My thread in response to an article in The Conversation. https://theconversation.com/ppe-unmasked-why-health-care-workers-in-australia-are-inadequately-protected-against-coronavirus-143751
There">https://theconversation.com/ppe-unmas... are a few things that need to be teased out a little.
There">https://theconversation.com/ppe-unmas... are a few things that need to be teased out a little.
2. First off, I agree we need to protect HCWs and patients, no question. That is the foundation of all infection prevention and control work and all those involved in this field in Aus and the globe. Personally, I have no fixed view, on any infection control matter.
3. We need clear, transparent information on how HCWs acquired COVID-19 - to inform evidence & guidelines, as well as a reassurance if changes to guidance are not required.
4. Publication bias of HCWs acquisition of any infectious disease is a major issue. More likely to report & #39;negative& #39; findings in peer reviewed journals. We need to know when things are working as well. Remembering the millions of episodes of care that are delivered safely
5. Many factors are at play re HCWs acquiring COVID-19, community acquisition, donning/doffing, training, and potentially the type of PPE used. These need to be explored thoroughly.
6. The outbreak in NW regional hospital in Tasmania involving HCWs was largely thought to be contact with other HCWs, unwell staff, physical distancing etc. https://www.health.tas.gov.au/__data/assets/pdf_file/0006/401010/North_West_Regional_Hospital_Outbreak_-_Interim_Report.pdf">https://www.health.tas.gov.au/__data/as...
7. Studies overseas have many reasons for HCWs acquiring COVID-19
https://www.nejm.org/doi/full/10.1056/NEJMc2005696
https://www.nejm.org/doi/full/... href=" https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7118342/
https://www.ncbi.nlm.nih.gov/pmc/artic... href=" https://www.medrxiv.org/content/10.1101/2020.03.23.20041913v3">https://www.medrxiv.org/content/1... (non peer reviewed)
https://www.nejm.org/doi/full/10.1056/NEJMc2005696
8. We can all find individual cases to make a point, we need to consider the totality of evidence as it stands - meaning more transparent information about HCW acquisitions.
9. The authors present droplet vs airborne as a dichotomy. In infection control, we know such dichotomy does not exists, it is there purely for practical reasons. Droplet to airborne is more of a continuum. See by some leading US experts http://haicontroversies.blogspot.com/2020/07/a-tiresome-spat.html">https://haicontroversies.blogspot.com/2020/07/a...
10. The MJA article referenced is not peer reviewed and is subject to a response by infection control experts in QLD, alongside another recent article https://clinicalexcellence.qld.gov.au/sites/default/files/docs/clinical-networks/sicn-covid-19-transmission-ps.pdf">https://clinicalexcellence.qld.gov.au/sites/def... and here https://jamanetwork.com/journals/jama/fullarticle/2768396">https://jamanetwork.com/journals/...
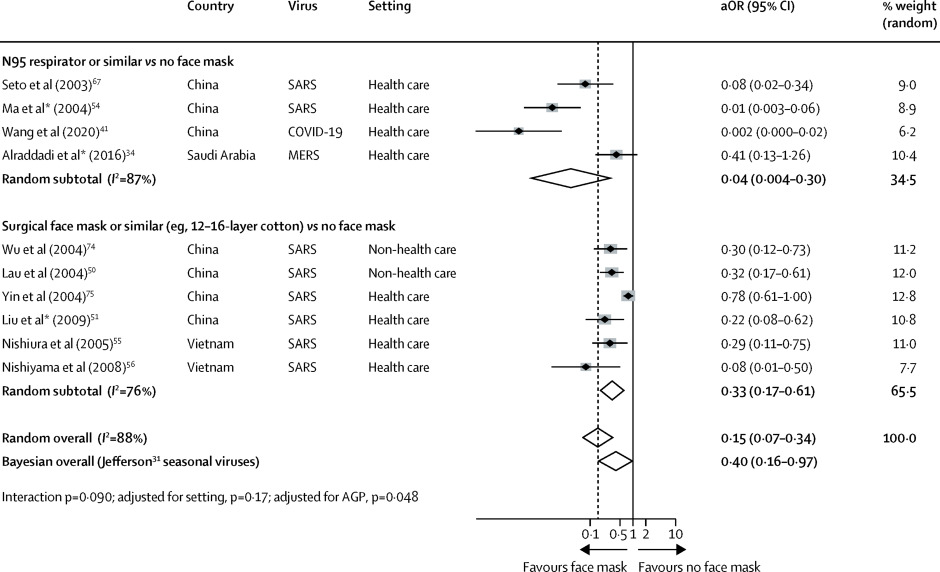
11. A systematic review was cited to claim N95 are superior to surgical masks. This is logical given the higher filtration, but is different to assessing clinical outcomes (infection). Figure 4 in the article compares N95 to no mask and surgical to no mask. (not N95 Vs surgical)
12. AHPPC receives advice from CDNA, PHLN & ICEG, among others, in making decisions. Each jurisdiction has a CHO on AHHPC who seek advice from their own jurisdiction. Maybe such advice is therefore based on experts from many fields, across the country. https://www.health.gov.au/committees-and-groups/australian-health-protection-principal-committee-ahppc">https://www.health.gov.au/committee...
13. Local epidemiology may play an important part. Local modifications to PPE requirements in the context of epidemiology and models of care are sensible. They should not be used as evidence of a & #39;controversy& #39;
14. There are often practical reasons for N95 masks use (over & above airborne debate) - e.g. prolonged use to reduce mask doffing associated risks; areas / ward with many COVID-19 patients. Again, not to be mixed with other issues.

 Read on Twitter
Read on Twitter