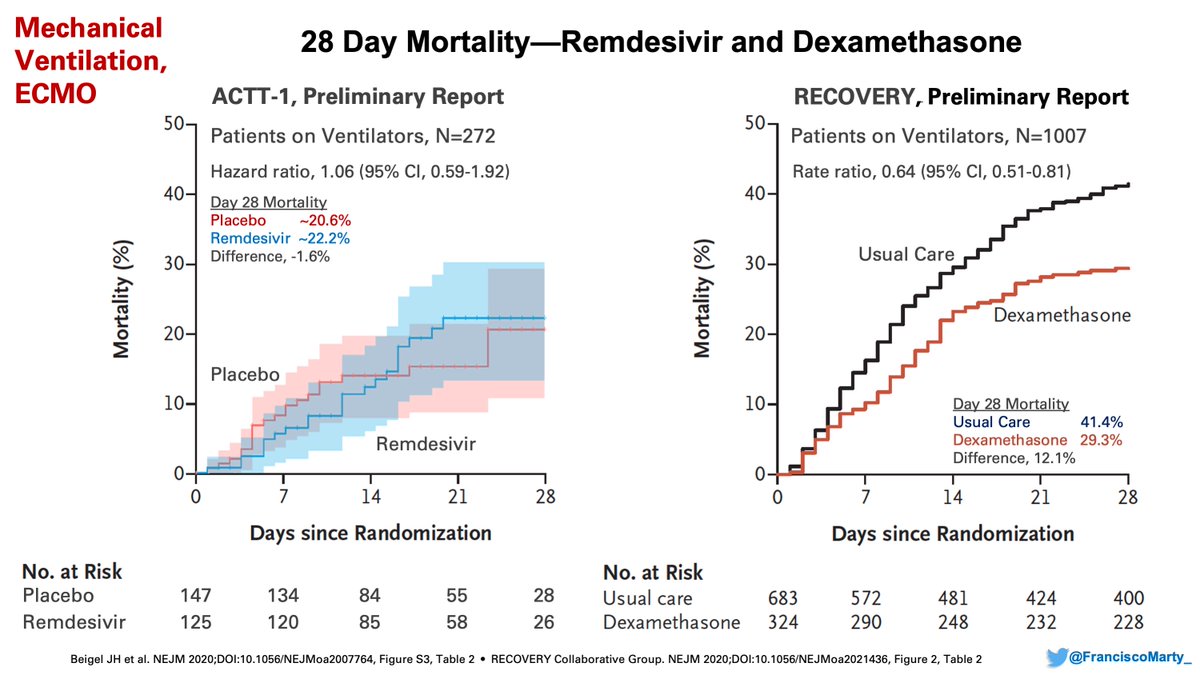
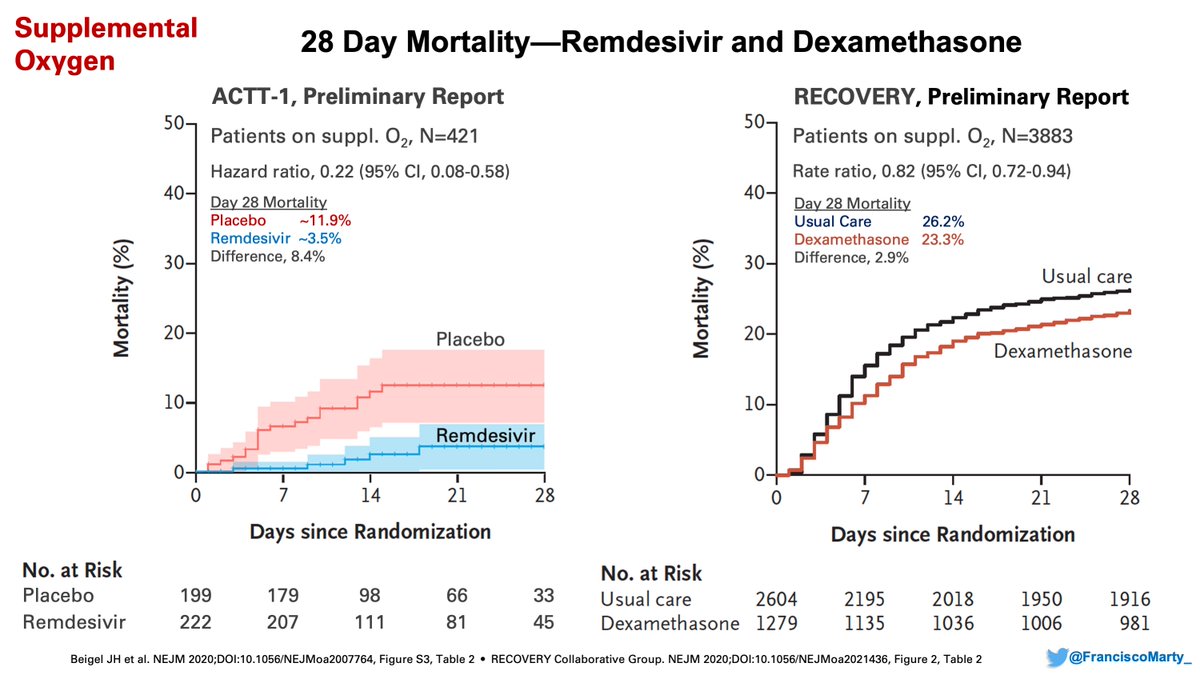
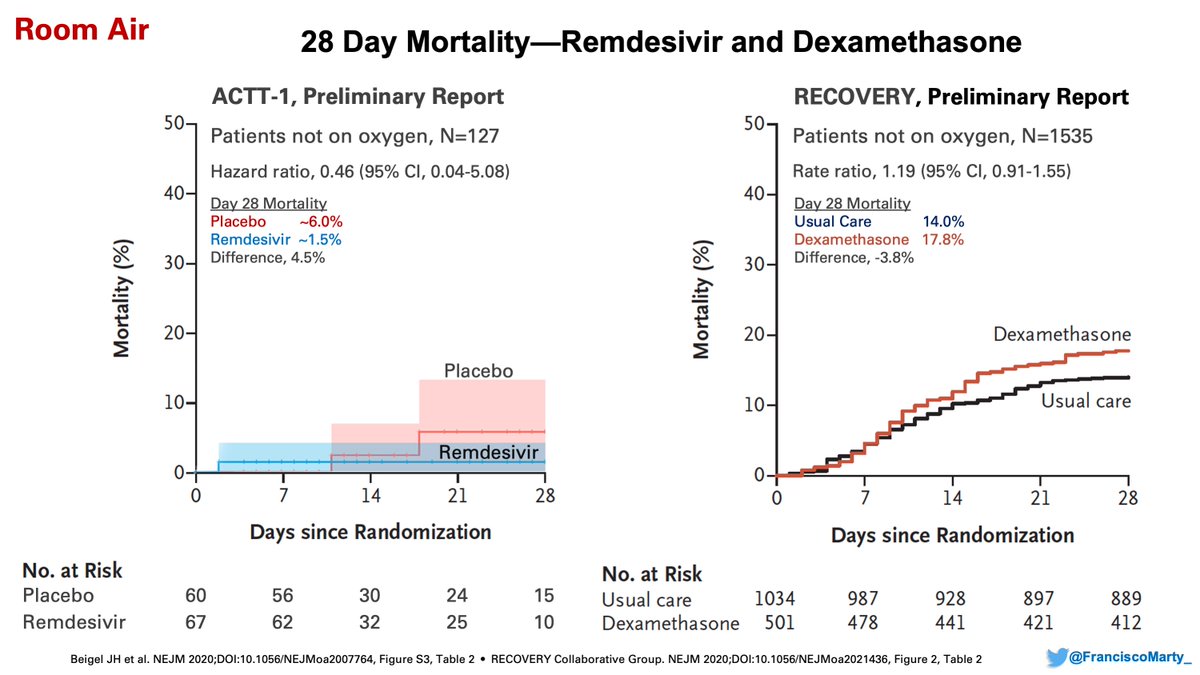
Have been thinking on useful lessons from #COVID19 randomized treatment trials published to date, want to explore the disease spectrum of clinical #SARSCoV2 infection (aka, CoViDisease) and put some ideas we can discuss and see if they can help with interpretation & new designs.
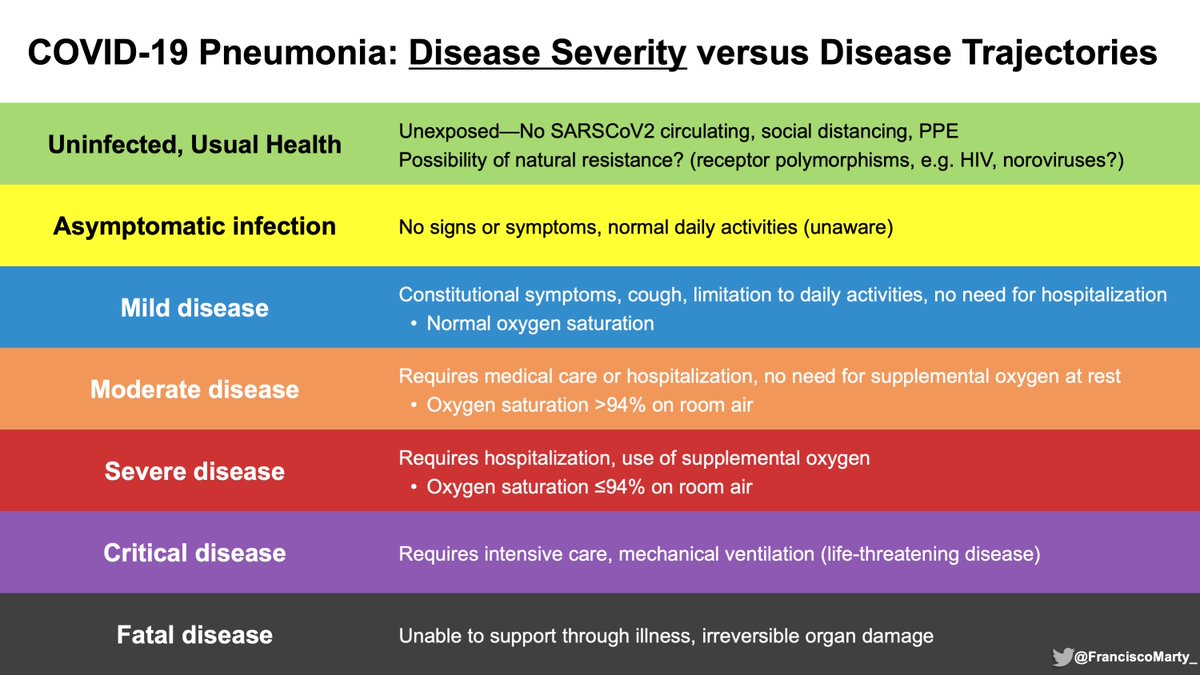
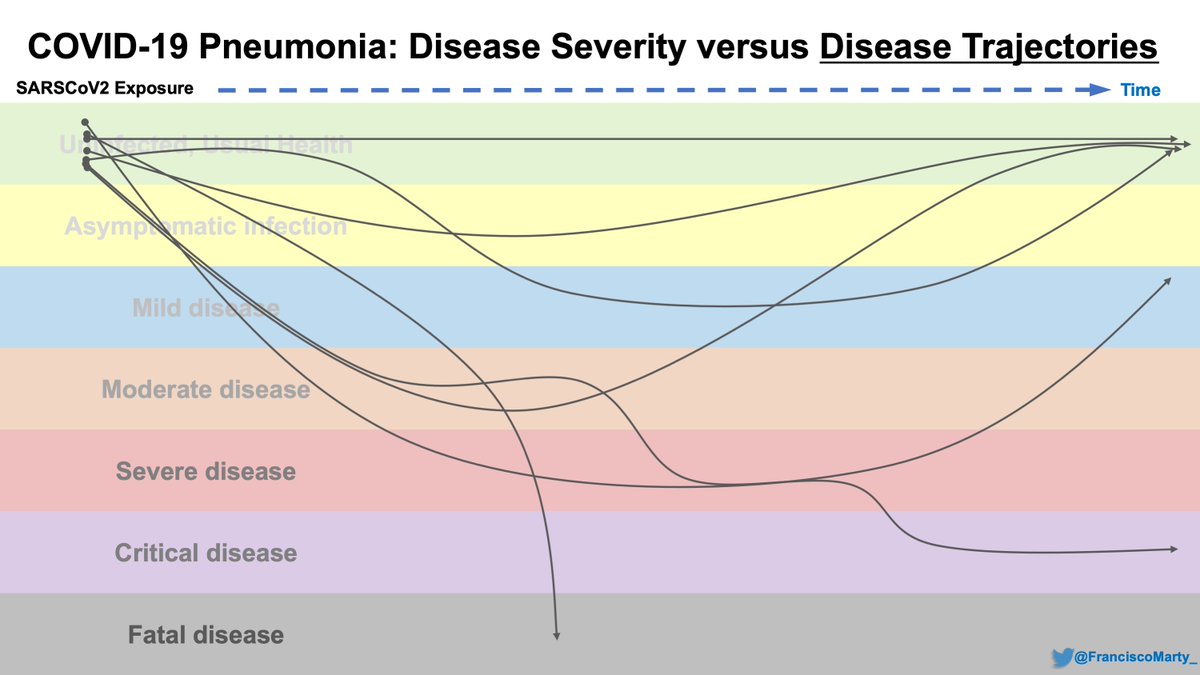
This is a summary slide of rather clean #COVID19 disease classification based on pulmonary disease severity.
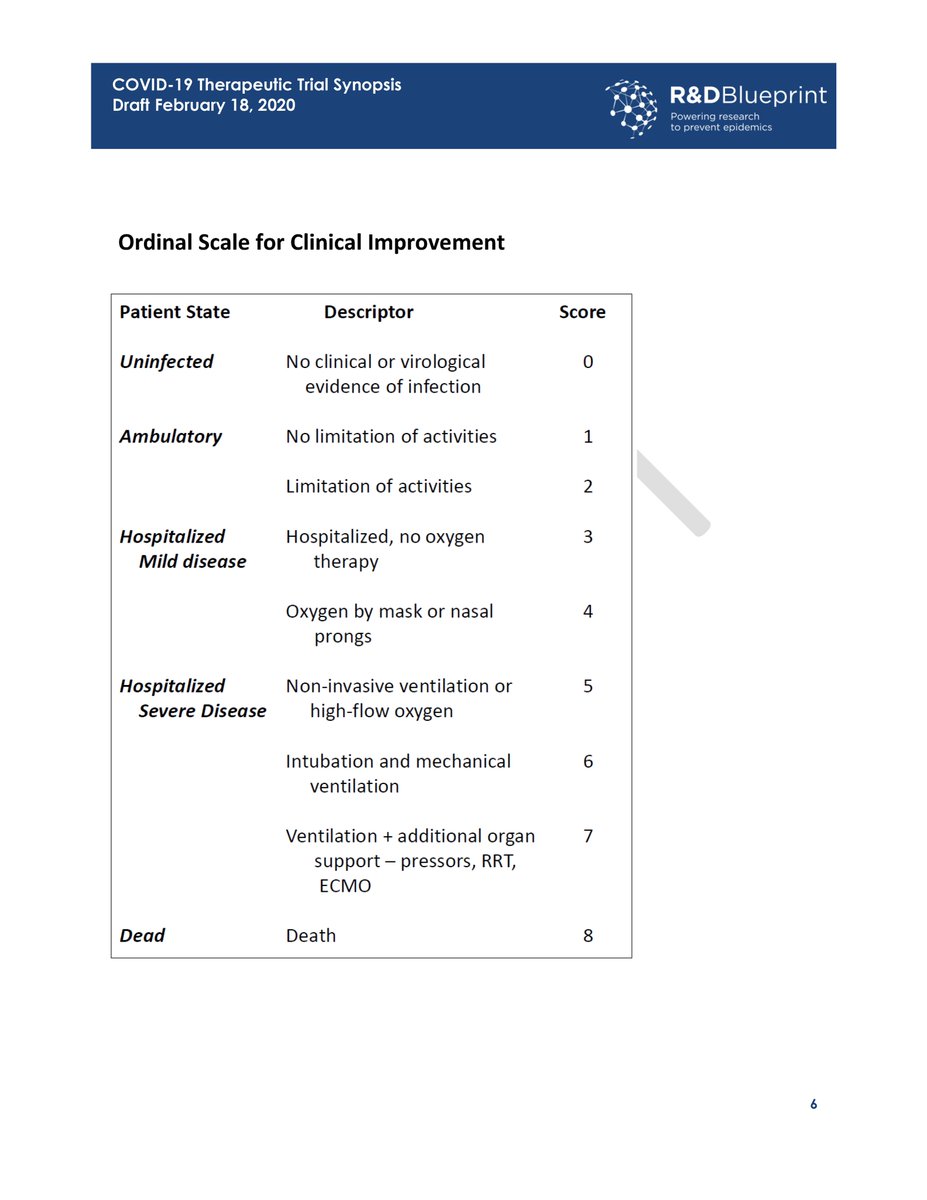
As the #WHO ordinal scale that we plugged into play with the first set of trials, it is based on care needs (home vs. hospital) and oxygen and ventilatory support offered.
As the #WHO ordinal scale that we plugged into play with the first set of trials, it is based on care needs (home vs. hospital) and oxygen and ventilatory support offered.
This is kind of basic, but important, as many people and trials are not specific on what they mean by #mild, #moderate, #severe #COVID19 disease.
For a general doctor, being hospitalized or on oxygen is #severe #COVID19, but for an #ICU doctor, is #mild, does not need ICU care.
For a general doctor, being hospitalized or on oxygen is #severe #COVID19, but for an #ICU doctor, is #mild, does not need ICU care.
I think the #WHO #ordinal scale was a useful initial tool that was able to be put into play quickly in the pandemic, but I think it has limitations and biases that are affecting how study results are interpreted by many.
link (still a draft since 2/2020): https://www.who.int/blueprint/priority-diseases/key-action/COVID-19_Treatment_Trial_Design_Master_Protocol_synopsis_Final_18022020.pdf">https://www.who.int/blueprint...
link (still a draft since 2/2020): https://www.who.int/blueprint/priority-diseases/key-action/COVID-19_Treatment_Trial_Design_Master_Protocol_synopsis_Final_18022020.pdf">https://www.who.int/blueprint...
Some issues with the scale
1. It is #ICU and #Hospital centric, does not represent the majority of those sick with #COVID19
2. many of the levels of severity depend on modes of #oxygenation that are not available or are very limited in many places
3. Why is #ECMO featured...?
1. It is #ICU and #Hospital centric, does not represent the majority of those sick with #COVID19
2. many of the levels of severity depend on modes of #oxygenation that are not available or are very limited in many places
3. Why is #ECMO featured...?
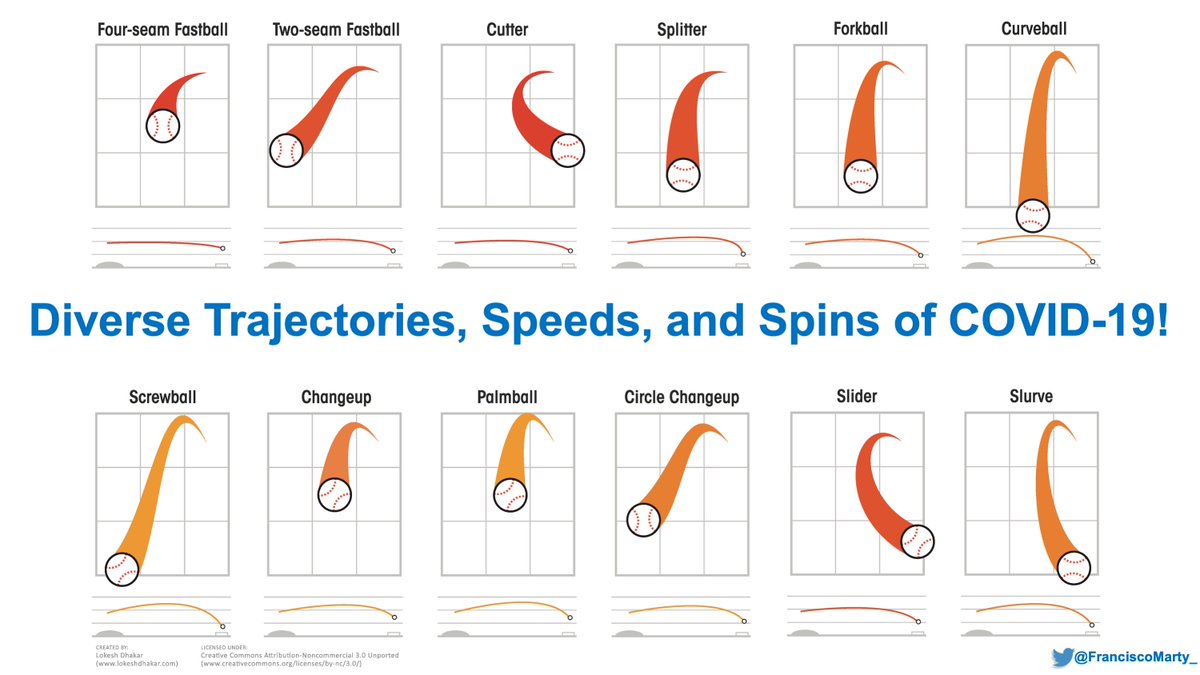
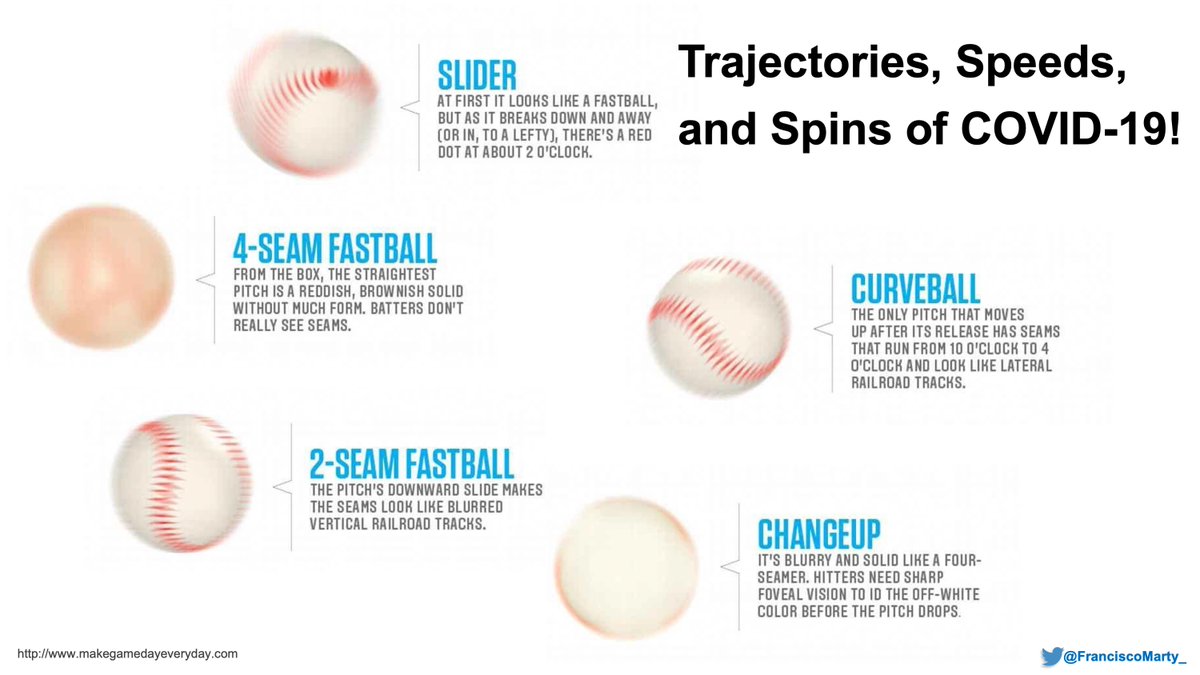
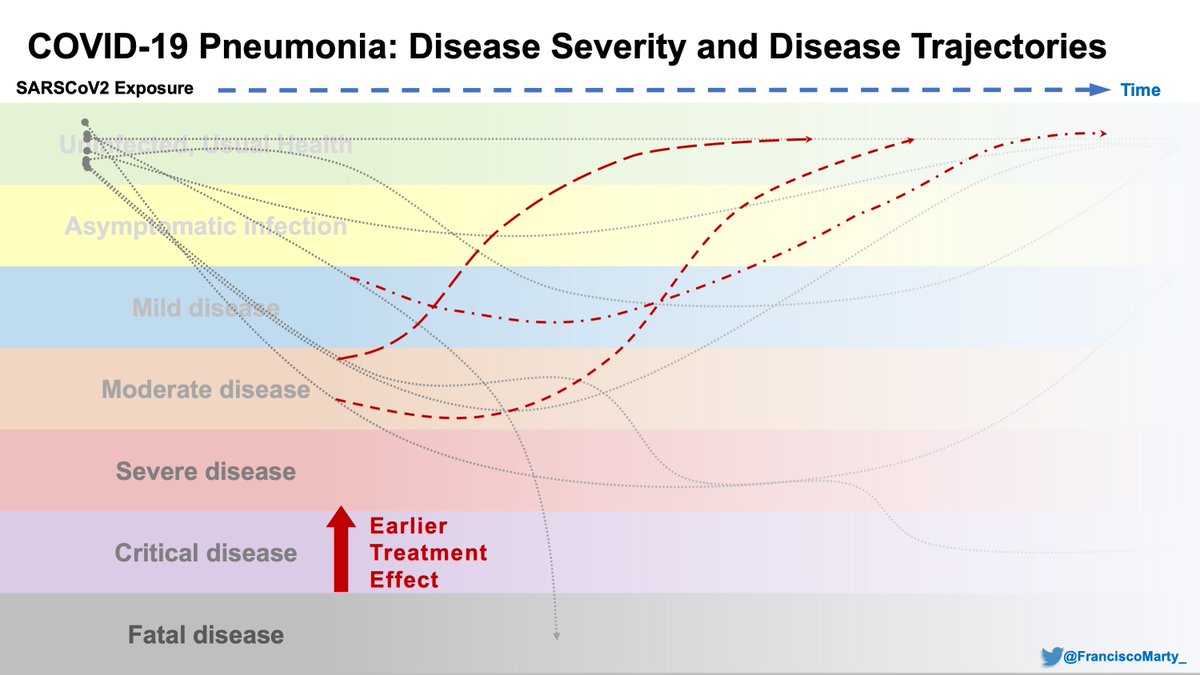
The severity scale suggests patients progress in a stepwise, almost magical manner from one band to the other, but it is devoid of time or the sense of trajectory, an important concept in infectious diseases, the hardest one to teach according to my mentor Bob Rubin, so some
baseball to help with this idea
It is easy to see the trajectory of a ball after the catcher has caught it (lines below each square), but batters are constantly trying to anticipate speed, spin, and type of pitch they are getting so they can hit the ball
It is easy to see the trajectory of a ball after the catcher has caught it (lines below each square), but batters are constantly trying to anticipate speed, spin, and type of pitch they are getting so they can hit the ball
on the wards during the first pandemic #COVID19 wave, it was clear to me that patients had different trajectories of their disease before and after hospitalization.
Some literally crashed and burned in just 3-5 days, they did not read the fairy tale of viral, then immune fase
Some literally crashed and burned in just 3-5 days, they did not read the fairy tale of viral, then immune fase
Their #COVID19 disease had different speeds, spins, some with GI-predominant disease, other odd manifestations, not really captured in trials to date.
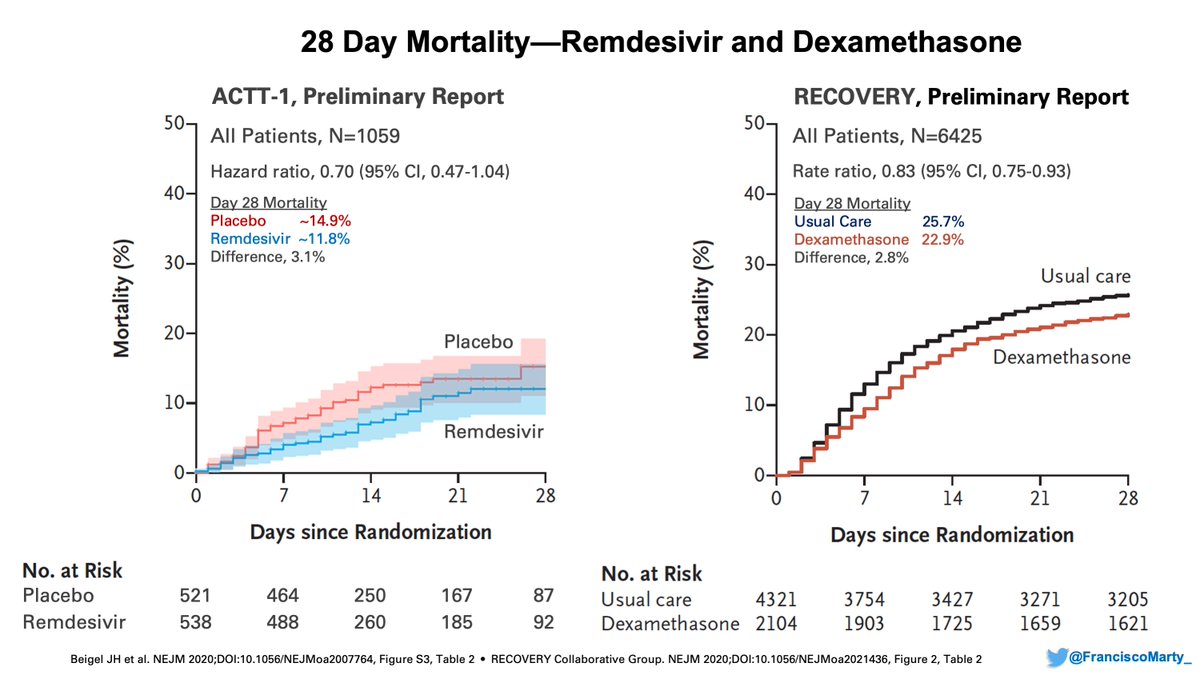
What we hoped on our first rushed trials, before we even understood the disease well (still only beginning to), is that #COVID19 treatments will "recover" patients, bring them up on the scale, or more nuanced, change their disease trajectory over time.
I find fascinating and puzzling is that for hospitalized patients with #COVID19, their disease severity (score, scale) at randomization has been the strongest predictor of their outcome in the trials we have done so far.
Note that the median time of symptoms has been 9-10 days.
Note that the median time of symptoms has been 9-10 days.
At the same time we have (more or less understandably) over-focused on the sickest and on complex care (buying ventilators, expanding hospitals). This is care I have been trained to do and we excel at where I work, but we may be need a different batting approach to these pitchers
We need to take the study and trials of #COVID19 outside of the hospital, switch scales, outcomes to more meaningful ones, even if it is not death.
I was looking for an example in #StrepThroat, bumped into fascinating stories I was not really taught in school or fellowship (maybe because penicillin is generic, or because it was not sexy anymore.
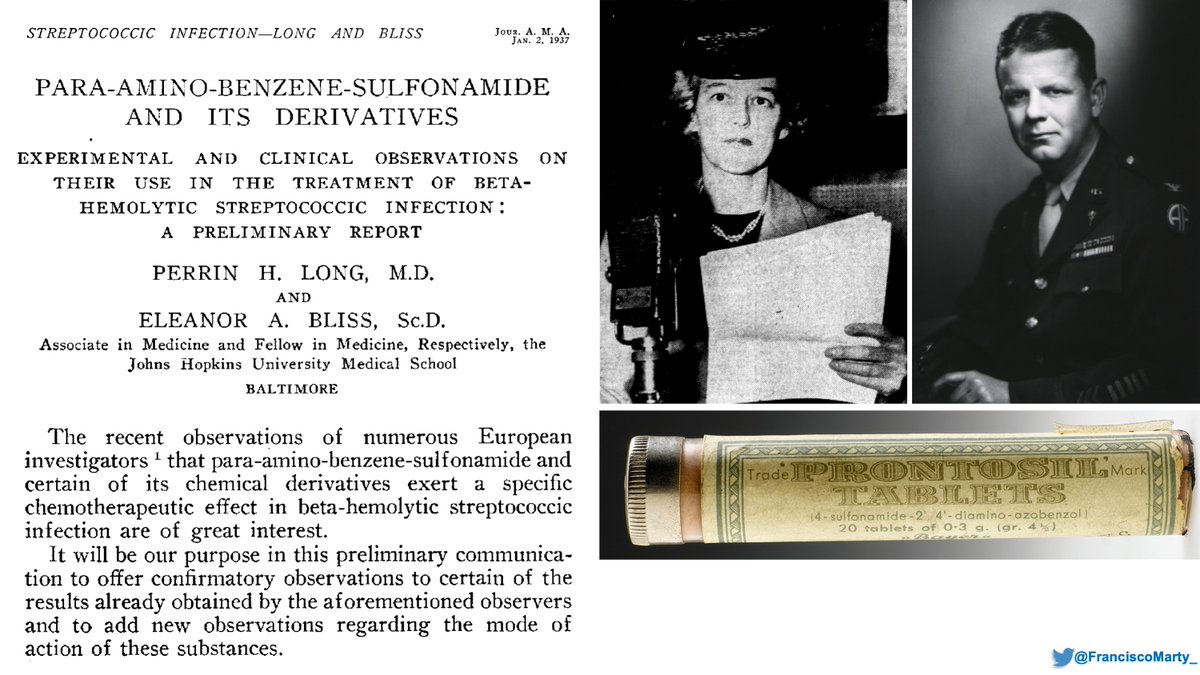
Here is the first sulfonamide use for #streptococcal disease in the US, 1937.
Here is the first sulfonamide use for #streptococcal disease in the US, 1937.
The first randomized controlled trial was 12 years away, but it became clear very quickly that sulfonamides would change the course of regularly fatal illnesses.
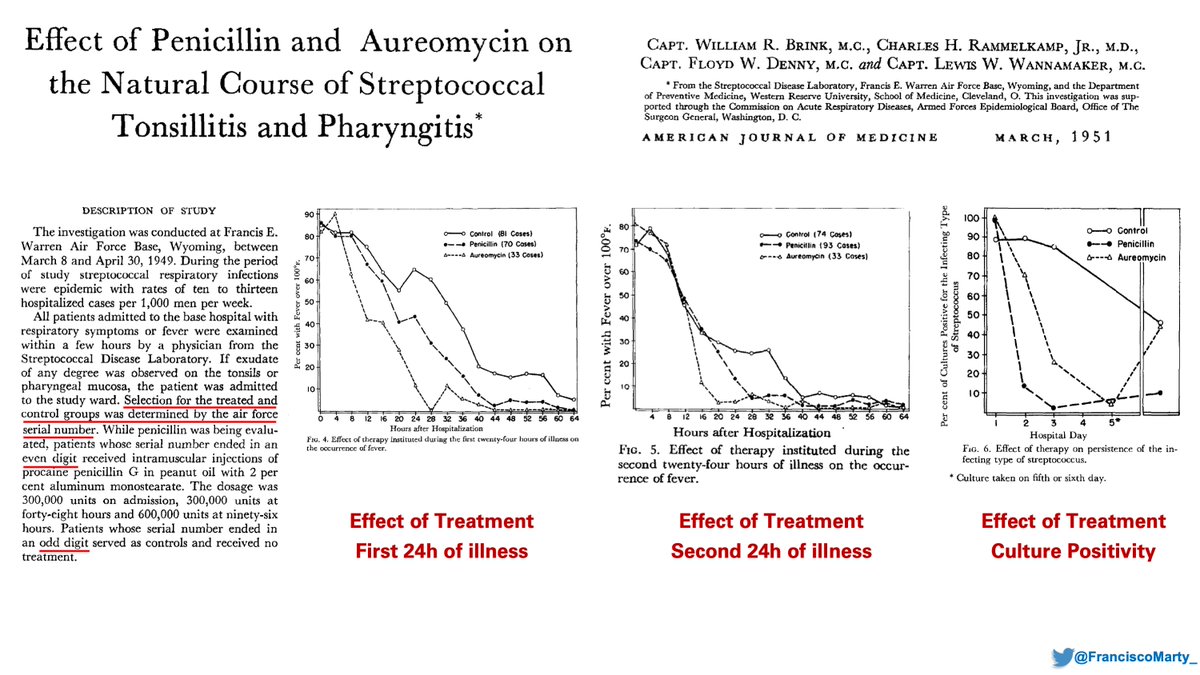
This was a fun find (1951)
1. Not randomized, but using even/odd IDs for selection
2. Treating recruits within 1 day, nicely beneficial, wait another day, not much difference.
3. If a fixed outcome time had been selected (72 hours) this would have been a negative study.
1. Not randomized, but using even/odd IDs for selection
2. Treating recruits within 1 day, nicely beneficial, wait another day, not much difference.
3. If a fixed outcome time had been selected (72 hours) this would have been a negative study.
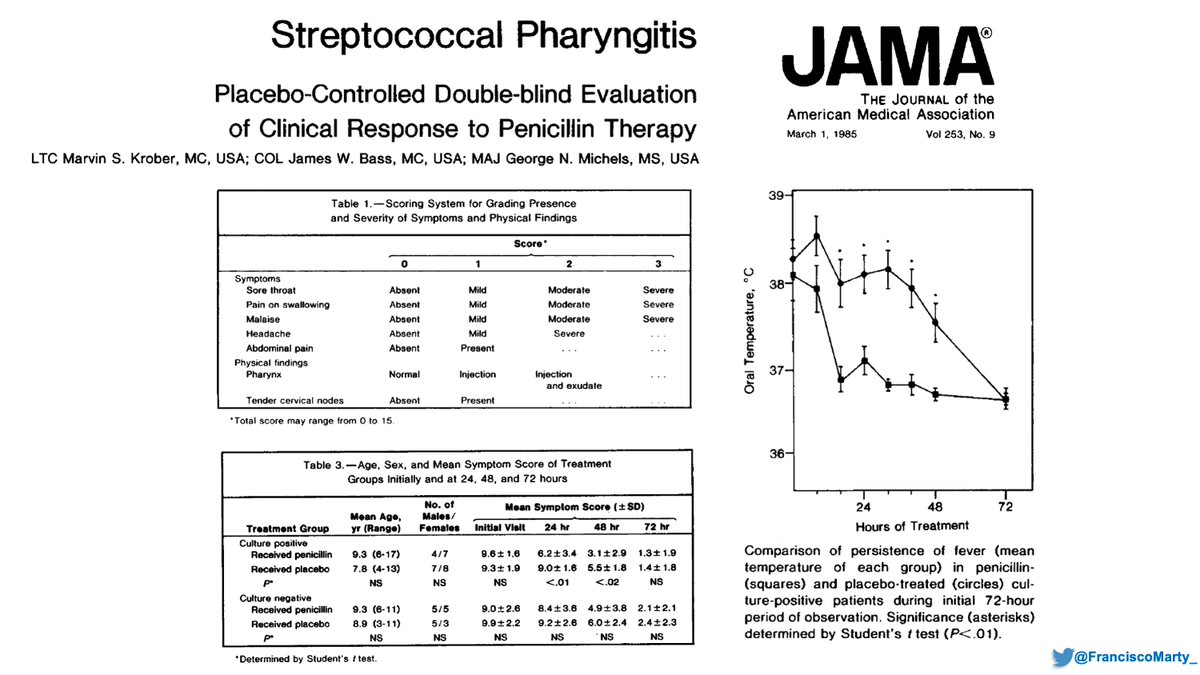
But it took 50 years for some to get their act together and do a modern trial on #StrepThroat. All were small with very interesting findings.
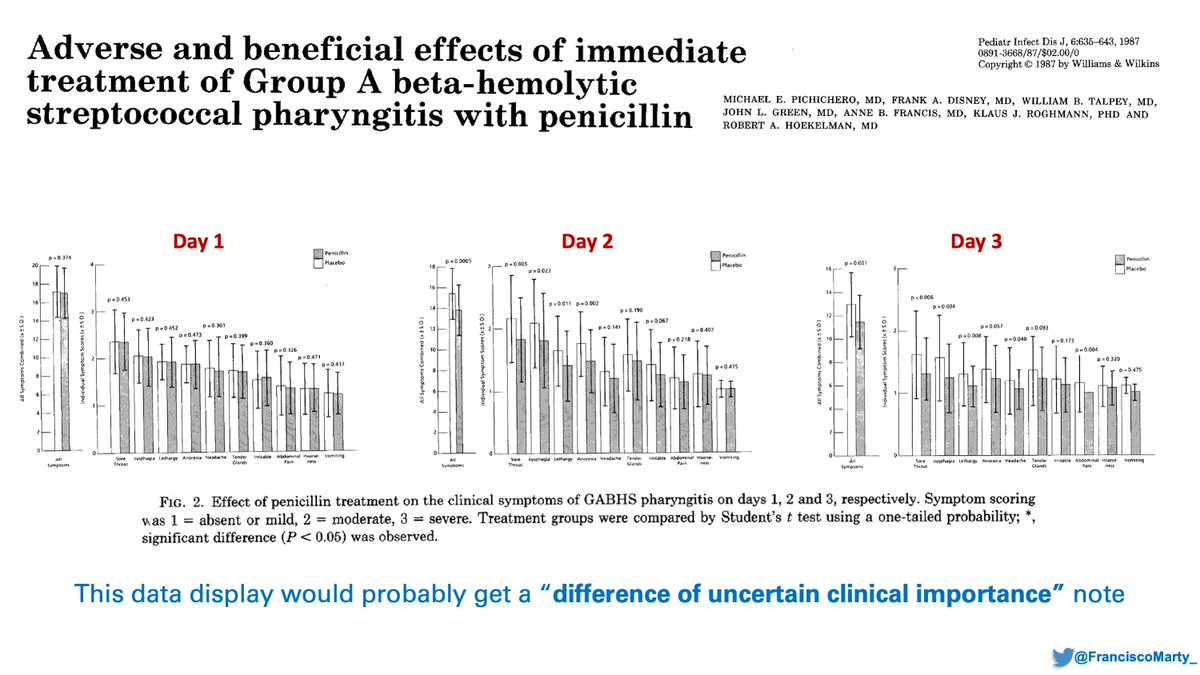
This trial was cool as it was randomized, double blind, with immediate vs. delayed treatment (1987_. A clean abstract with pros-cons, done in a private practice in Rochester, NY.
But once you start looking at multiple variables, maybe you start thinking is not that much of a deal breaker.
But we spend a lot of resources on strep-throat because we want
- children to get better
- to prevent transmission
- to avoid, heart, kidney, other complications
But we spend a lot of resources on strep-throat because we want
- children to get better
- to prevent transmission
- to avoid, heart, kidney, other complications
So back to #COVID19, maybe we want to treat earlier, we want to arrest the disease process so we don& #39;t see all the immunologic, hematological complications we have seen, we unload the system.
Vaccines will help if and when they work, but what do we do in the mean time?
Vaccines will help if and when they work, but what do we do in the mean time?
I think we want to intervene earlier (<5-7 days), catch people that crash-and-burn before they end up in the hospital, minimize the long recovery phase by minimizing organ injury to others
It will mean treating people who may never get too sick, but maybe we prevent transmission.
It will mean treating people who may never get too sick, but maybe we prevent transmission.
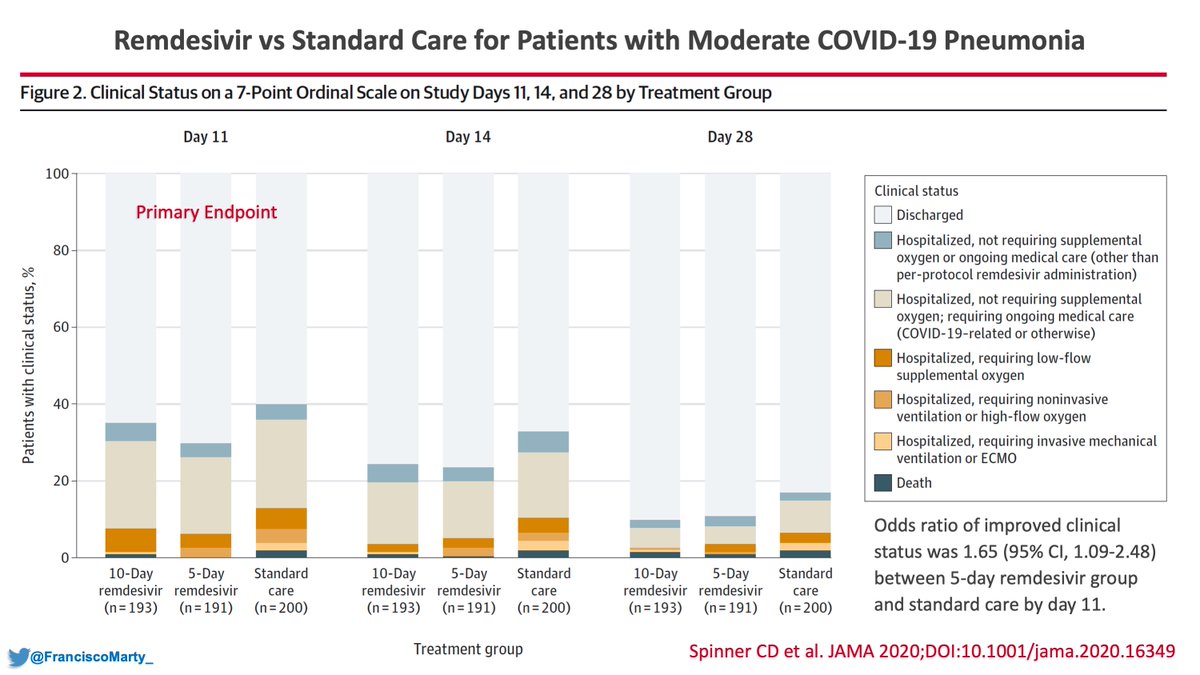
I feel a bit like the #StrepThroat researcher who sees the benefit a randomized intervention having done the #remdesivir treatment trial for moderate #COVID19 disease, yet using different scales, others can miss the certainty where gains and benefits are.
https://ja.ma/32u0OUc ">https://ja.ma/32u0OUc&q...
https://ja.ma/32u0OUc ">https://ja.ma/32u0OUc&q...

 Read on Twitter
Read on Twitter