The #agedcareRC has begin its hearing this morning into impact of Covid-19 on the sector. Peter Rozen QC is delivering opening remarks. Says there is nothing surprising about the horror headlines.
"In light of those deficiencies, it is hardly surprising that the aged care
sector has struggled to respond to COVID-19... the de-skilling of the aged care workforce was identified as a likely consequence of the lack of regulation of staffing in aged care," Rozen says.
sector has struggled to respond to COVID-19... the de-skilling of the aged care workforce was identified as a likely consequence of the lack of regulation of staffing in aged care," Rozen says.
"The consequences of a shortage of clinical skills in aged care homes for care quality and resident safety have been demonstrated time and again in the case studies this Royal Commission has examined."
"[cases have shown] consequences of a system in which providers have the ultimate say concerning the numbers and skill mix of their workforce and can chose between paying the hourly rate of a university-educated nurse and that of a care worker with or without a Certificate III."
Rozen quotes Hunt who said in late July: "aged care around the country has been immensely prepared." The Royal Commission disagrees. "The evidence will demonstrate that the sector has been underprepared." Surprise!
"There was undoubtedly a great deal done to prepare the Aust health sector more generally for the pandemic, the evidence will reveal that neither the Commonwealth Department of Health nor the aged care regulator developed a COVID-19 plan specifically for the aged care sector."
Now, much of this hearing will focus on lessons that were (or should have) been learned from Covid-19 outbreaks in Sydney at Dorothy Henderson Lodge and Newmarch House.
"It may come as a surprise to some that the aged care regulator has not investigated the circumstances of the Dorothy Henderson Lodge and Newmarch House outbreaks. Incident investigations are normally one of the key tasks of any regulator for obvious reasons."
Crucially, Rozen draws attention to the "notorious" issues regarding interface between state and territory health systems and fed govt aged care system. "These... were always going to be brought into stark relief by an outbreak of COVID-19 in the residential aged care sector."
Anglicare CEO said "there has been a frustrating level of dysfunction in the collaboration between Newmarch House/Anglicare management and the numerous got departments, agencies and hospital employees at both Federal and State level."
Strong words. "Once again, some families have been unable to ascertain even whether their loved ones are alive or dead. That this can happen in Australia in 2020 is unacceptable; that it is happening again so soon after Newmarch House is unforgiveable."
Oh wow, so regarding Newmarch House the aged care watchdog was "‘strongly recommending that infected residents be removed from the site." Despite this happening at Dorothy Henderson Lodge, the NSW Dept of Health did not want to do this and "set a precedent." #agedcareRC
Commissioner Janet Anderson was incensed by this. "If there is a view
sitting behind the NSW Health position that aged care residents
with COVID-19 should always be cared for in situ and should not
be transferred to a hospital in any circumstances..."
sitting behind the NSW Health position that aged care residents
with COVID-19 should always be cared for in situ and should not
be transferred to a hospital in any circumstances..."
"...then WE MUST
CALL THIS OUT as an intolerable and unsupportable assumption." Capital letters used by Anderson in email to Department of Health on 16 April.
CALL THIS OUT as an intolerable and unsupportable assumption." Capital letters used by Anderson in email to Department of Health on 16 April.
You& #39;ll recall this has also been one of the key issues in the Victorian outbreaks about whether aged care residents should have been moved to hospital at the first sign of an infection.
"The evidence of [Anglicare& #39;s] Miller will be that this stand-off between
officials was so concerning that he spoke to the federal Aged Care
Minister, Senator Colbeck about it. He was subsequently told by the
Minister’s department to follow the NSW Health Department’s advice."
officials was so concerning that he spoke to the federal Aged Care
Minister, Senator Colbeck about it. He was subsequently told by the
Minister’s department to follow the NSW Health Department’s advice."
The result? "According to Mr Millard, of the 37 residents who tested positive
to COVID-19 at Newmarch House, only two were transferred to hospital. 48 One of those died. The other 16 residents who died of COVID-19 were all treated at Newmarch House." #agedcareRC
to COVID-19 at Newmarch House, only two were transferred to hospital. 48 One of those died. The other 16 residents who died of COVID-19 were all treated at Newmarch House." #agedcareRC
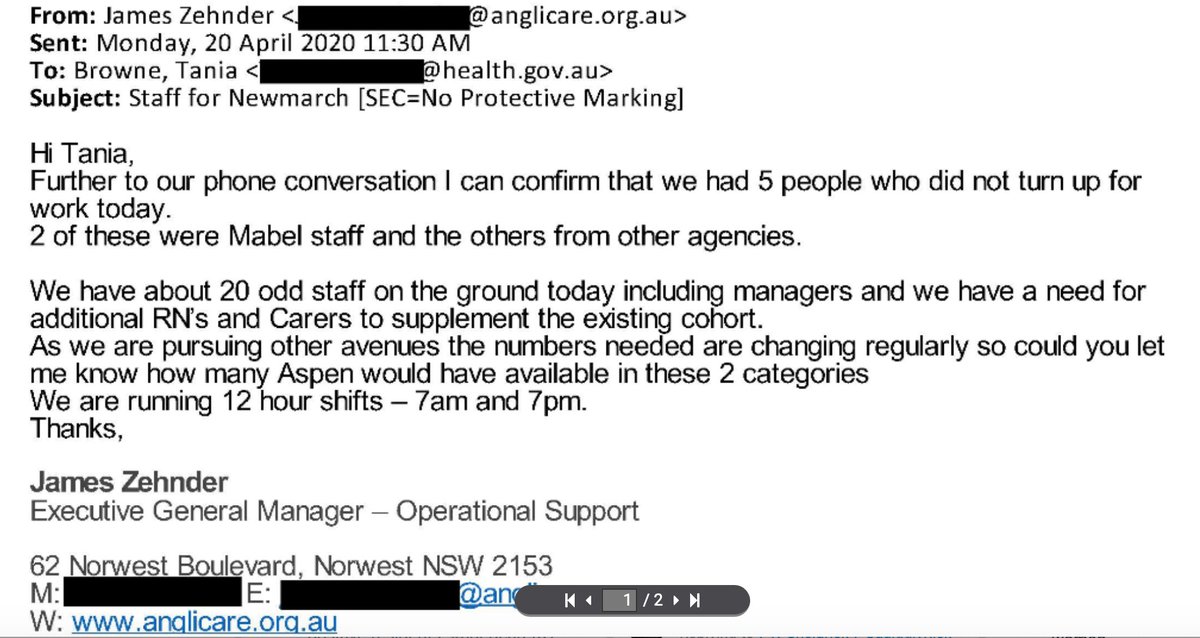
Newmarch planned to lose 30 to 40% of its staff in the event of an outbreak. Anglicare& #39;s Miller now says this was "a massive underestimate" and "totally unrealistic." Dorothy Henderson Lodge lost its entire workforce within 48 hours. Now, how did they get temp staff?
"Interestingly Commissioners, the way they attracted agency staff to work at Dorothy Henderson Lodge was to offer them acute sector pay rates and other improved working conditions. Perhaps the solution to the workforce crisis in aged care is not that complex after all?" - Rozen
"Mr Millard’s... was very impressed with the Aspen employees [but] it became quickly apparent to him that the Mable workers did not have the skills and qualifications that were needed in the particular circumstances." I covered this late May: https://www.thesaturdaypaper.com.au/news/politics/2020/05/23/exclusive-govs-58m-aged-care-app-offers-no-duty-care/15901560009868">https://www.thesaturdaypaper.com.au/news/poli...
"The risks of aged care workers inadvertently introducing COVID-19 into their workplaces had been clear since the Dorothy Henderson Lodge outbreak in March." And that pretty much concludes opening remarks. Witnesses next.
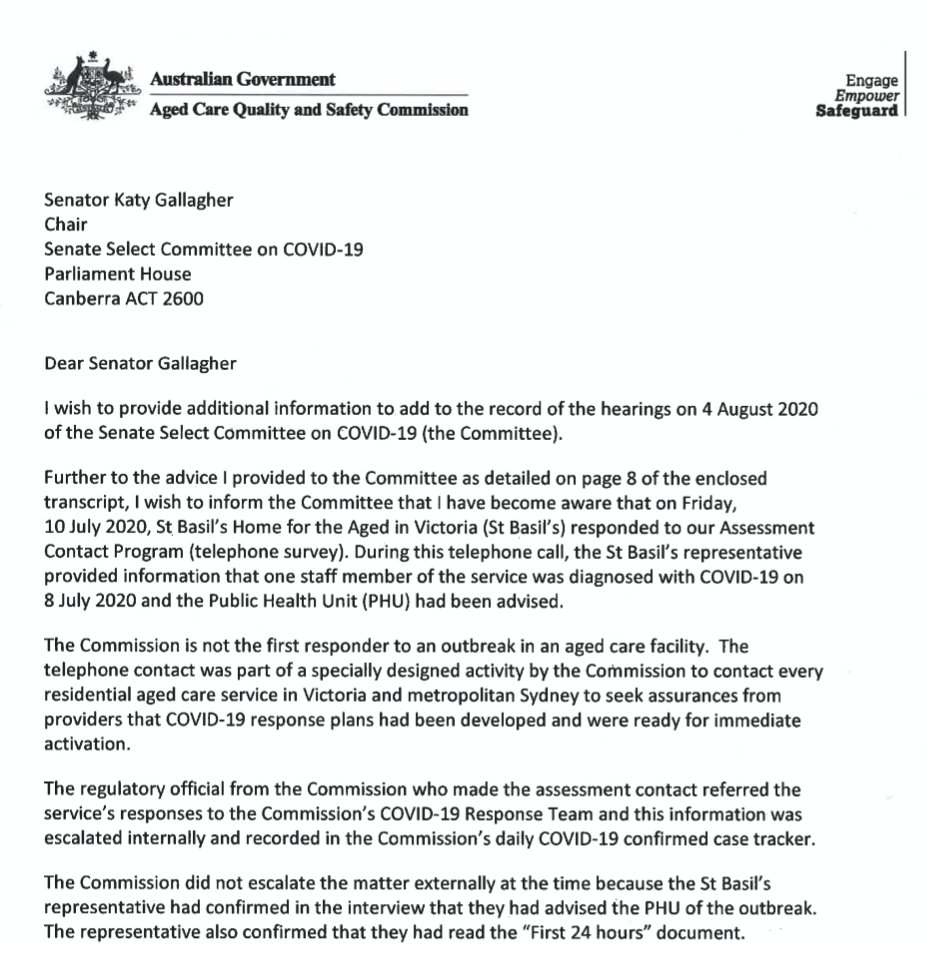
This is interesting. Aged care regulator Janet Anderson told parli inquiry last week that the watchdog was not aware of Covid-19 outbreak at St Basil& #39;s in Fawkner until July 14. Not true. They knew on July 10. She has clarified in a letter to committee chair.
UNSW epidemiologist and WHO pandemic adviser Prof. Mary-Louise McLaws has been telling the #agedcareRC that good airflow is critical to managing outbreaks. Hospitals need 40-80 litres per second per patient. Some aged care home are "less than 3 litres per second per resident."
Recap so far: The Commonwealth had no Covid-19 plan for aged care; crisis was inevitable given state of staffing and skills; NSW Health refused to put infected residents in hospital; Aged Care Minister Colbeck was warned and did not intervene; the same then happened in Vic.
Counsel Assisting the #agedcareRC Peter Rozen QC says: "We will be asking if greater attention to preparation may have saved lives and could save lives in the future." That& #39;s it, really, isn& #39;t it? That& #39;s the question. I suspect they know the answer.
South Australia has had a policy of ~immediately~ transferring any infected aged care resident straight to hospital. The state& #39;s Chief Health Officer Professor Spurrier says this is because they read the evidence on training, expertise etc.
"So we felt that it was, if we had a resident in an aged care facility, that it
would be very quickly that that would spread to not only other residents
but also other workers in that facility." SA is the only state that has such a policy.
would be very quickly that that would spread to not only other residents
but also other workers in that facility." SA is the only state that has such a policy.
Masks were made compulsory for aged care workers on July 13. Prof. McLaws is asked if that should have been done sooner. "Absolutely," she says.
"Masks were universally required in Victoria in the beginning of July. So I am not sure why the residential aged care facilities were considered any different to hospitals." That is an age old question in this space.
I should note here, if you& #39;re someone who knows more about these issues I& #39;m working on a piece this week. I& #39;d be very keen to hear more about the policy / preparedness dysfunction. rickm@thesaturdaypaper.com.au
Just going back over this afternoon& #39;s evidence. The #agedcareRC has heard from Merle Mitchell, a resident at a Victorian facility in Glen Waverley. It& #39;s heartbreaking. "I know I& #39;m here until I die so every morning when I wake up I think damn I& #39;ve woken up."
"But I& #39;m here until I die, so I do the best that I can, which is not to say I& #39;m not being cared for but I am sure if you
asked most people here they would all say they would rather be dead, rather than living here, if they& #39;re honest," she says. #agedcareRC
asked most people here they would all say they would rather be dead, rather than living here, if they& #39;re honest," she says. #agedcareRC
It& #39;s the little things. She hasn& #39;t had a haircut since February. Nor any human contact with her family, except for on the other side of glass initially and then through a window.
"I was lucky enough to have a birthday a couple of weeks ago and I saw her [my daughter] then and that was only through an open window that was two inches open," Merle Mitchell says. Her daughter was "outside in the cold." #agedcareRC
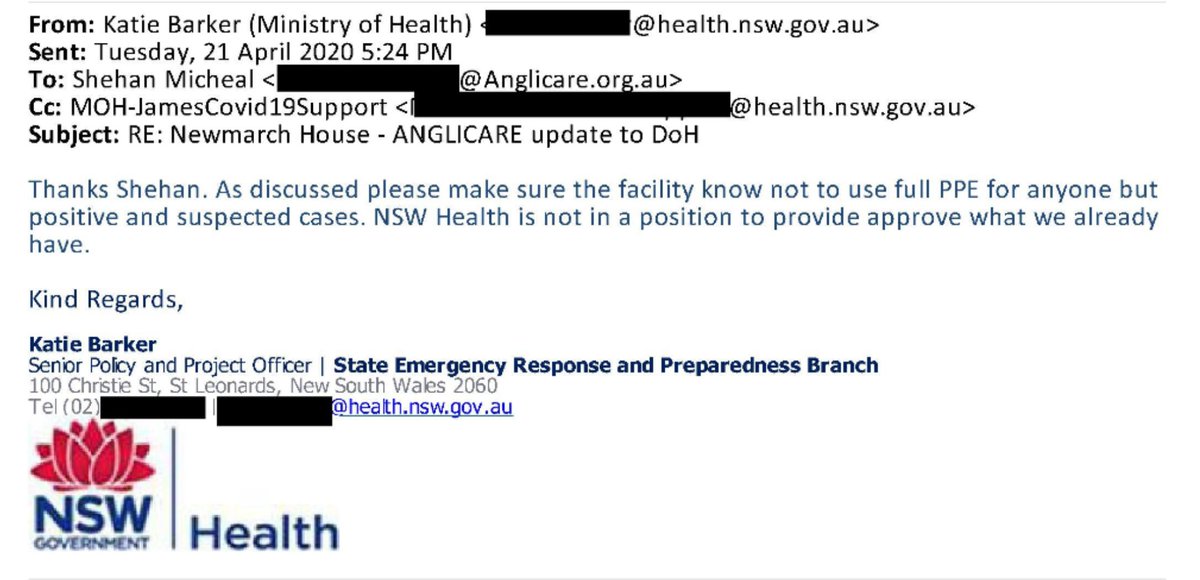
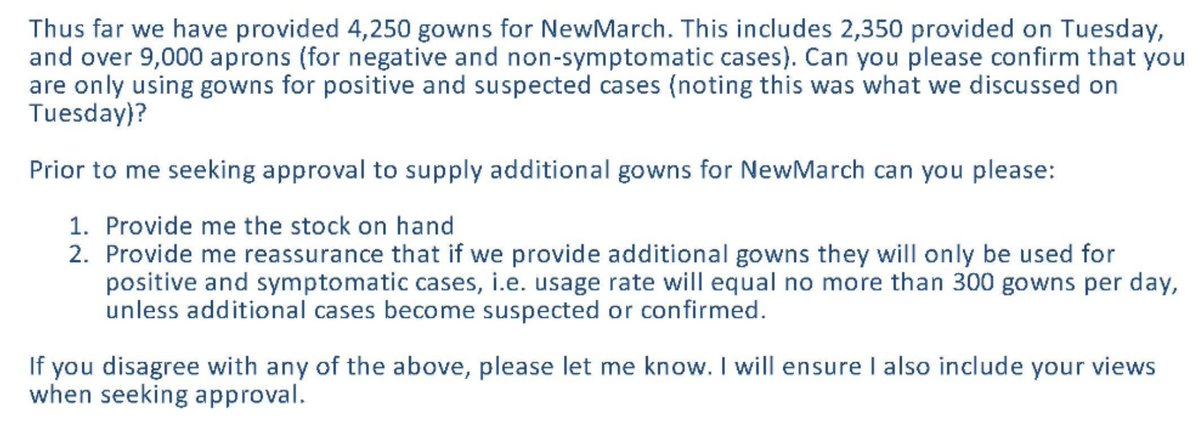
Alright, so Day 2 of the #agedcareRC is kicking off soon. More details on Newmarch. This is damning. On April 21, Anglicare had 25 Covid-19 positive residents. They advised NSW Health they are using full PPE for all 95 residents. The state govt tells them not to. In writing.
More from the same NSW Health staffer a few days later. Seeking "reassurance" that if they hand over more gowns they will only be used on positive residents. #agedcareRC
In the middle of the crisis, staff just didn& #39;t come to work at Newmarch. Including from Mable, the private company with "no duty of care" that was paid $1.6m in a limited tender by Commonwealth to support aged care in outbreaks.
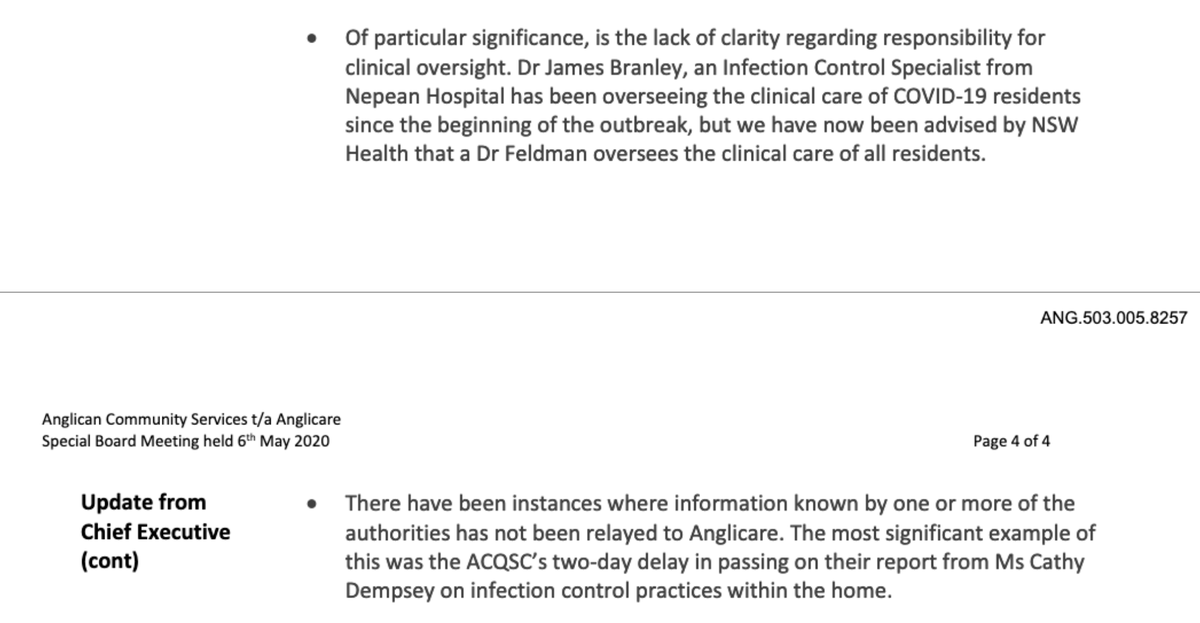
This is an update from Anglicare CEO Grant Millard on May 6 to a special board meeting regarding situation at Newmarch House.
Counsel assisting Paul Bolster is currently interviewing Virgina Clarke at the #agedcareRC. Her father was in relatively good health, in the low care wing of Newmarch House. He died after being infected with Covid-19. At first, Ms Clarke wasn& #39;t told he had tested positive.
Bolster: "Did anything in your conversation with (your Dad) on the Saturday, when you talked to him about the advanced care planning did anything in the conversation suggest to you that he knew that he had COVID-19?"
Ms Clarke: "No."
Ms Clarke: "No."
Clarke: "I asked the staff member one time when (I) finally got on to somebody I said & #39;Does dad know that he has COVID-19? Does he know that the test result came back positive?& #39; And they said & #39;Look, we can& #39;t answer that.& #39; She said & #39;I don& #39;t know& #39;."
Her father died on the Sunday, just three days later. It was difficult to sign off his death certificate as his usual doctor couldn& #39;t see the body. He had 7 children, more grandchildren and great grandchildren. Only 10 people could go to his funeral.
"They said once dad had passed away, we could... no longer have any further contact with Newmarch House," Virginia Clarke says. She never got the answers she sought.
Next up on the witness stand we are hearing from Anglicare CEO Grant Millard (they run Newmarch House)and Erica Roy, general manager residential care services for the non-profit provider. #agedcarerc
Ms Roy is a Registered Nurse, a member of Anglicare& #39;s Crisis Management Team and in charge of the team that manages clinical governance for the aged care provider. Just establishing her chops before we get into the evidence.
Peter Rozen QC is now asking Anglicare CEO Grant Millard about the process before the Covid-19 outbreak when the aged care regulator asked providers to do a "self-assessment" of their preparedness ahead of a potential outbreak. We all know how good self-assessments are!
It will surprise no one, I suppose, that Newmarch House answered "yes" to every question about Covid-19 preparedness from the Aged Care Quality and Safety Commission. Questions included "Does the service have an infection control respiratory
outbreak plan?" for example.
outbreak plan?" for example.
Ms Roy concedes many elements of Newmarch& #39;s response to regulator were "inaccurate" and with hindsight they treated Covid-19 as a "flu-like" illness rather than a virulent infection. That said, why was the regulator so naive as to think any provider assessment would be realistic?
Now, on the issue of transferring residents to hospital. Millard, Anglicare CEO: "There was one of the conference calls on the 16 April where there was a heated interaction or robust discussion about cohorting strategies, decanting either positives or negatives."
In late May, Millard told the Anglicare board: "In the event of infection at another home Anglicare would be far
more... would strongly push for these residents to be immediately transferred to hospital."
more... would strongly push for these residents to be immediately transferred to hospital."
Looking back, he says, managing an outbreak like Newmarch was a "monumental challenge."
"My comments were more related to the concern about the risk of infection to other residents in the home," Millard says.
"My comments were more related to the concern about the risk of infection to other residents in the home," Millard says.
Millard is now shown a NSW Health document about so-called "Hospital in the home" which says as a matter of policy any such arrangement in aged care must be done by written agreement. Has Millard ever seen such an agreement?
"No."
"No."
"I& #39;m not aware of any written agreement. I certainly have never seen one and the inquiries we have made, none was executed, no," Millard says. Such an agreement would have included clear definition of roles and responsibilities between Health and Aged Care.
Oh wow, so we are about to hear evidence from Nepean Hospital physician Dr Branley that NSW Health had ~already~ decided its policy would be to treat Covid-19 aged care residents "in their home." This decision was made well before the Newmarch outbreak.
"To run a hospital you need substantially more, a greater number of nurses to do that. It& #39;s just not the way a
residential aged care home operates," Millard says. Even so, at the peak of the outbreak documents show Newmarch had a "five-fold" increase in rostered nurses.
residential aged care home operates," Millard says. Even so, at the peak of the outbreak documents show Newmarch had a "five-fold" increase in rostered nurses.
"I think if you compare the level of equipment, the resourcing, you know, it& #39;s not reasonable to anticipate any of that level of equipment resourcing would be available in a residential aged care home. That would have to occur in a hospital," Millard says.
Commissioner Lynelle Briggs asks: "[Do you] think that NSW Health had made assumptions that you would be able to resource Newmarch House at the same level as a hospital, or were they simply unfamiliar with the aged care system?"
Millard: "I think that& #39;s really a question for state health to ponder... but I think it& #39;s generally understood the significant resourcing difference that& #39;s provided for an average bed day in a hospital as opposed to a residential aged care setting." Adjourned for a break now.
OK, we are getting important context on the NSW Department& #39;s refusal to hand over full protective equipment for use with all residents at Newmarch. Dr Branley, an infectious diseases specialist, had ~directed~ staff at Newmarch to use full PPE on ~all~ residents.
Dr Branley is a specialist at Nepean Hospital. In other words, an expert. But the bureaucrats in Department of Health directly contradicted his advice.
Millard: "It was deeply distressing based on the advice of the expert we had from Dr Branley about you really need to treat all of your residents as COVID positive until it& #39;s proven otherwise through multiple rounds of testing over a designated period."
Millard: "Many of the residents were
still incubating and in fact inadequate supply of PPE up-front meant that many of our staff in the initial stages were either affected or listed as
close contacts bc they weren& #39;t supplied, they didn& #39;t have adequate PPE in the early stages."
still incubating and in fact inadequate supply of PPE up-front meant that many of our staff in the initial stages were either affected or listed as
close contacts bc they weren& #39;t supplied, they didn& #39;t have adequate PPE in the early stages."
"Well, we had estimated in our, what we thought was conservative provisioning putting together a surge workforce of 30 to 40 people. Within a number of days we lost, we calculated 87 per cent of our workforce," Millard says.
Now we are talking about Mable, the ~only~ surge workforce provider funded by the Commonwealth at the start of the outbreak. Private company, run by financiers and investors. "Early on they just weren& #39;t up to the task," Millard says. "It was dangerous for them (the staff)."
"It wasn& #39;t as if they had a magic quarantine number of workers. We were all scratching around and people were scared. They were terrified of COVID and it was difficult to get people," Millard says.
Anglicare CEO Grant Millard is apologising to families for the lack of communication during the crisis. This comes across very genuine. It was a traumatic time for everyone, he says. "We were absolutely overwhelmed with
the challenges of dealing with with COVID-19."
the challenges of dealing with with COVID-19."
The more we learn about the Newmarch House outbreak, the harder it is to ignore the feeling that perhaps they particularly were let down by a litany of public agencies who had NFI what they were meant to be doing. Second outbreak but the most singularly devastating one then.
Quick pivot to Victoria, Dan Andrews says state health nurses have covered 1148 aged care shifts in the federal govt run sector. That is an enormous number.
Back at #agedcareRC we are now hearing from Kathleen (Kath) Dempsey, senior manager of the Healthcare Associated Infection program at the NSW Clinical Excellence Commission and Dr James Branley, the specialist physician seconded to Newmarch from Nepean Hospital during outbreak.
Dr Branley, who is also a clinical microbiologist, was part of an AUSMAT team that was sent to Wuhan, China during the initial stages of the Covid-19 outbreak in that country. He helped with evacuation of Australian citizens to Christmas Island.
Dempsey says re: aged care: "It& #39;s a balance between infection control and providing a homely and inviting environment and often the two don& #39;t match when things are going wrong." She has worked with resi aged care in the past on other infections (flu, gastro etc)
On May 1, her first day on site at Newmarch, Dempsey noted there was "a visible presence in the facility in operational management, however a lack of infection prevention and control expertise." Documents tendered to #agedcareRC show her report was given to the regulator but:
Key part of last tweet is that aged care watchdog sat on the report for two days, in the middle of an outbreak, and didn& #39;t inform Newmarch House. One would have thought it was urgent. Recall the watchdog was also told of outbreak at St Basil& #39;s in Vic 4 days before it said it had.
We are starting to see a pattern emerging here for the Aged Care Quality and Safety Commission (the federal regulator) either not acting fast enough or incapable of acting fast enough with critical information in the middle of a pandemic. And before, for that matter.
Now, back on issue of transferring to hospital or not. Dr Branley says the word & #39;policy& #39; is "perhaps a little too elaborate a title" for what was essentially a working arrangement in the Nepean health district. That arrangement was to do & #39;hospital in the home& #39; for +ve residents.
Rozen QC is showing Dr Branley a NSW Health policy document about hospital in the home. The eligibility criteria clearly state: "A patient must meet the
criteria for hospital admission under the New South Wales Health admission policy." Rozen is clever.
criteria for hospital admission under the New South Wales Health admission policy." Rozen is clever.
Rozen: "Is your evidence that all of the
patients that were treated at Newmarch House under this policy satisfied the first of those criteria, that they met the criteria for hospital admission under the New South Wales Health admission policy?" Dr Branley fudges.
patients that were treated at Newmarch House under this policy satisfied the first of those criteria, that they met the criteria for hospital admission under the New South Wales Health admission policy?" Dr Branley fudges.
Counsel for NSW Health objects to Mr Rozen& #39;s use of the term & #39;policy& #39;.
"That document is a guideline," the state& #39;s counsel Michael Fordham says.
"That document is a guideline," the state& #39;s counsel Michael Fordham says.
Rozen appears to be angling for a concession that refusal to transfer +ve Covid-19 residents to an actual hospital was done as a blanket & #39;policy& #39; w/o any regard to individual circumstances of each resident. Dr Branley says in an ideal world it would have been discussed w/ them
To be clear, hospital in home requires: written agreement with aged care facility, training provided to their staff, support provided to them, development of business rules for communication. Rozen then asks: "None of these steps were implemented at Newmarch House, were they?"
Dr Branley refers to "the volume of residents" but is cut off by Rozen who insists "it& #39;s a very simple question."
"None of these conditions were satisfied at Newmarch House, were they?"
Dr Branley: "Those conditions were applied as best we could."
"None of these conditions were satisfied at Newmarch House, were they?"
Dr Branley: "Those conditions were applied as best we could."
Dr Branley says what the commonwealth ought to have known at the beginning: "We know that internationally residential aged care facilities and hospitals have acted as the big amplifier and spreader of the virus throughout society."
Dr Branley comes at this from a different view, however. He says moving residents to hospitals "poses a really significant health issue, and it& #39;s a public health issue." It sounds awfully like residents at Newmarch were penned in to protect the wider hospital system.
Aged Care Minister Richard Colbeck says the nation has had a plan for Covid-19 in residential aged care "going right back to the beginnings of our preparations." I guess that is the definition of & #39;beginning& #39;.
tl;dr when did you have a plan? At the start of the plan.
Colbeck is absolutely not across the detail of the St Basil& #39;s outbreak. He says commonwealth was only "officially" told on the 14th of July. He then concedes the aged care watchdog found out on July 10. "The information that was gleaned wasn& #39;t passed on to anyone else," he says.
Colbeck says he has seen a "significant utilisation of the learnings" which is about as clear as porridge.
I& #39;m just catching up on the afternoon& #39;s evidence at the #agedcarerc and they had some GOOD examples of services that prepared for Covid-19. HammondCare was one, and Opal were brought in to give their view of how things unfolded.
Stephen Judd, the outgoing CEO of HammondCare, told the Commission about one aged care worker whose car broke down. She "knew the roster was really, really tight" and had a palliative client. So she ~walked~ 7 or 8 kilometres to actually care for that client.
In case it needs to be said: In most cases in aged care, incredibly lowly paid staff are fighting a terrific battle against the odds. The system around them, broken and dramatically underfunded for DECADES, has led to this. Not them.
Now this is interesting. Newmarch had its first case April 11. You& #39;ll recall only two residents there were taken to hospital. More than 30 with Covid-19 were not. But weeks earlier, Opal Bankstown had its first case on March 23. Another on March 25. And then a third April 8.
All three residents were taken to hospital. Opal Bankstown never had another positive Covid-19 case in its facility. This was a success story in difficult times. Then Newmarch happened, residents were forced to stay put as a matter of "guidelines." 19 residents died.
Opal Bankstown told the royal commission that at NO point was this so-called & #39;hospital in the home& #39; drive mentioned to them. Their residents needed hospital care and they got it. But not those at Newmarch just days later. What changed?
Opal& #39;s regional general manager Jonathan Anderson told the #agedcareRC that they relied on clinical expert advice but in the end it was Opal making decisions they thought were best for the residents. Not the state govt, not the commonwealth, not anyone else.
Judd at HammondCare agreed. Judd at HammondCare agrees. "We made a decision very early on, similar to what Mr Anderson has said that we weren& #39;t going to cede control, if you like, to other agencies." It reads very much like these providers did not trust them to get it right.
Raguz, director of clinical services at HammondCare, said they made decisions because they had responsibility to everyone. Not just Covid-19 positive residents but those in the facilities who were not.
"We still have other people who are residents within aged care who may be negative and they& #39;re not part of the health system. So the decision-making should sit with the provider in order to look at our overall cohort of people that we provide care for," Raguz says.
Still catching up on yesterday& #39;s #agedcareRC hearing before today& #39;s gets underway. The evidence from Angela Raguz, an RN and clinical gov team manager at HammondCare, is heartbreaking. This next quote has ruined me.
"People who do not see their loved ones are at higher risk of not just mental wellbeing suffering but also physical. I think underestimating the physical impact on people of not seeing people who they love is– that’s a mistake."
Psychologist Julie Kelly, embedded in one aged care facility: "For a lot of the residents, there’s a real, real strong sense of hopelessness, of not knowing when this is going to end or being able to see any changes for them."
Gerontological physiotherapist Rik Dawson says elderly people are literally wasting away in nursing homes throughout Covid-19 lockdown. "There’s probably 25 to 35 per cent of residents in nursing homes that have no access, or very limited access, to physio," he told #agedcareRC
Wow. Royal Commission was showed data by Dawson from one hospital in one state (Fiona Stanley Hospital, WA, which counsel argues is possibly the least affected state by Covid-19). The rate of falls in 75+ almost doubled in June compared to same month last year.
Alright, day 3 #agedcareRC hearing. I am juggling a few stories and commitments today but will try to keep up. First up is Professor Joseph Ibrahim, an expert in geriatric medicine of 30 years& #39; standing, public health credentials. He& #39;s top line.
"This is the worst disaster that is still
unfolding before my eyes and it& #39;s the worst in my entire career," Prof. Ibrahim says. "I didn& #39;t think we would sink any lower following the Royal Commission
findings from last year and yet we have."
unfolding before my eyes and it& #39;s the worst in my entire career," Prof. Ibrahim says. "I didn& #39;t think we would sink any lower following the Royal Commission
findings from last year and yet we have."
He continues: "In my opinion, hundreds of residents are, and will, die prematurely because people have failed to act. There& #39;s a lack of empathy, a lack of urgency. There& #39;s an attitude of futility which leads to an absence of action."
This is the key line and, of course, he is right. "What I wanted to stress is
all of this was foreseeable. I& #39;m not presenting anything looking back with hindsight or being smart after the fact."
all of this was foreseeable. I& #39;m not presenting anything looking back with hindsight or being smart after the fact."
Professor Ibrahim notes that Australia is now the second or third worst performing nation in the world on aged care deaths. Canada is the worst, with a death rate in care of 80 per cent.
According to his back-of-the-envelope calculation in Victoria, aged care homes were a 30-times GREATER risk of an outbreak than any other household in the state. The preparation for that, he says, never matched the extreme high risk.
Prof. Ibrahim says very few people understand what it is actually like to work in aged care. "The doctors come and go. In a hospital, the doctors are there 24/7. The nurses are there 24/7. That& #39;s not the situation in aged care."
Counsel assisting Peter Rozen shows Professor Ibrahim the health system response document the fed govt claims is an aged care plan. Is it?
Prof. Ibrahim says it isn& #39;t. "I think any person reading it would see that it doesn& #39;t do that [propose a response]."
Prof. Ibrahim says it isn& #39;t. "I think any person reading it would see that it doesn& #39;t do that [propose a response]."
"It doesn& #39;t reference that there are
existing failures in workforce, in infection control, in governance, in the
capability of individual providers. That& #39;s nowhere to be seen. All of
those factors would be essential," Prof. Ibrahim says.
existing failures in workforce, in infection control, in governance, in the
capability of individual providers. That& #39;s nowhere to be seen. All of
those factors would be essential," Prof. Ibrahim says.
Prof. Ibrahim says this isn& #39;t complex scientific modelling. "This is the sort of plain management you would teach to an undergraduate."
Now Rozen is showing the Communicable Diseases Network Australia (CDNA) guidelines which he says provides a "comprehensive list of instructions." Prof. Ibrahim says, again, this is a document for one facility. It& #39;s not a plan for the aged care sector.
"And so some poor bugger sitting
in an aged care home, a middle manager... tell us how you would find 20% of your workforce and you are probably already short staffed. But there& #39;s no offer of solutions. There& #39;s no offer of where info could come from or what others have done."
in an aged care home, a middle manager... tell us how you would find 20% of your workforce and you are probably already short staffed. But there& #39;s no offer of solutions. There& #39;s no offer of where info could come from or what others have done."
Morrison announced new measures on Friday. Prof. Ibrahim says "all of those announcements... could
have been made back in Feb or March. There& #39;s nothing in them that you would say we& #39;ve now learnt over the last six months and we now need to act. There& #39;s nothing novel in them."
have been made back in Feb or March. There& #39;s nothing in them that you would say we& #39;ve now learnt over the last six months and we now need to act. There& #39;s nothing novel in them."
Prof. Ibrahim is asked about the Aged Care Quality and Safety Commission. They are the federal regulator. I often just call them the watchdog because its easier. "The Commission knew prior to the pandemic that there were problems with infection control and with clinical care."
"They would know which facilities have a high risk of non-compliance in the past and should have been targeting that group in terms of pandemic response. They should have been actively reviewing the pandemic plans." But even so, they don& #39;t have the skills for that, he says.
Next witness will be very interesting. Dr Nigel Lyons, a deputy secretary with the NSW Ministry of Health.
Dr Lyons has been ~intimately~ involved in many of the discussions around moving positive Covid-19 aged care residents into hospitals.
OK, Dr Lyons is being asked about the notes made during a meeting with others including C& #39;wlth Department of Health rep where it is made clear NSW preference is not to move sick residents into hospitals due to "the precedent this would set."
He says there was certainly a discussion about "decanting" the residents but the difficulty was knowing who to take out, given some may be positive but not showing it yet. Counsel assisting Peter Rozen QC picks up on this.
"That& #39;s the point, though, isn& #39;t it, if you wait until everyone who is going to be tested tests positive, you potentially lose control of the outbreak in the facility, don& #39;t you?"
Quick pivot to Victoria. Dan Andrews says 406 aged care residents in the state have been transferred to hospital “the majority of them are positive for Covid-19.” Bear in mind this was not something that was done at the start of the outbreaks there.
Actually I might have misheard that number. It’s higher but not 500. Will have to go back and check.
Back to #agedcareRC and Counsel assisting Peter Rozen QC asks Dr Lyons if anyone from NSW Health at any time expressed concern that removing residents from Newmarch House would set a course for how any outbreak in the future would be handled.
"I can& #39;t recall those words being used in that way but I would say any action taken at any point in time can be then used as a basis for assessing future actions," Dr Lyons says. Which, in inquiry speak is: yes, but I don& #39;t want to say that.
Dr Lyons is now being grilled about the controversial & #39;hospital in the home& #39; model that was implemented at Newmarch House. The NSW Health guidelines state there should be written agreement, staff should be trained and supported. But Newmarch had lost almost all its original staff
"I suggest, doctor, that for hospital-in-the-home to work in the residential aged care facility in response to the COVID-19 pandemic, you have to have everything in place: the agreement, the training, the facilities, to have any chance of succeeding," Rozen says.
Dr Lyons says: "Certainly it would be an advantage to have it in advance."
Rozen quips: "Yes, like having the plan in advance, isn& #39;t it?"
Dr Lyons: "That& #39;s correct."
Rozen quips: "Yes, like having the plan in advance, isn& #39;t it?"
Dr Lyons: "That& #39;s correct."
By way of closing, Dr Lyons says they met twice a week to discuss ongoing review of clinical options at Newmarch. "We even talked about, other aged care providers taking some residents. We talked about options around private hospitals taking some of the residents."
Adjourned for a short break. Might eat some breakfast!
Ha ha just kidding. I’m having a smoke. At some point today I’ve got to try and write my second story for this weekend’s @SatPaper while also plugging in for the afternoon session. But things might get a bit patchy.
Commission back with a panel of union leaders including the indefatigable @AbutlerAnnie, Carolyn Smith and Diana Asmar.
Ms Asmar, branch secretary in Vic for the Health Services Union, says she believes about 1000 of the union& #39;s members have tested positive for Covid-19. These are mostly cleaners and personal care workers. They have been calling facilities and compiling their own data.
Annie Butler from the AMNF says her members are experiencing horrors previously unknown. "I would call it trauma," she says.
"And some of our nurses are reporting, registered nurses who are coming from the public health sector to support staffing in residential aged care facilities and some of the things that they& #39;re finding, that can only be described as abject neglect," she says.
Annie Butler from the @anmf_federal says they went to Aged Care Minister Richard Colbeck on March 4 and raised the "urgent need" for "increased staffing and training" because of a "critical, critical concern" noticed in aged care globally up to that point.
This is astonishing.
"But I have to say that I understood that we requested a meeting with the Minister from 4 March. We didn& #39;t get a meeting until 4 April despite insistence and despite raising our concerns," Ms Butler says.
"But I have to say that I understood that we requested a meeting with the Minister from 4 March. We didn& #39;t get a meeting until 4 April despite insistence and despite raising our concerns," Ms Butler says.
All three union bosses saying what has been long known in the industry: aged care homes were short staffed well before Covid-19 came on the scene. But the outbreaks made an already bad situation catastrophic.
Ms Butler says there were massive strains around personal protective equipment, getting it delivered via the National Stockpile and then also within aged care facilities.
"We had members tell us they could only use one glove rather than two. We had members told they had to reuse equipment, put it in collective plastic
bags. A whole range of incredible breaches in infection control," she says.
bags. A whole range of incredible breaches in infection control," she says.
Now, did the fed govt have a plan? Well, they had a document, says Annie Butler. "The first (guidelines) that we saw in April didn& #39;t even have the Fed Govt as one of the bodies with responsibility. The Federal Government wasn& #39;t even included. Which is absolutely astonishing."
"And it feels like we wrote something, you know, there was a & #39;plan& #39; written on a piece of paper and then we have ticked the box and that& #39;s it. And that is disgraceful, I think that& #39;s absolutely disgraceful," Carolyn Smith says.
The #agedcareRC has resumed after lunch and it promises to be awkward and blistering. Four government witnesses. Dept of Health& #39;s Michael Lye, aged care watchdog boss Janet Anderson and her report Melanie Wroth and Health secretary Brendon Murphy (recently chief medical officer).
Murphy has already asked to "crave the indulgence" of the commission to "correct" a number of statements made in Peter Rozen QC& #39;s opening address which said the Commonwealth did not have a plan for Covid-19 and aged care. He says they are not accurate.
Commissioner Pagone is surprised. Says this request has "come out of left field." Rozen QC says it would be inappropriate to allow him to make a statement on indulgence. Commission adjourns briefly while they figure out what to do. C& #39;wlth clearly smarting.
This has to be a land speed record for awkwardness. Didn& #39;t think it would come so soon.
Back. Commissioner Pagone says he hopes what he is about to say doesn& #39;t become a story. It is only a procedural matter, he says. It is unusual, he says, to give witnesses a chance to respond to media reports from the box. "It has never been done in the course of this commission."
Professor Murphy has already wasted 10 minutes of time by asking for this very out-of-order request. They are only up as witnesses for an hour or two. Running down the clock.
Interestingly, Prof. Murphy wasn& #39;t meant to be a witness but Commonwealth solicitors sprang into action late on Monday and requested he be included. After Rozen& #39;s opening address. Commission accepted. Asked Prof. Murphy for a precis of his evidence. "None has been forthcoming."
Commissioner Pagone has just told the hearing that a note has been given to him. (What is this, Year 9?) The Commonwealth are asking to make a submission. Oh, it& #39;s Professor Murphy& #39;s signed statement that they are now offering to provide to the #agedcareRC that was never provided
We are watching the Commonwealth, in real time, in major damage control here. "Ms Morgan, I think that is probably
something that you really could have taken offline rather than occupy space of the Commission time," Pagone admonishes C& #39;wlth counsel.
something that you really could have taken offline rather than occupy space of the Commission time," Pagone admonishes C& #39;wlth counsel.
This has been a very weird, amateur-ish TWENTY minutes thanks to Prof. Murphy and bumbling Commonwealth legal counsel.
Oh it& #39;s not over. Professor Murphy is now trying to slip into his answers unrelated information about the "foundational" outbreak plan for residential aged care launched in March. Rozen QC asks him to stick to the topic.
This would be the thing he was itching to talk about in a statement of indulgence at the start of the hearing which was denied to him. I feel like I& #39;m watching a two-year-old knock over a vase in full sight and then claim he didn& #39;t see it.
Rozen QC asks Michael Lye from the Department. "Why is Australia faring so badly?" He is referring here to data that shows 70% of deaths in Oz from coronavirus happened in aged care, making us the 2nd or 3rd worst in the world. Lye says he has no expertise, defers to Murphy.
Please bear in mind that Michael Lye is THE MOST SENIOR Health bureaucrat in charge of the entire aged care sector. He says he is not an expert. Rozen is sharp. "No, I don& #39;t want Professor Murphy to answer the question. Mr Lye, I& #39;m asking you."
Lye says it is "unfair" to calculate the death rate this way. He maintains that "every death is a tragedy" but ultimately "given the nature of the COVID and its preponderance to effect the frail aged is population that where it takes hold, then we necessarily see that result" !!!
Now Rozen is asking about the Communicable Disease Network Australia document which the commonwealth has offered up as an example of its plan for Covid-19 in aged care settings.
The first version of this document was produced on March 13 this year. Version two was released April 30. The current version of this document is dated July 14.
The CDNA has some 24 members. But none of them have any expertise in aged care. None of them is a geriatrician, for example. Rozen asks Lye if he agrees with that. "I do," Lye says. But says they consulted more widely than the core group.
"It& #39;s not actually entitled & #39;plan& #39; is it, it is entitled & #39;guidelines& #39;," Rozen points out to Lye, who accepts. I know where Rozen is heading w/ this. He is pointing out the roles and responsibilities in this guidelines. Nowhere are the Commonwealth mentioned in first two versions
Lye ays he doesn& #39;t have the earlier versions of the document with him so he can& #39;t tell Rozen QC if the Commonwealth was listed as having a role or responsibility. Rozen: "You& #39;re telling me, though, that you don& #39;t know?"
Oh man, in all the fumbling Professor Murphy appeared to lean over and give the answer to Lye. This is schoolyard shit. "Did Professor Murphy just whisper the answer he suggest you give, Mr Lye?"
Professor Murphy& #39;s genius suggestion, by the way, was to whisper to Lye that it was an Australian government document so it would have been implied that the Commonwealth had oversight.
"You think this document would have been checked by the Department (of Health) without anyone noticing that it failed to refer to the Australian Government& #39;s role," Rozen asks Lye. This is very uncomfortable to watch.
The document, purported to be a Commonwealth "plan" for aged care and Covid-19 explicitly says "the department do not warrant or represent that the information contained in the guideline is accurate, current or complete." This is meant to be a plan. It& #39;s a coward& #39;s doc.
Lye says the only reason he could think of for that wording is that even though the Commonwealth funds aged care, it does not run the services. "As the document makes clear, residential care facilities have primary responsibility for the management of their - their service."
Now, this document says services should plan for a workforce shortage of 20 to 30 per cent. Remember, Newmarch lost 84% of its workforce. Other homes lost 100% of their employees in 48 hours. Rozen asks Murphy: where did your figure come from? What informed that?
Murphy doesn& #39;t know where the figure came from. "I& #39;d have to take advice on that," he says. Lye counters, saying it was only an absentee rate estimate and providers shouldn& #39;t have to assume they& #39;d lose their entire workforce which is why the Commonwealth provided surge. Helpful!
Janet Anderson& #39;s Aged Care Quality and Safety Commission used the same figures in the self-assessment survey conducted with nursing home providers. And where did that figure come from, she is asked. From the CDNA guidelines. Time is a flat circle.
Some argy bargy just then. Assuming the fed govt was so magnanimous as to assume providers shouldn& #39;t have to cover the absence of their entire workforce, when did surge planning start? Before outbreak at Dorothy Henderson Lodge, says Murphy. But contracts came after.
I find it reaaaalllllllly hard to believe that the reason the fed govt guidelines only referenced a 20 to 30% loss of aged care workforce in an outbreak was because they intended to cover the gap of anything above that. Personally, I think they are back pedalling super hard.
Now Murphy is saying, well actually, if you look across all facilities on average the 20 to 30% figure might actually be accurate. Which one is it buddy? An absentee estimate or a loss of workforce estimate?
Rozen QC tears into Michael Lye. "This is not an opportunity for you to make speeches," he says. Stick to the question.
Reminder: Morrison said in relation to St Basil& #39;s "we couldn& #39;t contemplate an entire workforce going" prior to that. Well, not only had it already happened twice in NSW but now his officials are saying on oath that they not only contemplated it but it was the plan all along?
They had some technical issues and I had to have a smoke. That was wild.
We are back. So, get this, even though the first TWO guideline versions produced by CDNA didn& #39;t bother to update the 20 to 30% estimate figure (both after the NSW outbreaks) a separate document produced on June 29 advised providers to prepare for loss of 80 to 100% of staff.
So this really torpedoes the earlier testimony from Lye and Murphy that they didn& #39;t need to update the 20 to 30% figure because the commonwealth planned on meeting any shortfall.
Asked if he sees any conflict between the documents, Lye says: "No I don& #39;t, counsel."
Janet Anderson now being asked why her Commission didn& #39;t alert the federal Department of Health when they found out via phone call that St Basil& #39;s in Victoria had an outbreak on July 10. It would be four days before that info made it to the commonwealth again.
"We are not a first responder," she says. But she concedes "in hindsight" it might have been the right thing for the staff member in her agency to let someone know. They now have an arrangement to make that a matter of routine "notwithstanding that is not our principal role." Hmm
Rozen asks again whether there is a "sufficient degree of curiosity" in the regulator& #39;s approach to doing its job "beyond just ticking boxes on a list."
Anderson: "We don& #39;t tick boxes, counsel."
Anderson: "We don& #39;t tick boxes, counsel."
Anderson is asked about the results of the "self assessment survey" with aged care providers. "Overall there did seem to be a large degree of confidence that providers were ready in the event of
a pandemic," she says. And Rozen asks, you were surprised by that? She wasn& #39;t.
a pandemic," she says. And Rozen asks, you were surprised by that? She wasn& #39;t.
Now why wouldn& #39;t that raise an eyebrow? More than 40 per cent of all providers rated themselves as "best practice" in this survey. One of those who did was Newmarch House. The regulator didn& #39;t blink an eye.
Now Anderson says: "We have become more questioning and we have deployed a number of additional regulatory activities in order to both prompt activity or action by providers."
Dr Wroth from the regulator is now being asked about notes which appear to show she and a colleague were "strongly recommending" Newmarch House residents be transferred to hospital during the outbreak. She says it wasn& #39;t specifically about removing them from Newmarch.
But then she concedes. "I was advocating that (hospital transfer) as one of the potential options, to protect people, yes."
Counsel is asking Lye about how this dispute between C& #39;wlth and NSW Health officials with regard to moving residents into hospital was resolved. Senator Colbeck was told, and appeared concerned, but the NSW position "held sway", Rozen says.
Now, in the wake of Newmarch, a protocol was developed between Commonwealth and NSW Health about what to do in the event of a serious outbreak in an aged care home. Rozen asks, was one developed with Victoria? There is a "similar process", Lye says.
Rozen isn& #39;t having it. He& #39;s after a document. He asks if Lye can "point us to a document that sets out the relationships, protocol?"
Spoiler alert: there isn& #39;t one.
Spoiler alert: there isn& #39;t one.
Now, the surge workforce. The $6m question. "What had you done when you entered into the contract with Mable to ensure that the workers they were providing would be such that could provide a quality response in such an important role?"
It cost $640,000 alone for the surge workforce at Newmarch House. Anglicare said in the beginning the workers they were provided via Mable were simply not up to the job.
"I repeat my question, is the taxpayer getting value for money in the Commonwealth spending money on Mable as the surge workforce," Rozen asks.
Lye says he believes they are now. But also, after initially contracting Mable as the sole provider of a surge workforce in aged care, Lye says they have now broadened this out to a "range of agencies."
Rozen now asking about decision to make masks compulsory in Victorian aged care homes for healthcare workers. This happened on July 13. Community transmission had been creeping in the state since June. By July 11 there were four active cases in nursing homes.
Prof. Murphy says in hindsight decision "could have have been implemented earlier, absolutely."
Rozen: "The implementation of it earlier may well have reduced the number of infections entering homes, mightn& #39;t it?"
Murphy: "That& #39;s speculation counsel but it& #39;s possible, yes."
Rozen: "The implementation of it earlier may well have reduced the number of infections entering homes, mightn& #39;t it?"
Murphy: "That& #39;s speculation counsel but it& #39;s possible, yes."
I’m going to have to tap out of the #agedcareRC here as I have to finish writing this other piece and I’m going on @ABCthedrum to talk about this and other things. See you there!
Before today’s hearing gets underway, I just want to place this extraordinary moment from yday on the timeline. Brendan Murphy, now Health secretary, tries to whisper an answer to his deputy in front of a mic, gets caught, acts surprised then stares blankly into space.
OK, so senior counsel Peter Rozen is making submissions to the #agedcareRC. After this week& #39;s evidence he says "we will be submitting that it was not well prepared."
"Because the risk of an outbreak of COVID-19 in an aged care home is
extremely high, even with low rates of community transmission there
needed to be a planned proportionate response to protect the elderly frail in the nursing homes." There wasn& #39;t.
extremely high, even with low rates of community transmission there
needed to be a planned proportionate response to protect the elderly frail in the nursing homes." There wasn& #39;t.
"None of the problems that have been associated with the response of the aged care sector to Covid-19 were unforeseeable." None of them.
Rozen is referring back to SA& #39;s chief health officer Professor Nicola Spurrier and the principles that underpin public health. "The principle is enshrined in the public health legislation of the states and territories," he says. This is key re: hospital transfers issue.
"The approach is concerned as much with the clinical needs of the resident as it is with what Professor McLaws described as the negative residents& #39; right to remain negative." That is the crux of the hospital issue. Negative residents have the ~right~ to be kept safe from Covid-19
Rozen now makes the point that while the fed govt& #39;s overarching emergency response plan for the health sector, a 56 page document, mentions aged care but does not detail what to do. "It is a plan, it& #39;s just not an aged care plan," Rozen says.
The above plan was February. The next one, which purports to deal specifically with aged care from the CDNA, was released on March 13. This, Rozen notes, was adapted from an existing plan for responses to influenza outbreaks in nursing homes.
"This derivation of the document may partly explain why some aged care
providers may have thought that their existing influenza plans would hold them in good stead for COVID-19 only to find that they left them woefully unprepared," Rozen says.
providers may have thought that their existing influenza plans would hold them in good stead for COVID-19 only to find that they left them woefully unprepared," Rozen says.
"Remarkably the first two versions (of the CDNA doc) made no mention of the Federal Government having a role in the system, that it funds to the total exclusion of the states," Rozen says. Bingo.
Now after Newmarch House and Dorothy Henderson Lodge outbreaks, the commonwealth developed a joint protocol with the NSW state government about what to do in event of an outbreak. No such protocol exists with any other state.
Regarding the above specifically, Rozen says: "It is unacceptable that such arrangements were not in place in February. It& #39;s unforgiveable that they are not in place in August. The virus is not a fair fighter. It doesn& #39;t wait until the bell rings."
On June 26, the royal commission asked the aged care quality and safety commission to supply "any pandemic plan" or "risk-based framework" for dealing with Covid-19 in the sector. One of them is a widely availably risk pyramid. You can Google it.
"Whatever else may be said about the documents they are not the comprehensive plan of a regulator facing the COVID-19 pandemic," Rozen says.
Rozen notes that a credentialed infectious control expert was on the ground at Dorothy Henderson Lodge on Day 1. This made an enormous difference to containing the outbreak. There are 66 such experts across Australia.
Rozen asks the obvious question: why the hell didn& #39;t the commonwealth use them? "To be blunt, what could be more important to the nation right now than to deploy these experts to help our floundering aged care sector respond to this pandemic?"
"Commissioners, there is reason to think that in the crucial months between the Newmarch House outbreak in April and mid June a degree
of self-congratulation and even hubris was displayed by the Commonwealth." Ouch. True.
of self-congratulation and even hubris was displayed by the Commonwealth." Ouch. True.
"Perhaps, Commissioners, that is the ultimate lesson. When it comes to the health and safety of our residents in nursing homes we can& #39;t afford to take any risks at all," Rozen says. And with that, his oral submissions are finished.
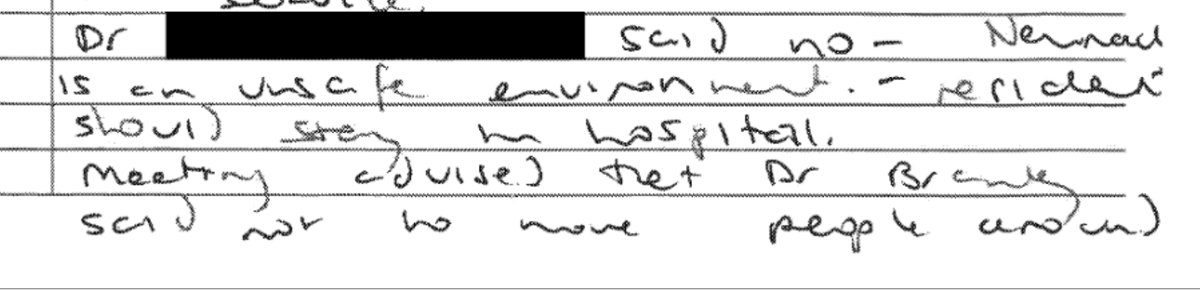
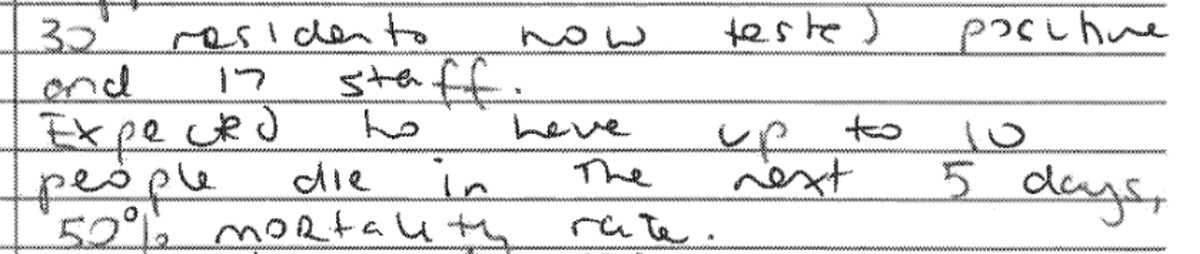
I& #39;m just going through the rest of the tendered evidence at #agedcareRC I didn& #39;t get time to read this week and this is chilling. On April 20 the aged care regulator& #39;s general manager Anne Wunsch made these notes about Newmarch House situation.
Keep in mind, at least 3 residents had already died. The rest were being forced into "hospital in the home". One was in actual hospital and discussion turned to whether they should "remain in hospital or return to service." One doctor said no. "Newmarch is an unsafe environment."
Three days later, she notes this terrifying stat. And on the SAME day, almost two weeks into the outbreak, they start using N95 masks instead of basic surgical masks. Gowns still being rationed.

 Read on Twitter
Read on Twitter