Delighted to present our paper in #BMJ today.
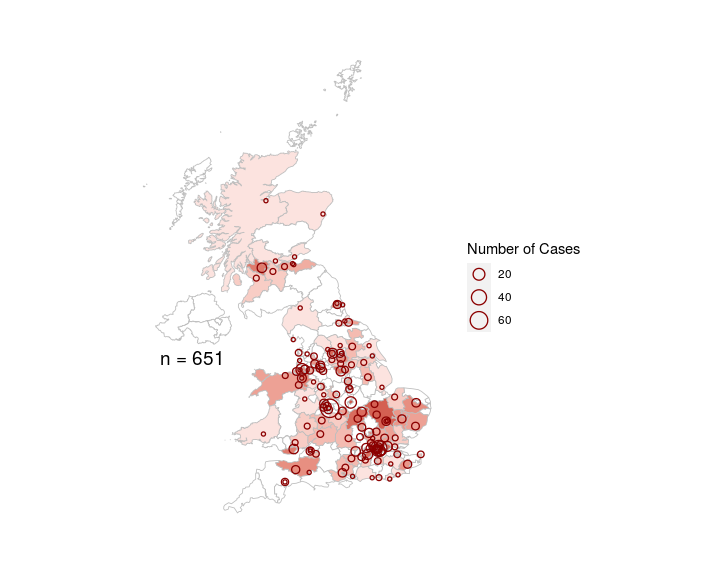
Detailed prospective study of 651 #children admitted with #SARSCoV2 across 138 UK hospitals
Here are some of the key findings: https://www.bmj.com/content/370/bmj.m3249">https://www.bmj.com/content/3...
Detailed prospective study of 651 #children admitted with #SARSCoV2 across 138 UK hospitals
Here are some of the key findings: https://www.bmj.com/content/370/bmj.m3249">https://www.bmj.com/content/3...
1. Severe disease was rare in children and death was extremely rare.
- Children under 19 made up less than 1% of all patients admited with #SARSCoV2 (651 / 69516 patients of all ages)
- Extremely low in-hospital mortality rate (<1% in children vs 27% in adults)
- Children under 19 made up less than 1% of all patients admited with #SARSCoV2 (651 / 69516 patients of all ages)
- Extremely low in-hospital mortality rate (<1% in children vs 27% in adults)
2. All 6 deaths were associated with profound comorbity / concurrent illness.
- 3 were neonates (1 = very premature, 1 = congenital abnorm, 1 = bacterial sepsis)
- 3 were 15-18 year olds (2 = profound neurodisability and 1 = malignancy on chemotherapy)
- 3 were neonates (1 = very premature, 1 = congenital abnorm, 1 = bacterial sepsis)
- 3 were 15-18 year olds (2 = profound neurodisability and 1 = malignancy on chemotherapy)
3. Analysis of symptoms found a systemic muco-enteric cluster (purple) which overlapped closely with the WHO criteria for Multisystem Inflammatory Syndrome in Children and Adolescents (MIS-C or PIMS-TS). This was quite separate to a respiratory cluster (green)
4. 18% of children hospitalised children were admitted to critical care
- Factors associated with critical care admission included age < 1m, age 10-14 years, black ethnicity and obesity
- Prematurity, respiratory and cardiac comorbidity also associated with critical care
- Factors associated with critical care admission included age < 1m, age 10-14 years, black ethnicity and obesity
- Prematurity, respiratory and cardiac comorbidity also associated with critical care
5. As a prospective study, we were able to follow the emergence of MIS-C in our cohort and found 52 children who met the WHO critiera for the syndrome. The earliest patient developed symptoms in mid March
6. Geographically, MIS-C was most common in the areas where the most children had been admitted with SARS-CoV2
7. Patients with MIS-C were older, (median age 10.7 yrs vs 1.6 years) and more likely to be of non-white ethnicity and to be obese than children who did not have MIS-C.
- Children with MIS-C were five times more likely to be admitted to critical care.
- Children with MIS-C were five times more likely to be admitted to critical care.
8. In addition to the WHO symptoms (gastrointestinal, rash and conjunctivitis), we found that patients with MIS-C were also more likely to have headache, sore throat and myalgia than those who did not.
9. Children with MIS-C were also more likely to have a platelet count of < 150 than those without MIS-C (32% vs 11%).
57% of patients with MIS-C had a cardiac complication
57% of patients with MIS-C had a cardiac complication
10. Children with MIS-C had different features depending on whether they were PCR positive or serology positive
11. - PCR positive children with MIS-C had more respiratory symptoms and were more likely to obese.
- Serology positive children were more likely to have cardiac complications and to receive IVIg and IV steroids
- Serology positive children were more likely to have cardiac complications and to receive IVIg and IV steroids
12. This paper is stuffed full of tables that we hope clinicians will find useful and we tried to look at these detailed data from as many angles as possible
13. Please do have a read. We hope it will be useful both for clinicians seeing children with #SARSCoV2, but also to reassure families as children go back to school in the UK.
14. Thank you to the incredible team who worked tirelessly as part of @ISARIC1 and @CCPUKstudy and the research nurses and medical students who helped collect the data.
15. Enormous thanks to @TweedieChap
@abdocherty79
@medcaremalawi
@LanceTurtle
@c_j_fairfield
@ShamezLadhani
@ewenharrison
@c_j_fairfield
@Tom_Drake1
@kennethbaillie
@p_openshaw
@OutbreakJake
@abdocherty79
@medcaremalawi
@LanceTurtle
@c_j_fairfield
@ShamezLadhani
@ewenharrison
@c_j_fairfield
@Tom_Drake1
@kennethbaillie
@p_openshaw
@OutbreakJake
How could I forget @wheezylikesund1 ! Sorry!

 Read on Twitter
Read on Twitter