in EM we love clinical decision tools, risk stratification tools. HEART, Canadian (___), Wells, PERC, Ottawa (__)...but, what do we really know about them? a short thread from the talk (1/) https://twitter.com/BaystateEM/status/1297904123216564225">https://twitter.com/BaystateE...
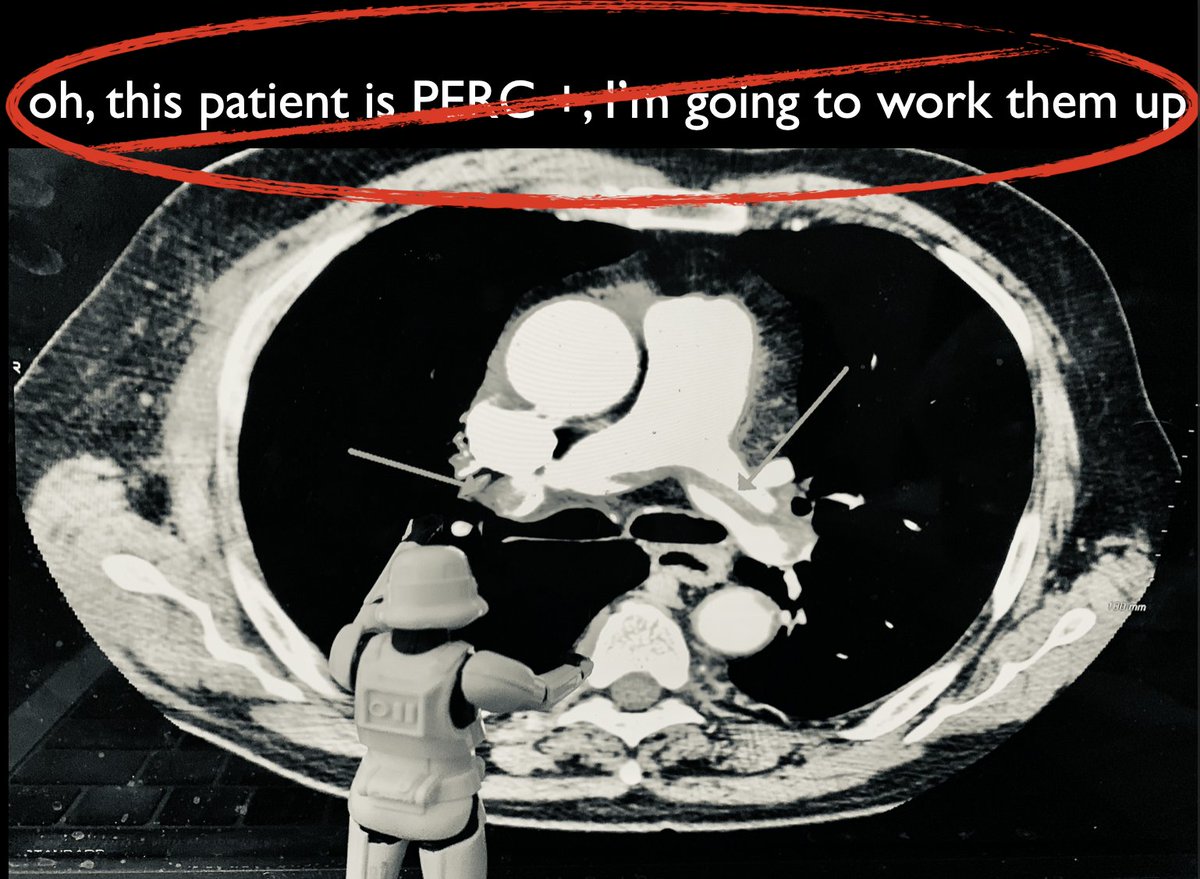
Know if it& #39;s a 1-way tool or a 2-way tool? A 2-way tool is a bit easier to use b/c it tells you when to act and when not to (i.e. scan or don& #39;t scan - Canadian head/c-spine, Ottawa ankle etc). 1-way tools tell you - if negative, don& #39;t do X.. but...it& #39;s tempting to use as 2-way
It& #39;s helpful to know *how* the tool was derived. How were the variables determined? Inclusion and exclusion criteria are also important (can help avoid indication creep & ensure right patient population) - eg. Canadian head CT often applied to trivial injury
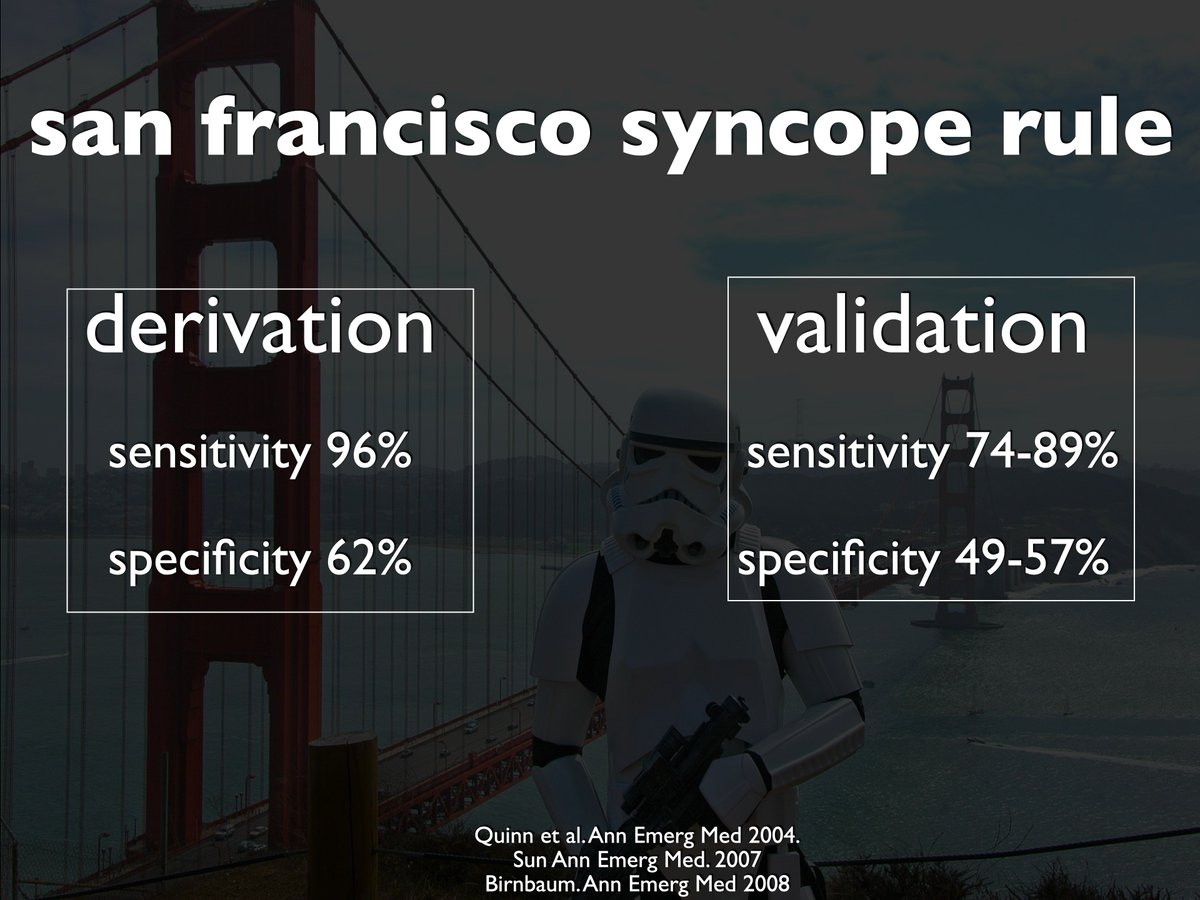
Has the tool been validated? Where? How (ideally prospectively)? This is important because you want to make sure it & #39;works& #39;, especially outside of a single population and by various clinicians
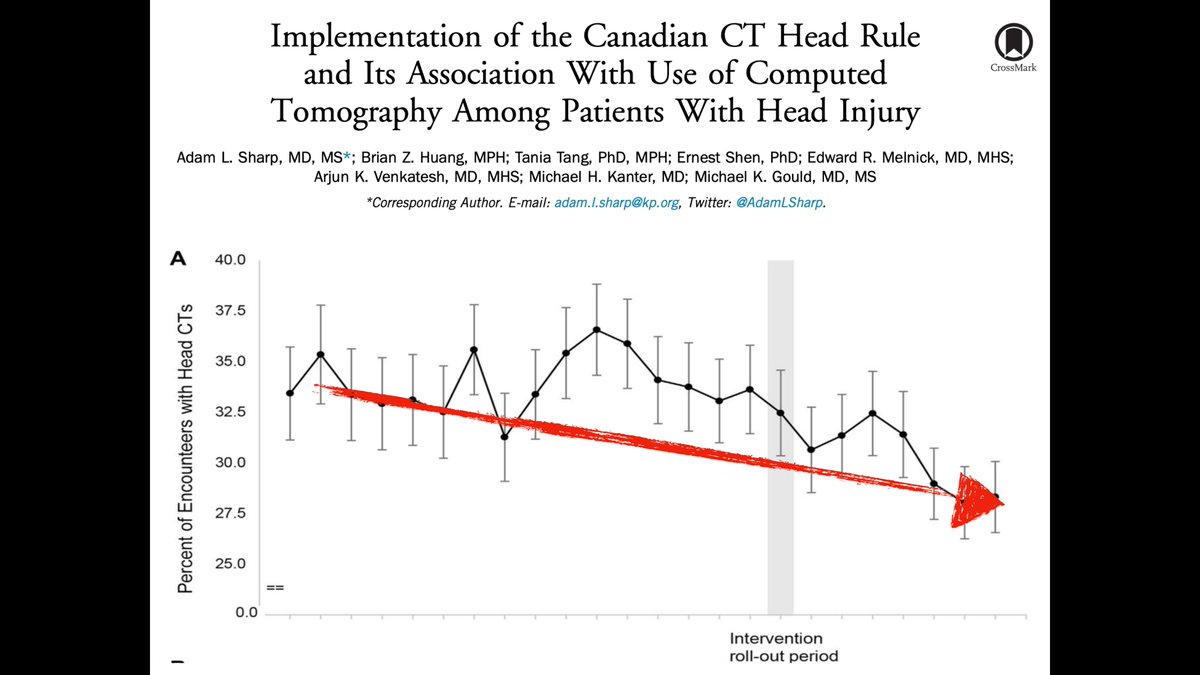
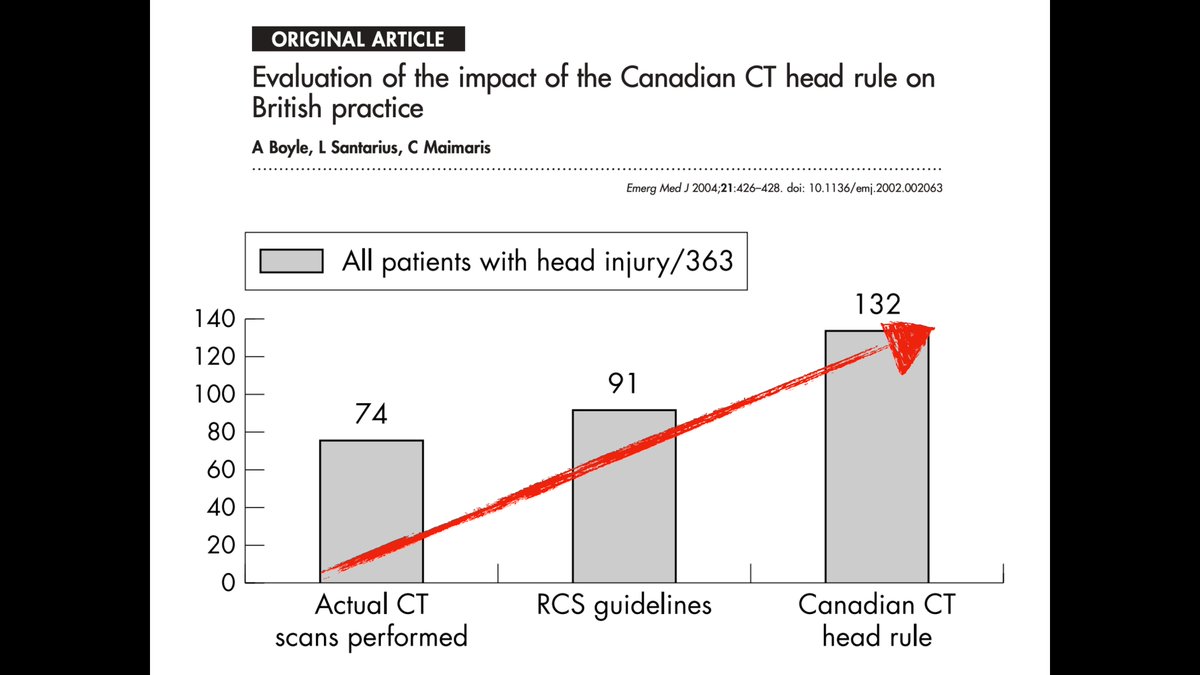
What is the impact of the clinical decision tool? Has an impact analysis been done? These tools may perform well in different environments (eg. imaging tools may actually *increase* ordering in places outside the US or places that don& #39;t have wild overtesting issues)
Of course, the biggest thing is...does the tool add value over gestalt? This will very much depend on the clinician and local milieu. People love to cite https://pubmed.ncbi.nlm.nih.gov/28238497/ ">https://pubmed.ncbi.nlm.nih.gov/28238497/... as "proof that my gestalt is just as good"...but a lot of this depends on *what* you& #39;re measuring
Are you measuring probability of PE? Or are you measuring if (and how) clinicians evaluate for PE (the action that actually reaches the patient)? This meta-analysis found ↑ CT yield (kind of a proxy for appropriate ordering) with decision tools https://pubmed.ncbi.nlm.nih.gov/26747217/ ">https://pubmed.ncbi.nlm.nih.gov/26747217/...
Despite being ubiquitous & amazing resources to help us use them, clinicians misuse and misinterpret these toools https://pubmed.ncbi.nlm.nih.gov/32220127/ ">https://pubmed.ncbi.nlm.nih.gov/32220127/... So..when you use a decision tool,know how you& #39;re supposed to use it, look it up (everytime...) & think about why you& #39;re using it/added value

 Read on Twitter
Read on Twitter