Treatment for #COVID19 has improved and there may be some & #39;mortality displacement& #39; effect with a proportion of the most at-risk population having deceased in the spring epidemic. Both factors could contribute to reducing mortality during a & #39;winter wave& #39;. (1/6) https://twitter.com/jengleruk/status/1294010284424732673">https://twitter.com/jengleruk...
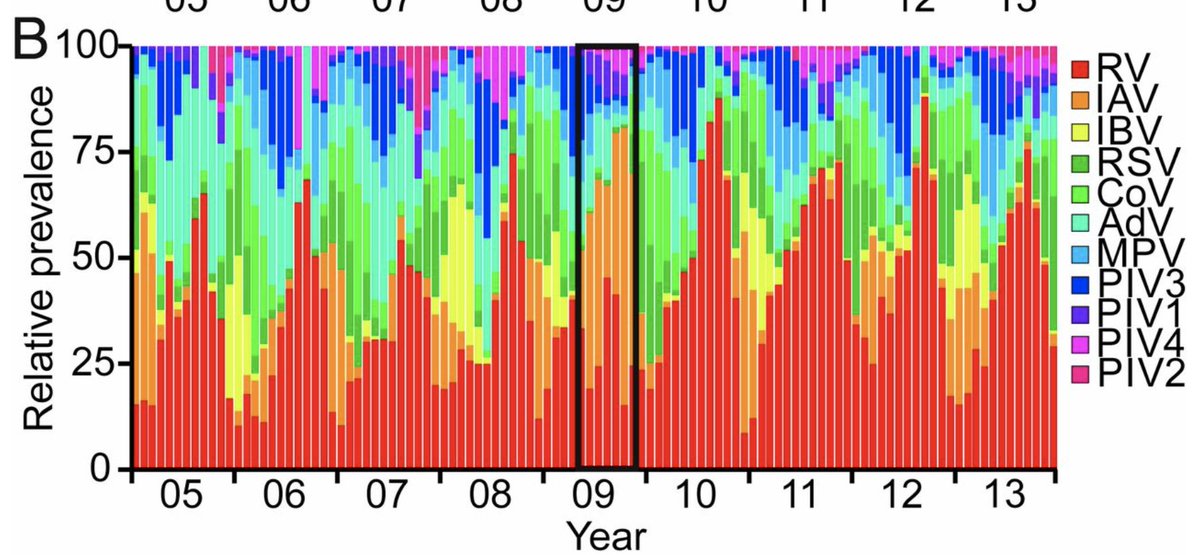
There are many other factors that have a seasonal component. Though, the big unknown is how #SARSCoV2 will interact with the other >200 seasonal respiratory viruses in circulation, which are involved in complex population dynamics (e.g. below). (2/6)
https://www.pnas.org/content/116/52/27142">https://www.pnas.org/content/1...
https://www.pnas.org/content/116/52/27142">https://www.pnas.org/content/1...
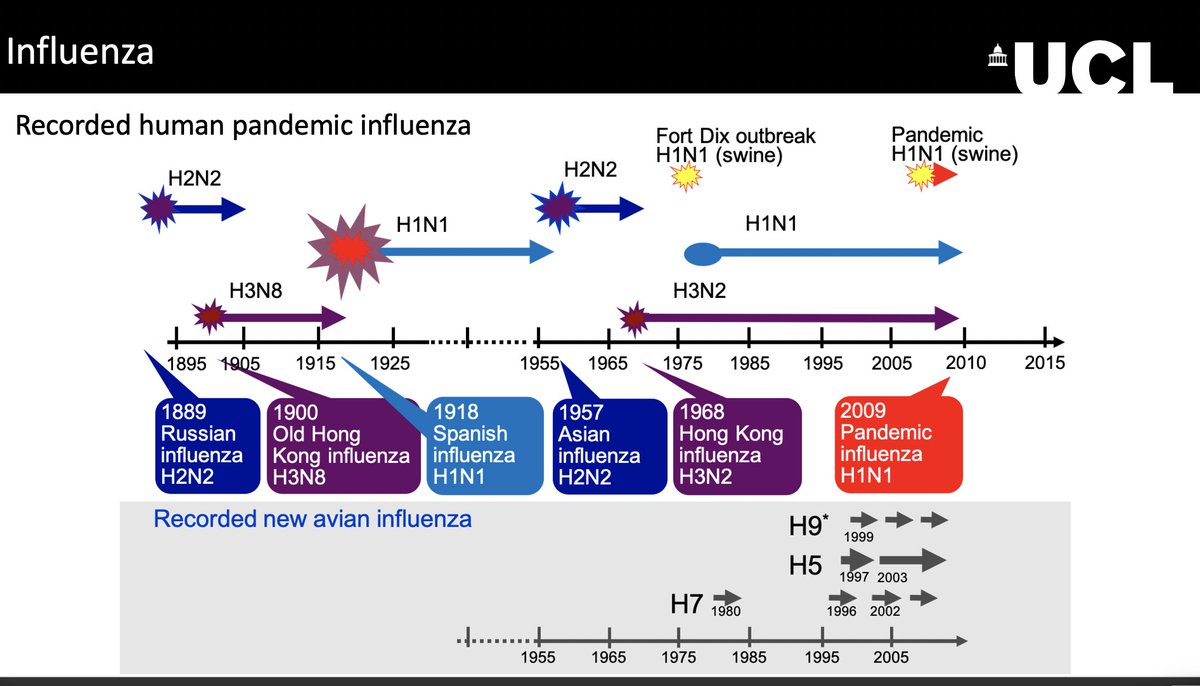
#SARSCoV2 might enter in synergistic interactions with other viruses. One - entirely hypothetical - but worrisome scenario would be for co-infection with the flu to lead to particularly severe. A bad flu season, on top of #COVID19 would also challenge healthcare capacity. (3/6)
Conversely the #COVID19 winter epidemics could be mitigated by #SARSCoV2 getting in competition with other viruses (e.g. common cold coronaviruses), either directly, or through cross-immunisation. Such negative interactions might reduce #COVID19 spread and mortality. (4/6)
This is what may have happened in the 2009 flu pandemic winter wave, which never really was. The 2009 H1N1 pandemic strain failed to displace the influenza strains in circulation, possibly due to cross-immunity with the 1918 H1N1 strain, which is still around to this day. (5/6)

 Read on Twitter
Read on Twitter