It’s time for another #MCQMonday - this week we’re thinking about optimal #COPD treatment - here’s our Q. #RespEd #loveyourlungs #SCE #RespisBest
Q. Which one of the following is the most appropriate treatment plan? 2/n
We didn’t quite get round to posting the answer last night. We blame the heat! But it’s still Wednesday in Hawaii so we’re claiming that as our spiritual home! The answer was of course - add LABA. 80% of you were correct 3/n
This patient has moderate airflow obstruction (GOLD stage 2). He has had only 1 exacerbation, not requiring hospitalisation, but has persistent daily symptoms with CAT >18 and mMRC>/=2. He therefore falls into GOLD grade B when assessing severity of #COPD. 4/n
Importantly he has received high quality care, with a focus on the highest value interventions in #COPD - smoking cessation, pulmonary rehabilitation & vaccination.
5/n
5/n
So let’s focus on inhaled drugs. LABAs & LAMAs are bronchodilators. They cause smooth muscle relaxation & increased airflow. But wait, isn& #39;t the hallmark of COPD that it is a fixed airways disease without reversibility? 6/n
Yes, bronchodilators have little measurable effect on FEV1 at rest, but they reduce dynamic hyperinflation and measurably increase exercise performance e.g. this study using tiotropium https://erj.ersjournals.com/content/23/6/832">https://erj.ersjournals.com/content/2... @erspublications 7/n
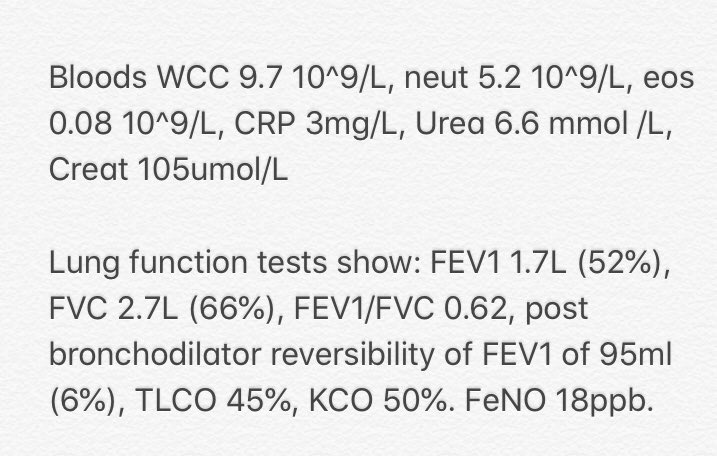
Ok first let’s think about LABAs. They act on beta adrenergic receptors, increase cAMP & prevent bronchoconstriction. They improve lung function, dyspnoea, health status, & reduce exacerbation rates. 8/n (image from @EurekaMedicine)
LABAs have no measurable effect on mortality or rate of decline of lung function. https://www.cochrane.org/CD010177/AIRWAYS_long-acting-beta2-agonists-for-people-with-copd.">https://www.cochrane.org/CD010177/... @CochraneAirways 9/n
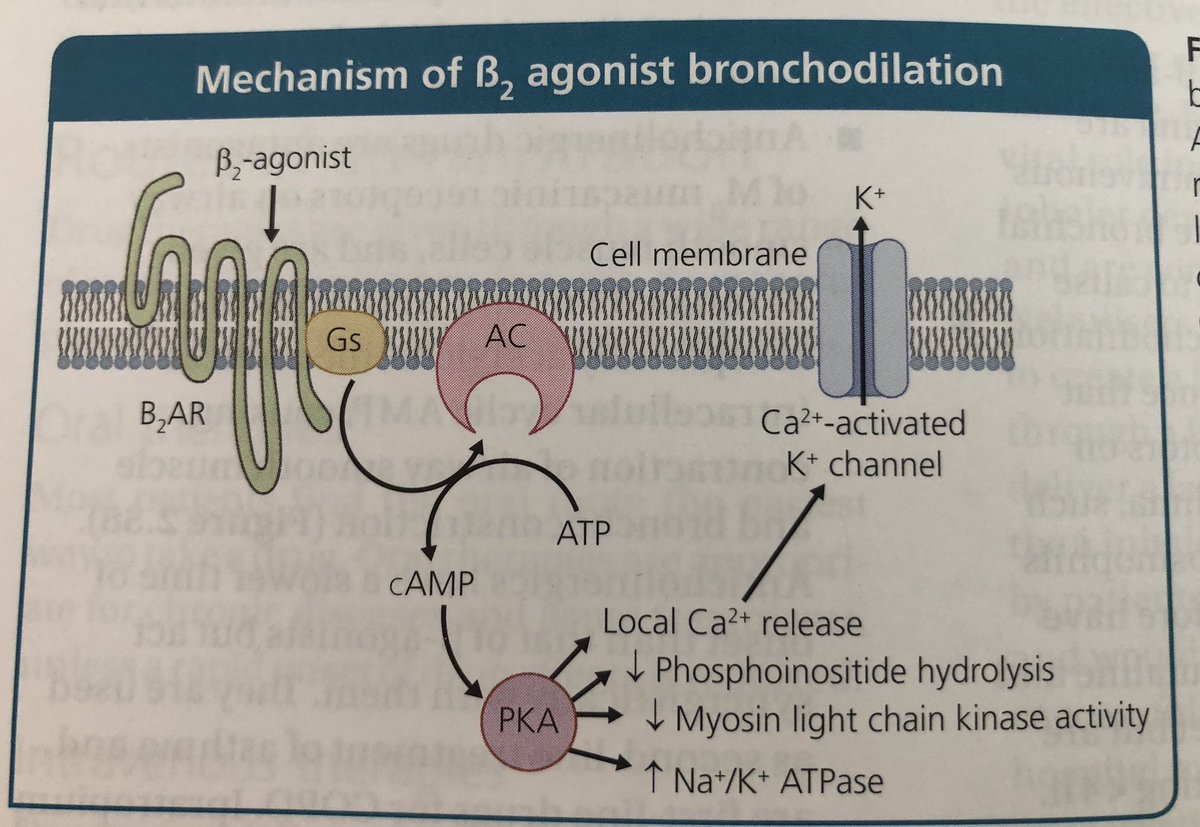
LAMAs block bronchoconstrictor effects of ACh on M3 muscarinic receptors. LAMAs improve symptoms & health status, reduce exacerbations & hospitalisations, & improve the effectiveness of pulmonary rehabilitation https://www.sciencedirect.com/science/article/abs/pii/S0012369215310886">https://www.sciencedirect.com/science/a... in @accpchest 10/n (image: @EurekaMedicine)
Clinical trials have shown a greater reduction in exacerbation rate with LAMAs vs LABAs, which is why guidelines recommend LAMA as first line treatment in patients with #COPD on monotherapy. Eg @LancetResp INVIGORATE trial indacaterol vs tiotropium
https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(13)70158-9/fulltext">https://www.thelancet.com/journals/... 11/n
https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(13)70158-9/fulltext">https://www.thelancet.com/journals/... 11/n
Combination therapy with a LABA/LAMA has a greater effect on patient reported outcomes than mono therapy with either class of drug. The latest @NICEComms guidelines 2019 recommend combination therapy for anyone with #COPD & optimised non-pharmacological therapy 12/n
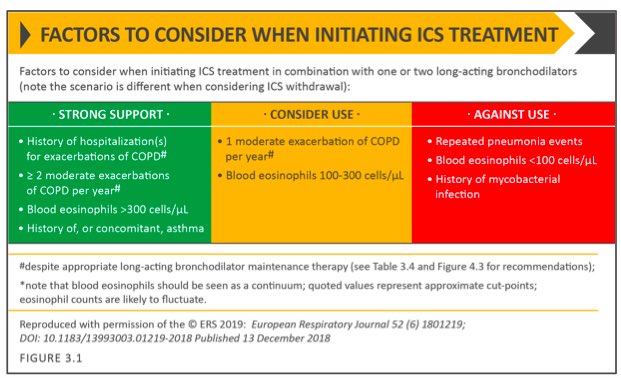
So what is the place of ICS in the treatment of stable #COPD? There is no evidence of mortality benefit or reduced FEV1 decline for ICS alone. However, in patients with moderate to very severe COPD & exacerbations, an ICS/ LABA is more effective than either component alone 13/n
LABA/ICS improves lung function, health status, & reduces exacerbation in mod-v severe #COPD. Combination therapy has not been shown to have a statistically significant impact on all cause mortality. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD006829.pub2/abstract">https://www.cochranelibrary.com/cdsr/doi/... 14/n
Blood eosinophil count predicts ICS response in preventing future exac. ICS containing regimes have little or no effect at a blood eosinophil count of <100 cells/microlitre. The greatest benefit is in those with count of >300. https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(18)30006-7/fulltext">https://www.thelancet.com/journals/... @LancetResp 15/n
COPD is a diverse & heterogenous collection of conditions. Eosinophil count is one ‘treatable trait’ that can be used to form a personalised management plan for an individual patient. https://erj.ersjournals.com/content/47/2/410">https://erj.ersjournals.com/content/4... 16/n
The use of biomarkers to predict outcome, & treatable traits which can be treated to modify those outcomes is an area of active research in #COPD & other respiratoey conditions https://erj.ersjournals.com/content/53/5/1802058.full">https://erj.ersjournals.com/content/5... 17/n
The treatment effect of ICS containing regimes is higher in patients with a higher exacerbation rate (>2 exacerbations, or 1 hospitalisation in the previous year) - shown in this post hoc analysis of 3 RCTs 17/n https://www.sciencedirect.com/science/article/abs/pii/S2213260018300067">https://www.sciencedirect.com/science/a...
The potential benefits of ICS must be weighed against risks. ICS use is assoc with higher prevalence of oral candidiasis, hoarse voice & skin bruising. Of more concern is a higher risk of pneumonia - present even at lower doses of fluticasone furoate 18/n https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(13)70040-7/fulltext">https://www.thelancet.com/journals/...
This from @GOLD_COPD is a helpful summary of considerations when deciding whether to prescribe an #ICS for a patient with #COPD 19/n
What about triple therapy? There are now several trials which show that triple therapy improves lung function, & reduces exacerbation. These trials were done in patients with moderate to very severe COPD, who had an least 1 exacerbation in the previous year. 20/n
Excitingly recent papers suggest there may be a mortality benefit to triple therapy in patients at the more severe end of the spectrum, although these trials did not have mortality as their predefined primary outcome @NEJM. https://www.nejm.org/doi/full/10.1056/NEJMoa1916046">https://www.nejm.org/doi/full/... 21/n
So, current evidence favours a combination LABA/LAMA for this patient with #COPD who has stopped smoking & completed PR but remains breathless, has no evidence of asthma, low eosinophils, & a low exacerbation rate in the last year. 22/n
If you can’t get enough of #COPD we recommend the @NICEComms 2019 guidance: https://www.guidelines.co.uk/respiratory/nice-copd-guideline/454912.article">https://www.guidelines.co.uk/respirato... 23/n
And also the @GOLD_COPD 2020 guidelines: https://goldcopd.org/gold-reports/ ">https://goldcopd.org/gold-repo... 24/n
And the South East London #COPD management guidelines, collaboratively produced by primary & secondary care & which we think are excellent! https://www.lambethccg.nhs.uk/news-and-publications/meeting-papers/south-east-london-area-prescribing-committee/Documents/Clinical%20guidelines%20and%20pathways/SEL%20COPD%20guideline%20Apr%202019.pdf">https://www.lambethccg.nhs.uk/news-and-... 25/n
Ok that’s it this week. Hope you enjoyed this dive into inhaled treatments for #COPD. See you next week for more #RespEd on #MCQMonday. Pls share with any budding #phlegmfriends you know! #RespisBest #loveyourlungs 26/26

 Read on Twitter
Read on Twitter