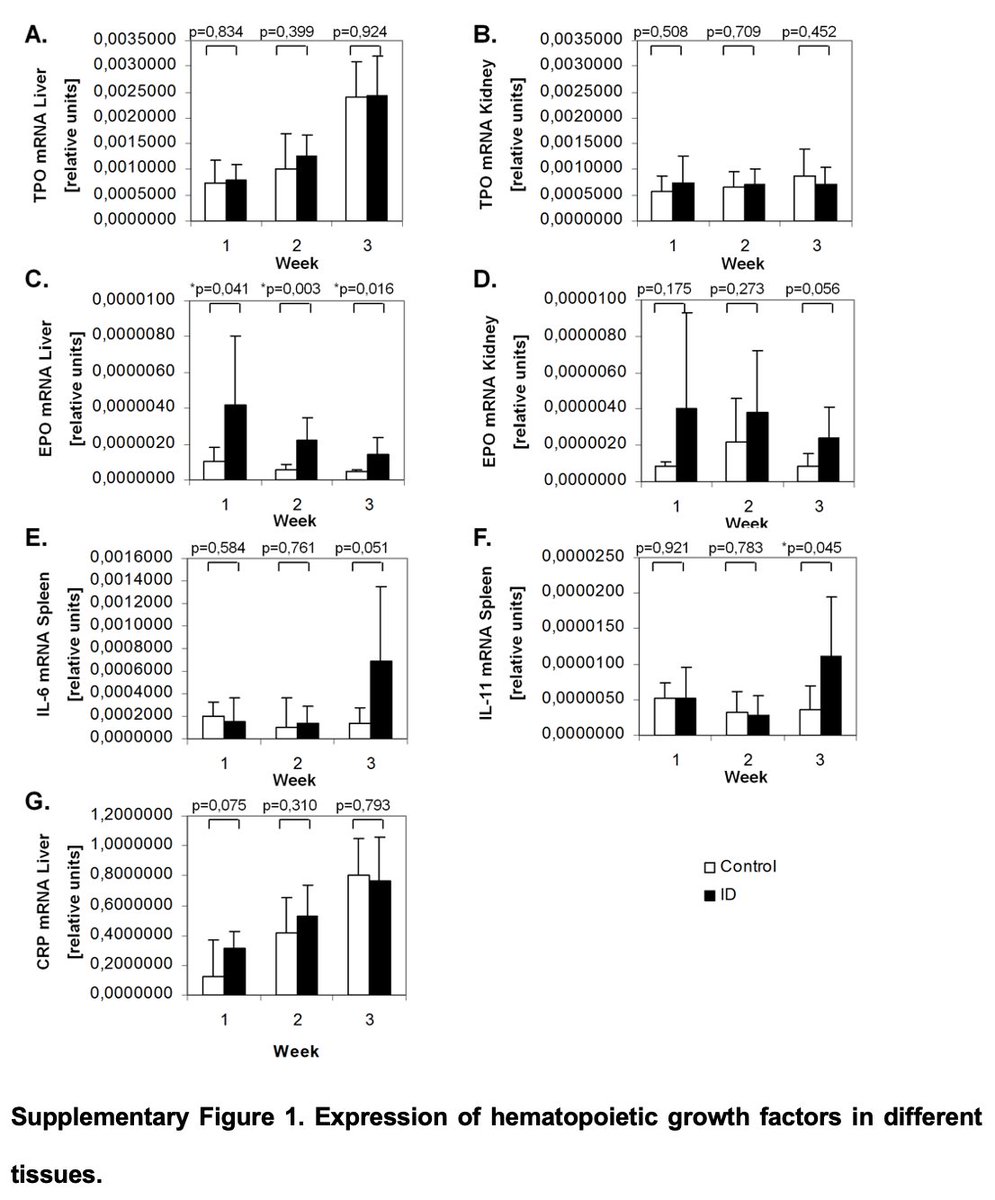
In a rat study, Evstatiev et al induced iron deficiency and looked at various cytokine levels over time.
They induced iron deficiency (measured by hepatic iron) and subsequently microcytic anemia + thrombocytosis (compared to control rats) within a matter of weeks.
In a rat study, Evstatiev et al induced iron deficiency and looked at various cytokine levels over time.
They induced iron deficiency (measured by hepatic iron) and subsequently microcytic anemia + thrombocytosis (compared to control rats) within a matter of weeks.
9/
HOWEVER, while TPO https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> with time in both groups, TPO levels were similar between groups.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> with time in both groups, TPO levels were similar between groups.
IL-6 and IL-11 (also suggested as involved in IDA thrombocytosis) did rise in week 3 spec. in the ID group, but that rise came after the https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> in platelets.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> in platelets.
HOWEVER, while TPO
IL-6 and IL-11 (also suggested as involved in IDA thrombocytosis) did rise in week 3 spec. in the ID group, but that rise came after the
10/
They DID find increased ploidy (DNA replication) of Megakaryocytes in the ID group https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> larger MKs
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> larger MKs  https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> platelet-producing ability.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> platelet-producing ability.
This suggests that iron deficiency causes https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> MK size (via increased DNA replication), and thereby
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> MK size (via increased DNA replication), and thereby  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> Platelets https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4114532/">https://www.ncbi.nlm.nih.gov/pmc/artic...
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> Platelets https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4114532/">https://www.ncbi.nlm.nih.gov/pmc/artic...
They DID find increased ploidy (DNA replication) of Megakaryocytes in the ID group
This suggests that iron deficiency causes
11/
But how does MK growth happen?
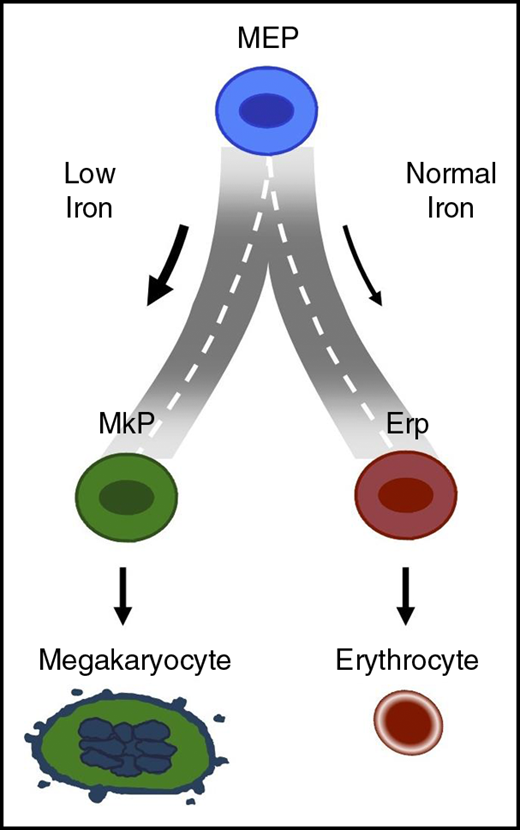
In a paper (which was a plenary session at @ASH_hematology ), Xavier et al looked at both mouse and human cell models for iron deficiency and found iron deficiency caused MK/erythrocyte precursors to preferentially develop into MKs.
But how does MK growth happen?
In a paper (which was a plenary session at @ASH_hematology ), Xavier et al looked at both mouse and human cell models for iron deficiency and found iron deficiency caused MK/erythrocyte precursors to preferentially develop into MKs.
12/
AND, the transferrin receptor was upregulated in the Fe-def models, while TFs previously known to regulate erythrocytes and MK maturation were no different.
I.e. MK/RBC progenitor cells shunted towards MKs via transf. receptor sensing https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> iron.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> iron.
( https://ashpublications.org/blood/article-abstract/134/18/1547/374971/Low-iron-promotes-megakaryocytic-commitment-of)">https://ashpublications.org/blood/art...
AND, the transferrin receptor was upregulated in the Fe-def models, while TFs previously known to regulate erythrocytes and MK maturation were no different.
I.e. MK/RBC progenitor cells shunted towards MKs via transf. receptor sensing
( https://ashpublications.org/blood/article-abstract/134/18/1547/374971/Low-iron-promotes-megakaryocytic-commitment-of)">https://ashpublications.org/blood/art...
13/
So again, why does iron deficiency cause thrombocytosis?
So again, why does iron deficiency cause thrombocytosis?
14/
Now of course that& #39;s only one type of answer to "why". One can also ask "why" from an evolutionary standpoint, or "why" only some patients with IDA have https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> platelets.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> platelets.
Now of course that& #39;s only one type of answer to "why". One can also ask "why" from an evolutionary standpoint, or "why" only some patients with IDA have
15/
We can only postulate here. Xavier et al propose:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔹" title="Kleine blaue Raute" aria-label="Emoji: Kleine blaue Raute">Perhaps thrombocytosis might confer a selective advantage in life-threatening hemorrhage (which may be a cause of IDA)?
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔹" title="Kleine blaue Raute" aria-label="Emoji: Kleine blaue Raute">Perhaps thrombocytosis might confer a selective advantage in life-threatening hemorrhage (which may be a cause of IDA)?
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔸" title="Kleine orangene Raute" aria-label="Emoji: Kleine orangene Raute">Perhaps limiting differentiation towards RBCs preserves iron for other necessary functions?
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔸" title="Kleine orangene Raute" aria-label="Emoji: Kleine orangene Raute">Perhaps limiting differentiation towards RBCs preserves iron for other necessary functions?
We can only postulate here. Xavier et al propose:
16/
But that& #39;s all for today!
Much acknowledgement to Xavier et al for a beautifully constructed set of experiments and adding greatly to the body of knowledge on this topic.
Hope you all enjoyed this (my first!) tweetorial. Hopefully many more to come!
But that& #39;s all for today!
Much acknowledgement to Xavier et al for a beautifully constructed set of experiments and adding greatly to the body of knowledge on this topic.
Hope you all enjoyed this (my first!) tweetorial. Hopefully many more to come!

 Read on Twitter
Read on Twitter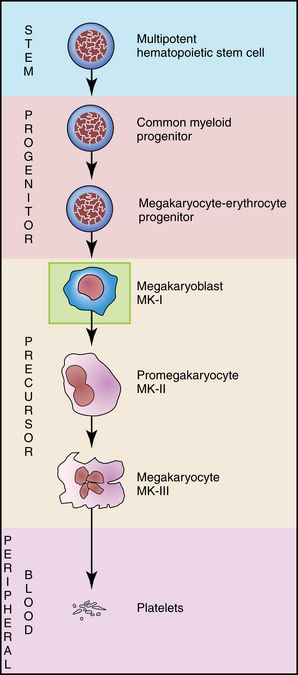 then to a MKhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="↪️" title="Nach rechts zeigender Pfeil mit Haken" aria-label="Emoji: Nach rechts zeigender Pfeil mit Haken"> which flicks off pieces of its cytoplasm to create plateletshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="↪️" title="Nach rechts zeigender Pfeil mit Haken" aria-label="Emoji: Nach rechts zeigender Pfeil mit Haken"> that then leave the BM and go out into the bloodstream.TPO (Thrombopoietin) drives this maturation process." title="6/The HSC progresses to a megakaryocyte (MK)/erythrocyte precursorhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="↪️" title="Nach rechts zeigender Pfeil mit Haken" aria-label="Emoji: Nach rechts zeigender Pfeil mit Haken"> then to a MKhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="↪️" title="Nach rechts zeigender Pfeil mit Haken" aria-label="Emoji: Nach rechts zeigender Pfeil mit Haken"> which flicks off pieces of its cytoplasm to create plateletshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="↪️" title="Nach rechts zeigender Pfeil mit Haken" aria-label="Emoji: Nach rechts zeigender Pfeil mit Haken"> that then leave the BM and go out into the bloodstream.TPO (Thrombopoietin) drives this maturation process." class="img-responsive" style="max-width:100%;"/>
then to a MKhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="↪️" title="Nach rechts zeigender Pfeil mit Haken" aria-label="Emoji: Nach rechts zeigender Pfeil mit Haken"> which flicks off pieces of its cytoplasm to create plateletshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="↪️" title="Nach rechts zeigender Pfeil mit Haken" aria-label="Emoji: Nach rechts zeigender Pfeil mit Haken"> that then leave the BM and go out into the bloodstream.TPO (Thrombopoietin) drives this maturation process." title="6/The HSC progresses to a megakaryocyte (MK)/erythrocyte precursorhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="↪️" title="Nach rechts zeigender Pfeil mit Haken" aria-label="Emoji: Nach rechts zeigender Pfeil mit Haken"> then to a MKhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="↪️" title="Nach rechts zeigender Pfeil mit Haken" aria-label="Emoji: Nach rechts zeigender Pfeil mit Haken"> which flicks off pieces of its cytoplasm to create plateletshttps://abs.twimg.com/emoji/v2/... draggable="false" alt="↪️" title="Nach rechts zeigender Pfeil mit Haken" aria-label="Emoji: Nach rechts zeigender Pfeil mit Haken"> that then leave the BM and go out into the bloodstream.TPO (Thrombopoietin) drives this maturation process." class="img-responsive" style="max-width:100%;"/>
 with time in both groups, TPO levels were similar between groups.IL-6 and IL-11 (also suggested as involved in IDA thrombocytosis) did rise in week 3 spec. in the ID group, but that rise came after the https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> in platelets." title="9/HOWEVER, while TPO https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> with time in both groups, TPO levels were similar between groups.IL-6 and IL-11 (also suggested as involved in IDA thrombocytosis) did rise in week 3 spec. in the ID group, but that rise came after the https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> in platelets." class="img-responsive" style="max-width:100%;"/>
with time in both groups, TPO levels were similar between groups.IL-6 and IL-11 (also suggested as involved in IDA thrombocytosis) did rise in week 3 spec. in the ID group, but that rise came after the https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> in platelets." title="9/HOWEVER, while TPO https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> with time in both groups, TPO levels were similar between groups.IL-6 and IL-11 (also suggested as involved in IDA thrombocytosis) did rise in week 3 spec. in the ID group, but that rise came after the https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> in platelets." class="img-responsive" style="max-width:100%;"/>