LICHEN PLANUS
A #dermtwitter, #medtwitter, and #medstudenttwitter #tweetorial! PC: @dermnetnz. Let& #39;s kick off this #MedEd #FOAMEd #medthread with a question.
With LP, which one of the following body sites is most commonly involved?
1/
A #dermtwitter, #medtwitter, and #medstudenttwitter #tweetorial! PC: @dermnetnz. Let& #39;s kick off this #MedEd #FOAMEd #medthread with a question.
With LP, which one of the following body sites is most commonly involved?
1/
The correct answer is wrists! LP lesions are most commonly seen on flexor wrists, trunk, medial thighs, and shins. It very rarely involves the face.
The mnemonic for the clinical appearance of LP is to remember the "Ps."
Pruritic (!!!)
Purple
Polygonal/Planar
Papules
2/
The mnemonic for the clinical appearance of LP is to remember the "Ps."
Pruritic (!!!)
Purple
Polygonal/Planar
Papules
2/
You can also make out white and gray lacy streaks and puncta. This is called "Wickham Striae" which helps confirm the diagnosis (1).
Notably, LP also can go to the oropharynx, which can cause erosive lesions that are painful. Wickham Striae are easier to see in the mouth (2).
3/
Notably, LP also can go to the oropharynx, which can cause erosive lesions that are painful. Wickham Striae are easier to see in the mouth (2).
3/
Remember that all inflammatory skin conditions can appear different in skin of color. LP tends to affect POC more, so this is critical!
In pic 1, we see hypertrophic LP on darker skin on the shin. Notice that the erythema is much more muted when compared with whiter skin (2).
4/
In pic 1, we see hypertrophic LP on darker skin on the shin. Notice that the erythema is much more muted when compared with whiter skin (2).
4/
Other than the mouth, LP can also affect other mucosal sites (eg: groin). This can lead to erosions and scarring, so it& #39;s important to treat aggressively.
The nails can be involved as well leading to painful scarring, nail splitting, and all 20 nails can be affected!
5/
The nails can be involved as well leading to painful scarring, nail splitting, and all 20 nails can be affected!
5/
Finally, one more subtype to discuss. Lichen planus pigmentosus is a form of dyspigmentation that commonly affects the face (but can involve the torso & extremities). It can be cosmetically distressing, & more commonly affects skin of color.
This is really difficult to treat!
6/
This is really difficult to treat!
6/
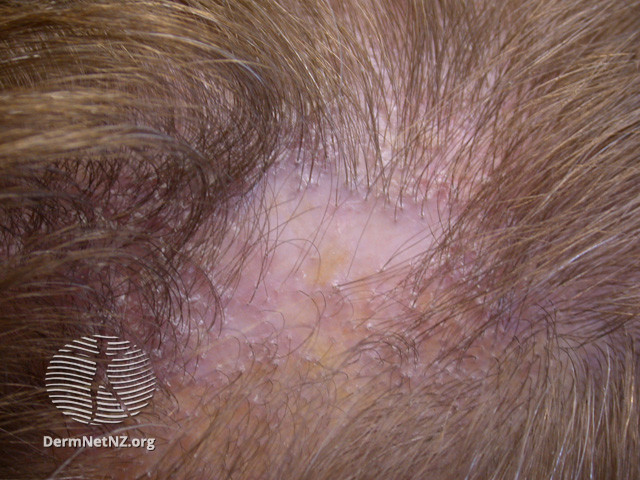
A little more peripherally associated, lichen planopilaris is involvement of the scalp leading to a scarring alopecia. Classic findings include loss of follicular ostia, peri-follicular erythema & scaling.
This can be associated with regular LP and a non-scarring alopecia!
7/
This can be associated with regular LP and a non-scarring alopecia!
7/
So while there are so many subtypes of LP, they all fall into this bucket of "lichenoid" processes because of the #dermatopathology that is seen on biopsy.
While classic LP doesn& #39;t require a biopsy, atypical cases benefit from CPC.
What would you expect to see on histology?
8/
While classic LP doesn& #39;t require a biopsy, atypical cases benefit from CPC.
What would you expect to see on histology?
8/
The path finding is the band-like lymphocytic infiltrate in the upper dermis. There are a lot of nuances to this with subtypes, but whenever we say "lichen," that& #39;s what we expect to see.
Tagging our favorite #dermpath @ilanarosman if she feels compelled to add some detail https://abs.twimg.com/emoji/v2/... draggable="false" alt="😉" title="Zwinkerndes Gesicht" aria-label="Emoji: Zwinkerndes Gesicht">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="😉" title="Zwinkerndes Gesicht" aria-label="Emoji: Zwinkerndes Gesicht">
9/
Tagging our favorite #dermpath @ilanarosman if she feels compelled to add some detail
9/
Before we talk treatment, let& #39;s talk associations. LP has been associated with a variety of processes so it& #39;s important to think about this, especially in cases where LP arose de novo!
Think about:
Hepatitis C infection
Hepatitis B vaccine
Primary Biliary Cirrhosis
10/
Think about:
Hepatitis C infection
Hepatitis B vaccine
Primary Biliary Cirrhosis
10/
Also, reminder that LP can koebnerize. Remember that koebner phemonemon is where epidermal injury (usually scratching) can cause the underlying inflammatory disease to occur in traumatized skin.
This leads to linear LP!
11/
This leads to linear LP!
11/
So let& #39;s talk treatment. If you& #39;re not a #dermatologist, topical steroids are helpful.
LP is traditionally VERY itchy, so you may want to start with a Class 1 steroid (but not on the face!). Check out my #tweetorial on topical steroids for help. https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Rückhand Zeigefinger nach unten" aria-label="Emoji: Rückhand Zeigefinger nach unten">
https://twitter.com/DrStevenTChen/status/1123605778127052800?s=20
12/">https://twitter.com/DrStevenT...
LP is traditionally VERY itchy, so you may want to start with a Class 1 steroid (but not on the face!). Check out my #tweetorial on topical steroids for help.
https://twitter.com/DrStevenTChen/status/1123605778127052800?s=20
12/">https://twitter.com/DrStevenT...
For the #dermatology crowd, I personally have found LP can be very stubborn to treat. I have tried prednisone, mycophenolate, cyclosporine, and methotrexate. Phototherapy can help, as can systemic retinoids and metronidazole (article!).
https://www.jaad.org/article/S0190-9622(00)99923-7/fulltext
13/">https://www.jaad.org/article/S...
https://www.jaad.org/article/S0190-9622(00)99923-7/fulltext
13/">https://www.jaad.org/article/S...
RECAP
- LP is an inflammatory condition that can go beyond the skin to mucosa, scalp, nails, & can cause pigmentary issues!
- Treatment can be difficult, but starting with topical steroids is good.
- Don& #39;t forget to investigate possible associations!
Hope this was helpful!
14/14
- LP is an inflammatory condition that can go beyond the skin to mucosa, scalp, nails, & can cause pigmentary issues!
- Treatment can be difficult, but starting with topical steroids is good.
- Don& #39;t forget to investigate possible associations!
Hope this was helpful!
14/14

 Read on Twitter
Read on Twitter







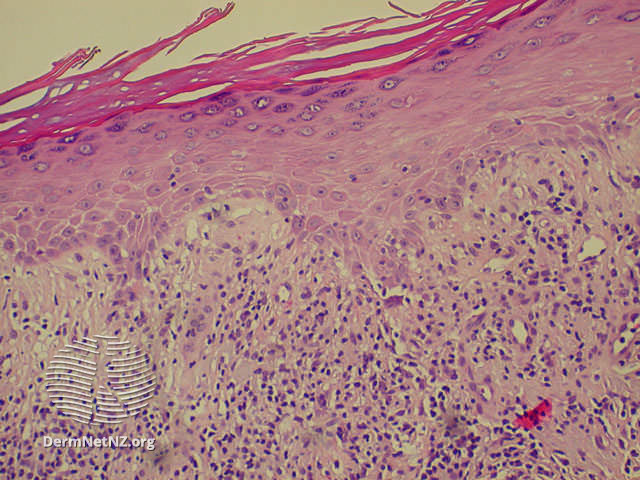 9/" title="The path finding is the band-like lymphocytic infiltrate in the upper dermis. There are a lot of nuances to this with subtypes, but whenever we say "lichen," that& #39;s what we expect to see.Tagging our favorite #dermpath @ilanarosman if she feels compelled to add some detailhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="😉" title="Zwinkerndes Gesicht" aria-label="Emoji: Zwinkerndes Gesicht">9/" class="img-responsive" style="max-width:100%;"/>
9/" title="The path finding is the band-like lymphocytic infiltrate in the upper dermis. There are a lot of nuances to this with subtypes, but whenever we say "lichen," that& #39;s what we expect to see.Tagging our favorite #dermpath @ilanarosman if she feels compelled to add some detailhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="😉" title="Zwinkerndes Gesicht" aria-label="Emoji: Zwinkerndes Gesicht">9/" class="img-responsive" style="max-width:100%;"/>



